Abstract
Background
Postoperative delirium is common in older patients after spinal surgery. Many reports investigating the risk factors for delirium after spinal surgery have been published recently.
Methods
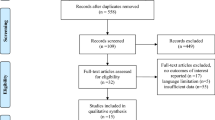
A literature search was performed using the Cochrane Library, Web of Science, PubMed, Embase, and Springer databases from inception to February 2019. Relevant studies involving patients with delirium who underwent spinal surgery were included if the studies contained data about blood transfusion or other related factors, such as haemoglobin, haematocrit, and blood loss levels. The Newcastle–Ottawa Scale was used for the study-quality evaluation. The pooled odds ratios or (standard) mean differences of the individual risk factors were estimated using the Mantel–Haenszel or inverse-variance methods.
Results
Fifteen observational studies met the inclusion criteria; the studies included a total of 583,290 patients (5431 patients with delirium and 577,859 patients without delirium). In addition to an advanced age, the results of the meta-analyses showed that living in an institution, diabetes, cerebral vascular diseases, pulmonary diseases, opioid use, length of surgery, intraoperative blood loss, blood transfusions, intraoperative infusion, preoperative albumin, postoperative albumin, preoperative haematocrit, postoperative haematocrit, preoperative haemoglobin, postoperative haemoglobin, preoperative sodium, postoperative sodium, Mini-Mental State Examination score, inability to ambulate, depression, number of medications, and treatment with multiple drugs (> three types) were significantly associated with delirium.
Conclusion
The above-mentioned risk factors can be used to identify high-risk patients, and the appropriate prophylaxis strategies should be implemented to prevent delirium after spinal surgery.
















Similar content being viewed by others
References
Leslie DL, Marcantonio ER, Zhang Y et al (2008) One-year health care costs associated with delirium in the older population. Arch Intern Med 168:27–32
Witlox J, Eurelings LS, de Jonghe JF et al (2010) Delirium in older patients and the risk of postdischarge mortality, institutionalization, and dementia: a meta-analysis. JAMA 304:443–451
Akunne A, Murthy L, Young J (2012) Cost-effectiveness of multi-component interventions to prevent delirium in older people admitted to medical wards. Age Ageing 41:285–291
Galanakis P, Bickel H, Gradinger R et al (2001) Acute confusional state in the older following hip surgery: Incidence, risk factors and complications. Int J Geriatr Psychiatry 16:349–355
Inouye SK, van Dyck CH, Alessi CA et al (1990) Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med 113:941–948
Trzepacz PT, Mittal D, Torres R et al (2001) Validation of the Delirium Rating Scale-revised-98: comparison with the delirium rating scale and the cognitive test for delirium. J Neuropsychiatry Clin Neurosci 13:229–242
Fong T, Tulebaev S, Inouye S (2009) Delirium in older adults: diagnosis, prevention and treatment. Nat Rev Neurol 5:210–220
Fineberg SJ, Nandyala SV, Oglesby M et al (2013) Incidence and risk factors for post-operative delirium following lumbar spine surgery. Spine 38:1790–1796
Ahmed S, Leurent B, Sampson EL (2014) Risk factors for incident delirium among older people in acute hospital medical units: a systematic review and meta-analysis. Age Ageing 43:326–333
Shi C, Yang C, Gao R et al (2015) Risk factors for delirium after spinal surgery: a meta-analysis. World Neurosurg 84:1466–1472
Higgins JPT, Altman DG (eds) (2008) Cochrane handbook for systematic reviews of interventions. Version 5.0.1. The Cochrane Collaboration
Harris JD, Quatman CE, Manring MM et al (2014) How to write a systematic review. Am J Sports Med 42:2761–2768
Wan X, Wang W, Liu J et al (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14:135
Wells GA, Shea B, O’Connell D et al (2011) The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/. Accessed 10 Mar 2019
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50:1088–1101
Egger M, David SG, Schneider M et al (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Kawaguchi Y et al (2006) Postoperative delirium in spine surgery. Spine 6:164–169
Gao R, Yang ZZ, Li M (2008) Probable risk factors for postoperative delirium in patients undergoing spinal surgery. Eur Spine J 17:1531–1537
Lee JK, Park YS (2010) Delirium after spinal surgery in Korean population. Spine (Phila Pa 1976) 35:1729–1732
Soh S, Shim JK, Song JW et al (2017) Postoperative delirium in older patients undergoing major spinal surgery: role of cerebral oximetry. J Neurosurg Anesthesiol 29:426–432
Jiang X, Chen D, Lou Y et al (2017) Risk factors for postoperative delirium after spine surgery in middle- and old-aged patients. Aging Clin Exp Res 29:1039–1044
Brown CH, LaFlam A, Max L et al (2016) Delirium after spine surgery in older adults: incidence, risk factors, and outcomes. J Am Geriatr Soc 64:2101–2108
Seo JS, Park SW, Lee YS et al (2014) Risk factors for delirium after spine surgery in older patients. J Korean Neurosurg Soc 56:28–33
Oe S, Togawa D, Yamato Y et al (2018) Preoperative age and prognostic nutritional index are useful factors for evaluating postoperative delirium among patients with adult spinal deformity. Spine (Phila Pa 1976) 44:472–478
Morino T, Hino M, Yamaoka S et al (2018) Risk factors for delirium after spine surgery: an age-matched analysis. Asian Spine 12:703–709
Kim KH, Kang SY, Shin DA et al (2018) Parkinson’s disease-related non-motor features as risk factors for post-operative delirium in spinal surgery. PLoS ONE 13:e0195749
Kobayashi K, Imagama S, Ando K et al (2017) Risk factors for delirium after spine surgery in extremely elderly patients aged 80 years or older and review of the literature: Japan Association of Spine Surgeons with Ambition Multicenter Study. Glob Spine J 7:560–566
Li H, Li CD, Yi XD et al (2012) Analysis of risk factors for delirium in the older patients after spinal operation. Beijing Da Xue Xue Bao 44:847–850
Susano MJ, Scheetz SD, Grasfield RH et al (2018) Retrospective analysis of perioperative variables associated with postoperative delirium and other adverse outcomes in older patients after spine surgery. J Neurosurg Anesthesiol. https://doi.org/10.1097/ANA.0000000000000566
Fineberg SJ, Nandyala SV, Marquez-Lara A et al (2013) Incidence and risk factors for postoperative delirium after lumbar spine surgery. Spine (Phila Pa 1976) 38:1790–1796
Elsamadicy AA, Adogwa O, Lydon E et al (2017) Depression as an independent predictor of postoperative delirium in spine deformity patients undergoing elective spine surgery. J Neurosurg Spine 27:209–214
Kuhn E, Du X, McGrath K et al (2014) Validation of a consensus method for identifying delirium from hospital records. PLoS ONE 9:e111823
Chen XW, Shi JW, Yang PS et al (2014) Preoperative plasma leptin levels predict delirium in older patients after hip fracture surgery. Peptides 57:31–35
Wu D, Hao H, Zhu J et al (2015) Risk factors analysis for postoperative delirium of older hip fracture patients. Chin J Geriatr Orthop Rehabil 1:34–38
Miyagawa Y, Yokoyama Y, Fukuzawa S et al (2017) Risk factors for postoperative delirium in abdominal surgery: a proposal of a postoperative delirium risk score in abdominal surgery. Dig Surg 34:95–102
Ushida T, Yokoyama T, Kishida Y et al (2009) Incidence and risk factors of postoperative delirium in cervical spine surgery. Spine (Phila Pa 1976) 34:2500–2504
Densky J, Eskander A, Kang S et al (2019) Risk factors associated with postoperative delirium in patients undergoing head and neck free flap reconstruction. JAMA Otolaryngol Head Neck Surg. https://doi.org/10.1001/jamaoto.2018.3820
Oh ES, Sieber FE, Leoutsakos JM et al (2016) Sex differences in hip fracture surgery: preoperative risk factors for delirium and postoperative outcomes. J Am Geriatr Soc 64:1616–1621
Tahir M, Malik SS, Ahmed U et al (2018) Risk factors for onset of delirium after neck of femur fracture surgery: a prospective observational study. SICOT J 4:27. https://doi.org/10.1051/sicotj/2018018
Cukierman T, Gerstein HC, Williamson JD (2005) Cognitive decline and dementia in diabetes—systematic overview of prospective observational studies. Diabetologia 48:2460–2469
Wang H, Anthony D, Selemidis S et al (2018) Resolving viral-induced secondary bacterial infection in COPD: a concise review. Front Immunol 9:2345
Kalvas LB, Monroe TB (2019) Structural brain changes in delirium: an integrative review. Biol Res Nurs 8:1099800419849489
Kim H, Chung S, Joo YH et al (2016) The major risk factors for delirium in a clinical setting. Neuropsychiatric Dis Treat 12:1787–1793
Caza N, Taha R, Qi Y et al (2008) The effects of surgery and anesthesia on memory and cognition. Prog Brain Res 169:409–422
Whitlock EL, Behrends M (2015) Blood transfusion and postoperative delirium. Curr Anesthesiol Rep 5:24–32
van der Zanden V, Beishuizen SJ, Swart LM et al (2017) The effect of treatment of anemia with blood transfusion on delirium: a systematic review. J Am Geriatr Soc 65:728–737
Wang LH, Xu DJ, Wei XJ et al (2016) Electrolyte disorders and aging: risk factors for delirium in patients undergoing orthopedic surgeries. BMC Psychiatry 16:418
Shiiba M, Takei M, Nakatsuru M et al (2009) Clinical observations of postoperative delirium after surgery for oral carcinoma. Int J Oral Maxillofac Surg 38:661–665
Miyagawa Y, Yokoyama Y, Fukuzawa S et al (2017) Risk factors for postoperative delirium in abdominal surgery: a proposal of a postoperative delirium risk score in abdominal surgery. Dig Surg 34:95–102
Wang LH, Xu DJ, Wei XJ et al (2016) Electrolyte disorders and aging: risk factors for delirium in patients undergoing orthopedic surgeries. BMC Psychiatry 16:418
Wu Y, Shi Z, Wang M et al (2015) Different MMSE Score is associated with postoperative delirium in young-old and old-old adults. PLoS ONE 10:e0139879
Heirene R, John B, Roderique-Davies G (2018) Identification and evaluation of neuropsychological tools used in the assessment of alcohol-related cognitive impairment: a systematic review. Front Psychol 9:2618
Yang J, Zhou Y, Kang Y et al (2017) Risk factors of delirium in sequential sedation patients in intensive care unit. Biomed Res Int 2017:3539872
Nelson S, Rustad JK, Catalano G et al (2016) Depressive symptoms before, during, and after delirium: a literature review. Psychosomatics 57:131–141
Nie H, Zhao B, Zhang YQ et al (2012) Pain and cognitive dysfunction are the risk factors of delirium in older hip fracture Chinese patients. Arch Gerontol Geriatr 54:e172–e174
Wood PB, Schweinhardt P, Jaeger E et al (2007) Fibromyalgia patients show an abnormal dopamine response to pain. Eur J Neurosci 25:3576–3582
Thompson C, Brienza VJM, Sandre A et al (2018) Risk factors associated with acute in-hospital delirium for patients diagnosed with a hip fracture in the emergency department. CJEM 20:911–919
Steidl S, Wasserman DI, Blaha CD et al (2018) Opioid-induced rewards, locomotion, and dopamine activation: a proposed model for control by mesopontine and rostromedial tegmental neurons. Neurosci Biobehav Rev 83:72–82
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhu, C., Wang, B., Yin, J. et al. Risk factors for postoperative delirium after spinal surgery: a systematic review and meta-analysis. Aging Clin Exp Res 32, 1417–1434 (2020). https://doi.org/10.1007/s40520-019-01319-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-019-01319-y