Abstract
Purpose
To compare prevalence of self-reported diabetes between U.S. state-born, Puerto Rico-born, Mexico-born, Cuba-born, and South/Central America-born Hispanic groups, and examine whether risk for diabetes differs by country of origin and experiences with discrimination when accounting for BMI.
Methods
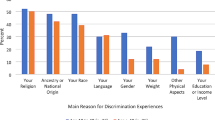
Data from 6223 Hispanic respondents from the nationally representative NESARC-III study was used. Sociodemographic characteristics were compared across nativity groups, and adjusted odds of self-reported diabetes diagnosis (past year) tested. Differences by perceived discrimination (using endorsement of individual items assessing specific experiences) and by nativity were examined when accounting for sociodemographic characteristics, acculturation, and BMI.
Results
Prevalence of self-reported diabetes diagnosis was significantly higher among the Puerto Rico-born Hispanics, and remained significantly elevated when adjusting for perceived discrimination, acculturation, and health risk behaviors. When adjusting further for BMI, there were no significant differences in the odds of diabetes by nativity. Prevalence of lifetime perceived discrimination was significantly lower among Cuba-born Hispanics. Mean BMI was significantly lower in South/Central America-born Hispanic individuals relative to U.S. state-, Mexico-, and Puerto Rico-born Hispanic groups. Higher BMI was associated with significantly greater risk of diabetes diagnosis across groups.
Conclusion
Marked heterogeneity exists in prevalence and in factors associated with diabetes risk and weight status across Hispanic groups in the U.S. Experiences with discrimination may play an important role in accounting for these differences. This should be considered when planning future research to inform the most optimal patient-centered prevention efforts.
Level of evidence
Level III, Evidence obtained from well-designed cohort analytic study.
Similar content being viewed by others
Data availability statement
The data that support the findings of this study are available from the National Institute on Alcohol Abuse and Alcoholism (NIAAA). Restrictions apply to the availability of these data, which were used under license for this study. Data are available at https://www.niaaa.nih.gov/research/nesarc-iii/nesarc-iii-data-access with the permission of NIAAA. The NESARC-III Codebook with all individual items asked of respondents is also available: https://www.niaaa.nih.gov/research/nesarc-iii/general-codebook.
References
American Diabetes Association (2018) Economic costs of diabetes in the U.S. in 2017. Diabetes Care 41:917
Nathan DM et al (2009) Modern-day clinical course of type 1 diabetes mellitus after 30 years’ duration: the diabetes control and complications trial/epidemiology of diabetes interventions and complications and Pittsburgh epidemiology of diabetes complications experience (1983–2005). Arch Intern Med 169:1307–1316
Centers for Disease Control and Prevention (2017) National diabetes statistics report, 2017. U.S. Dept of Health and Human Services: Atlanta, GA.
World Health Organization (2018) Diabetes. https://www.who.int/news-room/fact-sheets/detail/diabetes.
Riddle MC, Herman WH (2018) The cost of diabetes care—An elephant in the room. Diabetes Care 41:929. https://doi.org/10.2337/dci18-0012
Bommer C et al (2018) Global economic burden of diabetes in adults: projections from 2015 to 2030. Diabetes Care 41:963. https://doi.org/10.2337/dc17-1962
Brondolo E et al (2015) Place of birth effects on self-reported discrimination: variations by type of discrimination. Int J Intercult Relat 49:212–222. https://doi.org/10.1016/j.ijintrel.2015.10.001
Krueger PM, Coleman-Minahan K, Rooks R (2014) Race/ethnicity, nativity and trends in BMI among U.S. adults. Obesity 22:1739–1746. https://doi.org/10.1002/oby.20744
Wen M, Kowaleski-Jones L, Fan JX (2013) Ethnic-immigrant disparities in total and abdominal obesity in the US. Am J Health Behav 37:807–818. https://doi.org/10.5993/AJHB.37.6.10
Menke A et al (2015) Prevalence of and trends in diabetes among adults in the United States, 1988–2012. JAMA 314:1021–1029. https://doi.org/10.1001/jama.2015.10029
Cheng YJ et al (2019) Prevalence of diabetes by race and ethnicity in the United States, 2011–2016. JAMA 322:2389–2398. https://doi.org/10.1001/jama.2019.19365
Schneiderman N et al (2014) Prevalence of diabetes among Hispanics/Latinos from diverse backgrounds: the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Diabetes Care 37:2233. https://doi.org/10.2337/dc13-2939
Casagrande SS et al (2017) Hemoglobin A1c, blood pressure, and LDL-cholesterol control among Hispanic/Latino adults with diabetes: results from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Endocrine Practice 23:1232–1253. https://doi.org/10.4158/ep171765.Or
Casagrande SS et al (2018) Factors associated with undiagnosed diabetes among adults with diabetes: results from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Diabetes Res Clin 146:258–266. https://doi.org/10.1016/j.diabres.2018.11.004
Abraido-Lanza AF et al (2006) Toward a theory-driven model of acculturation in public health research. Am J Public Health 96:1342–1346
Anderson C et al (2016) Acculturation and diabetes risk in the Mexican American Mano a Mano Cohort. Am J Public Health 106:547–549. https://doi.org/10.2105/ajph.2015.303008
Chrisman M et al (2017) Associations between language acculturation, age of immigration, and obesity in the Mexican American Mano A Mano cohort. Obes Res Clin Pract 11:544–557. https://doi.org/10.1016/j.orcp.2017.03.005
O’Brien MJ et al (2014) Acculturation and the prevalence of diabetes in US Latino adults, National health and nutrition examination survey 2007–2010. Prev Chronic Dis 11:E176. https://doi.org/10.5888/pcd11.140142
O’Brien MJ et al (2014) (2014) A qualitative study of acculturation and diabetes risk among urban immigrant Latinas: implications for diabetes prevention efforts. Diabetes Educ 40(5):616–625. https://doi.org/10.1177/0145721714535992
Epstein JA, Botvin GJ, Diaz T (1998) Linguistic acculturation and gender effects on smoking among Hispanic youth. Prev Med 27:583–589. https://doi.org/10.1006/pmed.1998.0329
Flores E et al (2008) Perceived discrimination, perceived stress, and mental and physical health among Mexican-origin adults. His J Behav 30:401–424. https://doi.org/10.1177/0739986308323056
Finch BK et al (2001) The role of discrimination and acculturative stress in the physical health of Mexican-origin adults. His J Behav 23:399–429. https://doi.org/10.1177/0739986301234004
Peek ME et al (2011) Self-reported racial discrimination in health care and diabetes outcomes. Med Care 49:618–625. https://doi.org/10.1097/MLR.0b013e318215d925
Wagner JA et al (2013) Racial discrimination and metabolic control in women with type 2 diabetes. Ethn Dis 23:421–427
Gonzales KL et al (2014) Perceived racial discrimination in health care, completion of standard diabetes services, and diabetes control among a sample of American Indian women. Diabetes Educ 40:747–755. https://doi.org/10.1177/0145721714551422
Whitaker KM et al (2017) Experiences of discrimination and incident type 2 diabetes mellitus: the multi-ethnic study of Atherosclerosis (MESA). Am J Epidemiol 186:445–455. https://doi.org/10.1093/aje/kwx047
Abraído-Lanza AF, Chao MT, Flórez KR (2005) Do healthy behaviors decline with greater acculturation?: implications for the Latino mortality paradox. Soc Sci Med 61:1243–1255. https://doi.org/10.1016/j.socscimed.2005.01.016
Lyles CR et al (2011) Correlates of patient-reported racial/ethnic health care discrimination in the Diabetes Study of Northern California (DISTANCE). J Health Care Poor Underserved 22:211–225. https://doi.org/10.1353/hpu.2011.0033
LeBrón A et al (2017) Correlates of interpersonal ethnoracial discrimination among Latino adults with diabetes: findings from the REACH Detroit Study. J Ethnic Cult Div Social Work 26:48–67. https://doi.org/10.1080/15313204.2016.1263820
Cuevas A, Ortiz K, Ransome Y (2019) The moderating role of race/ethnicity and nativity in the relationship between perceived discrimination and overweight and obesity: results from the National Epidemiologic Survey on alcohol and related conditions. BMC Public Health 19:1458. https://doi.org/10.1186/s12889-019-7811-0
Janevic T et al (2018) The role of obesity in the risk of gestational diabetes among immigrant and U.S.-born women in New York City. Ann Epidemiol 28:242–248. https://doi.org/10.1016/j.annepidem.2018.02.006
Daviglus ML et al (2012) Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. JAMA 308:1775–1784. https://doi.org/10.1001/jama.2012.14517
Grant BF et al. (2014) Sources and accuracy statement: National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III), N.I.o.A.A.a. Alcoholism, Editor. 2014: Rockville, MD. http://www.niaaa.nih.gov/sites/default/files/NESARC_Final_Report_FINAL_1_8_15.pdf
Grant BF et al (2016) Epidemiology of DSM-5 drug use disorder: results from the National Epidemiologic Survey on alcohol and related conditions-III. JAMA Psychiatry 73:39–47. https://doi.org/10.1001/jamapsychiatry.2015.2132
Vásquez E, Murillo R, Echeverria S (2019) Neighborhood social cohesion and walking limitations in ethnically diverse older Latinos in the United States. Ethn Dis 29:247–252
Neo-Bustamante L, Flores A, Shai S. Facts on Hispanics of Puerto Rican origin in the United States, 2017 (2019). Pew Research Center. https://www.pewresearch.org/hispanic/fact-sheet/u-s-hispanics-facts-on-puerto-rican-origin-latinos/
Leong F, Park YS, Kalibatseva Z (2013) Disentangling immigrant status in mental health: psychological protective and risk factors among Latino and Asian American immigrants. Am J Orthopsychiatry 83:361–371
Pérez DJ, Fortuna L, Alegria M (2008) Prevalence and correlates of everyday discrimination among U.S. Latinos J Community Psychol 36:421–433
Krieger N, Smith K, Naishadham D, Hartman C, Barbeau EM (2005) Experiences of discrimination: validity and reliability of a self-report measure for population health research on racism and health. Soc Sci Med 61:1576–1596
Ruan WJ et al (2008) The alcohol use disorder and associated disabilities interview schedule-IV (AUDADIS-IV): reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug Alcohol Depend 92:27–36
Marin G, Gamba R (1996) A new measurement of acculturation for Hispanics: the Bidimensional Acculturation Scale for Hispanics (BAS). His J Behav 18:297–316
U.S. Department of Health and Human Services (2018) Physical activity guidelines for Americans, 2nd edn. U.S. Department of Health and Human Services, Washington, DC
Marascuilo LA, Serlin RC (1988) Statistical methods for the social and behavioral sciences. W. H. Freeman, New York
Sharpe D (2015) Your chi-square test is statistically significant: Now what? Practical Assessment, Research & Evaluation 20
Dendup T et al (2018) Environmental risk factors for developing type 2 diabetes mellitus: a systematic review. Int J Environ Res 15:78. https://doi.org/10.3390/ijerph15010078
Bethel JW, Schenker MB (2005) Acculturation and smoking patterns among Hispanics: a review. Am J Prev Med 29:143–148. https://doi.org/10.1016/j.amepre.2005.04.014
Riosmena F, Wong R, Palloni A (2013) Migration selection, protection, and acculturation in health: a binational perspective on older adults. Demography 50:1039–1064. https://doi.org/10.1007/s13524-012-0178-9
Reynolds MM, Chernenko A, Read J (2016) Region of origin diversity in immigrant health: moving beyond the Mexican case. Soc Sci Med 166:102–109. https://doi.org/10.1016/j.socscimed.2016.07.018
Young-Hyman D et al (2016) Psychosocial care for people with diabetes: a position statement of the American Diabetes Association. Diabetes Care 39:2126. https://doi.org/10.2337/dc16-2053
Hu FB (2011) Globalization of diabetes. Diabetes Care 34:1249. https://doi.org/10.2337/dc11-0442
Zhu Y et al (2019) Racial/ethnic disparities in the prevalence of diabetes and prediabetes by BMI: patient outcomes research to advance learning (PORTAL) multisite cohort of adults in the U.S. Diabetes Care 42:2211. https://doi.org/10.2337/dc19-0532
Acknowledgements
RK contributed to the conceptualization, discussion, writing, and editing of the manuscript. CG contributed to the conceptualization, discussion, writing and editing of the manuscript. EV contributed to the conceptualization, discussion, data analyses, and editing of the manuscript. TU contributed to conceptualization, discussion, data analyses, writing, and editing of the manuscript.
Funding
The article was prepared using a limited access dataset obtained from the National Institute on Alcohol Abuse and Alcoholism. CG was supported, in part, by Grants from the National Institutes of Health (R01 DK114075, R01 DK112771, R01 DK49587). This article does not reflect the opinions or views of the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institute on Alcohol Abuse and Alcoholism, or the United States Government.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Although CG reports no relevant direct or indirect conflicts of interest with respect to this study, he reports having received in the past 12 months honoraria for CME-related lectures and royalties from academic books published by Guilford Press and Taylor & Francis Publishers. RK, EV, and TU have no conflicts of interest to disclose.
Ethical approval
The NESARC-III was approved by the NIH Institutional Review Board (IRB). This study was deemed exempt from IRB review by the University of Albany for use of publicly available de-identified data.
Consent to participate
Respondents provided oral informed consent which was electronically recorded.
Consent for publication
All the co-authors have approved of the manuscript in its current form for submission for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kamody, R.C., Grilo, C.M., Vásquez, E. et al. Diabetes prevalence among diverse Hispanic populations: considering nativity, ethnic discrimination, acculturation, and BMI. Eat Weight Disord 26, 2673–2682 (2021). https://doi.org/10.1007/s40519-021-01138-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-021-01138-z