Abstract
Purpose of the review
Viral respiratory infections have been recognized as a cause of severe illness in immunocompromised and non-immunocompromised hosts. This acknowledgement is a consequence of improvement in diagnosis and better understanding of transmission. Available vaccines and antiviral drugs for prophylaxis and treatment have been developed accordingly. Viral respiratory pathogens are increasingly recognized as nosocomial pathogens as well. The purpose of this review is to describe the most frequent and relevant nosocomial viral respiratory infections, their mechanisms of transmission and the infection control measures to prevent their spread in the healthcare setting.
Recent findings
Although most mechanisms of transmission and control measures of nosocomial viral infections are already known, improved diagnostic tools allow better characterization of these infections and also lead to the discovery of new viruses such as the coronavirus, which is the cause of the Middle East Respiratory Syndrome, or the human bocavirus. Also, the ability to understand better the impact, dissemination and prevention of these viruses, allows us to improve the measures to prevent these infections.
Summary
Healthcare viral respiratory infections increase patient morbidity. Each virus has a different mechanism of transmission; therefore, early detection and prompt implementation of infection control measures are very important in order to avoid their transmission in the hospital setting.
Similar content being viewed by others
Introduction
Healthcare-associated viral infections cause an increase in morbidity and mortality among hospitalized patients and also in healthcare-associated costs. Viral respiratory pathogens are increasingly recognized as etiological agents of nosocomial infections. They can be acquired in different settings inside the hospital and they can produce upper (URI) or lower respiratory tract infections (LRI) [1•]. Transmission can occur by air through aerosolization, by drops of respiratory secretions or by inoculation after touching contaminated surfaces [2].
Among immunocompromised hosts, these types of infections can present themselves with subclinical manifestations and can be associated with high morbidity and mortality. For this reason, a high suspicion vigilance must be kept to confirm viral infections in these hosts. It is also known that viral shedding is more prolonged [3, 4•].
There are several etiological agents that cause these infections, with different ways of transmission depending on each virus. For this reason, it is mandatory to suspect and correctly identify the etiological agent and promptly implement isolation precautions.
Molecular methods have improved sensitivity for the diagnosis of viral infections and have also facilitated the identification of other viral pathogens that cause respiratory tract infections [5].
In the clinical setting, it is sometimes difficult to establish if a respiratory viral infection was acquired in the hospital or in the community. This situation is most commonly observed when the length of hospitalization is less than or equal to the incubation period of the disease. In some cases, virological studies such as next generation sequencing can be used to differentiate between these situations [6].
As a measure to establish the magnitude of respiratory viral infections in the healthcare setting, it must be noted that 20% of all nosocomial pneumonias are of viral origin. In this context, the incidence of each virus is related to its circulation in the community [2, 7].
The objective of this revision is to describe the means of transmission and the measures to control the dissemination of respiratory viral infections in the healthcare setting.
Characteristics of viral respiratory pathogens
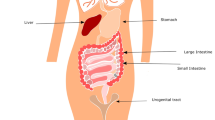
There are several viruses associated with upper and lower respiratory infections in humans. We describe the most relevant ones for the clinician.
Respiratory syncytial virus (RSV)
This virus belongs to the Mononegavirales order, Paramyxoviridae family and Pneumovirinae subfamily. Main characteristics of RSV include the number and order of genes and lack of hemagglutinin and neuraminidase activity [8].
RSV is the main cause of respiratory tract disease in small children. Viral propagation is so efficient that humans can acquire this infection in their first years of life. Immunity achieved after RSV infection is incomplete and reinfections are frequent. Although life threatening infections occur mainly during the first 2 years of life, RSV infections can cause a high morbidity due to acute upper and lower respiratory tract infections. In children, RSV causes bronchiolitis and pneumonia and it is a common pathogen in older adults and immunocompromised hosts, where it can either cause upper respiratory infections or pneumonia [9].
Influenza viruses
Influenza viruses are single-stranded, negative-sense RNA viruses belonging to the Orthomyxoviridae family and are classified into three main types, A, B and C, based on their antigenic different characteristics. These three types show significant differences related to their genetic organization, structure, possible hosts, epidemiology and clinical manifestations, with influenza A and B the most common human pathogens. These viruses share certain features such as the presence of an envelope derived from the host cell and surface glycoproteins essential for replication. They have a spheric or filamentous shape and measure 8 to 120 nm with surface projections that are spicules of hemagglutinins (HA) and neuraminidases (NA), also important for their antigenic mutations, as they are used as antigens for the influenza vaccine [10].
Human adenovirus (HadV)
This virus is an important cause of infections in immunocompetent and in immunocompromised hosts causing mild upper respiratory infections (pharyngitis, coryza, conjunctivitis) and complicated infections (pneumonia, hepatitis, hemorrhagic cystitis or disseminated diseases), respectively. There are seven species of HadV (A to G) and an increasing number of different serotypes were identified through genomic assays. Besides this, the improved understanding of viral persistence sites and reactivation requires continuous adaptations of diagnostic tools in order to facilitate timely detection and control of HAdV infections. HAdV infections are more frequent in closed communities such as the armed forces, nurseries and hospitals with immunocompromised hosts [11••].
Human parainfluenza virus (PIV)
This is a single-stranded RNA virus from the Paramyxoviridae family classified into five types: Respirovirus genus (PIV 1 and 3) and Rubulavirus (PIV 2, 4A, and 4B). [12]
PIV serotypes may cause bronchiolitis, laryngotracheobronchitis (croup) and pneumonia in different age groups in immunocompetent hosts, with PIV 3 more frequently associated with lower respiratory tract infections. Among immunocompromised hosts, PIV has been found in upper and lower respiratory tract infections in 2.2 - 7.1% of HSCT recipients. In solid organ transplant patients, lung recipients have demonstrated to be at risk for PIV disease and this infection was also associated to allograft rejection or dysfunction [13].
Human metapneumovirus (hMPN)
These viruses are non-segmented RNA viruses, belonging to the Mononegavirales order, Paramyoviridae family, Pneumovirinae subfamily and Metapneumovirus genus. Initially described as a pathogen in children, where it can cause upper respiratory disease, bronchiolitis and pneumonia, has also been later identified as an adult respiratory viral pathogen [14]. In immunocompromised hosts, hMPN has also been associated to produce upper and lower respiratory tract infections among HSCT patients and solid organ recipients, mainly lung transplant patients [13].
Picornaviruses
Picornaviridae family includes nine genuses, four of which (rhinovirus, enterovirus, parechovirus and hepatovirus) can infect humans. Human rhinoviruses (HRV) were classified based on immune serotypes, type of receptor, antiviral sensitivity and genotype. Rhinovirus infectivity can be neutralized by specific antisera and the new serotypes are defined based on the absence of cross reactivity with known specific antisera. HRV are RNA viruses and more than 160 serotypes have been identified. Clinical importance of HRV infections is well demonstrated in children where they are responsible for more than 70% of asthma exacerbations [15]. In immunocompetent adults, these are the most common cause of self-limited upper respiratory tract infections and could be responsible for more than 80% of common colds in autumn and spring seasons [16]. Immunocompromised hosts are particularly prone to severe infections. In lung transplant patients can be a common infection and lead to graft dysfunction. Among hematological malignancies HRV can produce lower respiratory tract infections with potential adverse consequences [11••, 17, 18].
Human coronaviruses (HCoV)
HCoV are positive-stranded RNA viruses from the Coronaviridae family, causing common colds; in children, they have also been associated with bronchiolitis and croup [19]. There are five HCoV identified as HCoV-OC43, HCoV-229E, HCoV-HKU1, HCoV-NL63 and HCoV-SARS. The latter virus was responsible of an epidemic of severe respiratory disease syndrome in some countries in Asia (China, Hong Kong SAR, Taiwan, Singapore, Vietnam) and Canada in 2003, with approximately 10% mortality and high attack rate in healthcare workers and family members; it was detected in humans for the last time in 2004 [19, 20].
More recently, one coronavirus was able to cause severe respiratory disease in humans in the middle east. This coronavirus was named as MERS-CoV and was isolated in Saudi Arabia in 2012 from respiratory secretions in a man who died from pneumonia. This finding, combined with a retrospective assessment of stored samples from an outbreak observed in healthcare workers in Jordan, allowed the recognition of MERS-CoV as a cause of this new severe respiratory disease [21•].
The origin of MERS-CoV has been widely debated. It was originally believed that the reservoir was bats due to the similarity between MERS-CoV and bat coronavirus. However, the strain found in humans was not related to the one described in bats. Another possible source for this type of coronavirus is the camel because they have antibodies against MERS-CoV similar to those found in humans. Most human cases of MERS-CoV were described in Saudi Arabia and, to a lesser degree, in the United Arabs Emirates. Later on, other cases outside the Arabian Peninsula were notified, but all of them were imported from endemic countries in the Middle East, and were related to close contact with sick people. Most of the patients were healthy males around 50 years [22].
Human bocavirus (HBoV)
This is a single-stranded DNA virus that has recently been found as a human pathogen. It belongs to the Parvoviridae family, Parvovirinae subfamily, bocaparvovirus genus; four genotypes have been described (HBoV 1 -4) [23, 24]. HBoV has been associated with upper and lower respiratory tract infections, sometimes as a single agent or as a co-pathogen with other viruses. It is also found in high proportion in fecal samples of children who had the virus already detected in respiratory samples. It has also been reported in stool and blood of immunosuppressed hosts [13].
Transmission
RSV
This virus is transmitted through droplets or by direct contact (Table 1) [25]. Droplet transmission is possible when the source is within 1 m. The size of droplets, produced by coughing, sneezing or any other procedure that moves respiratory secretions, is larger than 5 μm. Recent data has demonstrated the transmission of RSV through aerosolized particles based on the fact that they appear close to hospitalized children with bronchiolitis and RSV infections. These particles can remain suspended in the air for prolonged periods of time and can infect human epithelial cells [26].
The survival of RSV in the environment seems to be partly dependent on drying time and dew point. At room temperature RSV in patients’ secretions can be viable on polished surfaces for 3 to 30 h. On porous surfaces such as cloth or tissue papers viability is shorter, usually less than an hour. Viral infectivity in the hands varies from person to person, generally less than an hour [27].
The risk of transmission is not the same in all the hospital areas: in pediatric and neonatal units, risk of transmission occurs between 6% and 56%, in transplant and oncohematological units fluctuates between 6% and 12%, and in other adult wards between 30% and 32% [28]. It must also be considered that healthcare workers can be a source of transmission for RSV, considering that shedding occurs between 15% to 20% of them, even without symptoms [29].
In high transmission sites, as in oncohematological adult patient wards, it is recommended to manage these infections in ambulatory care to decrease the risk of transmission within the hospital. Nevertheless, it has been demonstrated that this group of patients can acquire RSV and PIV infections in spite of their short time of hospitalization [30, 31].
Influenza
Influenza virus can be transmitted through infectious droplets eliminated by patients when coughing or sneezing, or through direct contact with surfaces contaminated by respiratory secretions from symptomatic infected subjects (Table 1) [32]. Airborne transmission was observed with 2009 influenza A H1N1p strain; therefore, airborne precautions should also be implemented in case of a pandemic situation where high risk of aerosolization can occur (e.g. intubation) [13]. In closed areas with high risk patients, such as bone marrow transplant units about 50% of the infections come from healthcare personnel or infected visitors [33•]. Another source of nosocomial transmission of influenza are hospitalized patients with prolonged viral shedding, sometimes for weeks or months. High risk patients for prolonged shedding include those under high doses of steroids, oncohematological patients and children [13, 28, 32].
Another potential source of transmission at the hospital are those individuals not yet symptomatic, but within 1-3 days prior the infection. These cases are difficult to detect, and hence, preventive control measures are usually not implemented [34].
Different studies show that healthcare workers are one of the main vehicles of transmission of influenza within the hospital. There is data showing that many of them continue to work being ill, which certainly amplifies the rate of transmission [35].
Adenovirus
It is transmitted through direct contact with a contaminated patient’s environment and also by fomites containing the virus (Table 1). Adenovirus can also be transmitted through the fecal-oral route and by organ transplantation from infected donors. It can infect an individual, remain latent for a period of time and later cause disease during immunosuppression [36]. The ability of adenovirus to survive in the environment on certain surfaces like non-porous ones can be as prolonged as 49 days, facilitating its transmission [37].
PIV
It is transmitted through direct contact with patients’ secretions or by direct contact with the contaminated environment (Table 1). This virus can survive more than 4 h on porous surfaces and more than 10 h on non-porous surfaces. However, it is difficult to recover it from the hands and only 5% has been detected after 10 min of contact with contaminated secretions [38]. PIV can also be transmitted through droplets, and nosocomial outbreaks have been described [13, 39, 40]. Nosocomial transmission has been reported in pediatric and neonatal emergency wards, as well as in nurseries [41••]. Immunosuppressed hosts, particularly HSCT and oncohematological patients, are more prone to present PIV infections with an incidence of 4% and 2%, respectively [42]. Viral asymptomatic excretion has been described in HSCT and oncohematological patients, further increasing transmission in the hospital setting [43].
hMPN
This virus is transmitted by respiratory secretions from coughing, sneezing or through direct contact with contaminated surfaces (Table 1). It is transmitted mainly within the community, but a few reports of nosocomial outbreaks have been described [44].
HRV
Autoinoculation is the most common way of transmission after contact with contaminated objects. Aerosolization also contributes to viral spread (Table 1) [45].
Coronavirus
Some epidemiologic data support the possibility of transmission by contact or by air (Table 1). However, means of transmission of MERS-CoV have not been elucidated yet. The epidemiology of MERS-CoV infection since isolation of the pathogen in 2012 is consistent with multiple introductions of the virus into humans from an animal reservoir, with no long-term sustained human-to human transmission [46].
HBoV
HBoV is probably transmitted through respiratory droplets; however; nosocomial transmission of HBoV has not been reported (Table 1) [13].
Preventive and Infection Control Measures
Education of healthcare workers, close monitoring of compliance to preventive measures, and infection surveillance are useful tools to reduce the risk of transmission for most respiratory viruses that cause nosocomial infections [2]. In the following section, preventive and control measures for each respiratory virus are described.
RSV
The precautions recommended by the CDC to avoid RSV transmission include standard and contact precautions (handwashing with water and soap or alcohol hand rub; appropriate use of gloves in order to decrease autoinoculation and use of gown) [2]. Use of facemask (droplet precautions) and goggles when direct contact with the patient are also recommended by others (Table 2) [29, 47]. Eye protection should always be worn when performing procedures that might generate sprays from respiratory secretions, considering that nose and eyes are the main sites for virus inoculation [2, 47]. CDC also recommends that infected patients be hospitalized in single rooms or kept in cohort isolation if no individual isolation rooms are available. When cohorting, there should be at least 0.9 m of separation between beds [2]. Another measure to be considered is the use of individual equipment for each patient, including toys. Other strategies that help prevent RSV transmission in the healthcare setting include: reducing the quantity of persons in contact with hospitalized patients (especially oncohematological), avoiding the presence of children under 12 years of age in the hospital when RSV circulates either in the community or the hospital, and using single-bed rooms for infected patients [2, 29, 48].
Some studies have demonstrated that healthcare workers use of eye protection might more efficient than contact precautions in decreasing the risk of RSV transmission within the hospital setting [28].
Other recommendations, with very little or no evidence at all, suggest that healthcare personnel caring for RSV infected patients be exclusive for these individuals and that hospital visitor restrictions be taken during RSV season. The use of drugs for prophylaxis is limited to palivizumab in the high risk pediatric population although there are some data that demonstrates its effectiveness in the prevention of RSV in HSCT adult patients [13, 49,50,51].
Influenza
Annual influenza vaccination of healthcare workers and high-risk patients for influenza complications and their households is the most effective measure to prevent the disease and its complications. It also contributes to decrease viral transmission in the healthcare setting [2]. Vaccination of healthcare workers is the second most important strategy, just behind handwashing, to prevent nosocomial dissemination of influenza [41••]. Several studies have demonstrated a reduction in morbidity and mortality among patients in different healthcare settings when healthcare workers have been vaccinated against influenza [41••]. Different strategies were successfully implemented in order to increase vaccine uptake in healthcare personnel. Among these were educational campaigns regarding benefits of the vaccine for patients and personnel, actions addressed to remove administrative barriers for vaccination, implementation of accessible locations for vaccine administration and of signed declination statements, and mandatory vaccination policies for healthcare workers [52]. However, the scientific support for this last strategy has been questioned recently [53].
Antivirals against influenza have proved effective to reduce influenza viral transmission. The ones now available are the neuraminidase inhibitors such as oseltamivir, zanamivir and peramivir. Oseltamivir which is administered through the oral route has proved to effectively prevent secondary cases of influenza among household contacts if it is given within 48 h of symptoms initiation of the index case. Zanamivir, which is administered by inhalation per mouth, has also proved effective in preventing secondary influenza cases in households and healthcare workers [54, 55], but caution is advised, as its efficacy has only been demonstrated in particular circumstances. During a nosocomial outbreak, in high-risk patients and non-vaccinated healthcare workers, antiviral administration should be implemented. When a mismatch between the circulating influenza strain and the vaccine strain is identified, antiviral prophylaxis should be given to all healthcare workers if an outbreak occurs. Duration of antiviral administration during a nosocomial outbreak of influenza should be two weeks or one week after the outbreak control [2].
Besides vaccination and antivirals, infection control measures are of utmost importance in order to prevent influenza virus transmission and dissemination in the hospital environment. These measures include handwashing, limitation of visitors and of health personnel in contact with infected patients, cohort or single bed rooms isolation, and droplet precautions. Precautions to avoid aerosolization should also be implemented in case of a new pandemic strain or when performing high risk procedures (e.g. intubation) (Table 2) [13].
Adenovirus
Preventive measures to avoid adenovirus nosocomial infections include patient cohorting, reduction of visitors and contact and droplet precautions, along with the exclusion of infected healthcare workers from clinical duties (Table 2) [13, 36]. Handwashing seems to be non-effective in removing adenovirus from contaminated fingers [56]. There are no available vaccines or antiviral prophylaxis to help prevent adenovirus infection [33•, 57, 58].
PIV
In order to prevent nosocomial transmission of PIV several measures are proposed. They include contact precautions, reinforcement of hand hygiene and standard precautions in all patients to avoid an outbreak in the hospital setting (Table 2) [2]. There are some vaccines under the initial phases of development that take advantage of mucosal immunity, but there are no efficacy data yet [59].
hMPV
Infection control measures to prevent nosocomial transmission of this virus include handwashing and contact precautions (Table 2) [42].
MERS-CoV
There is no consensus regarding recommendations to prevent MERS-CoV transmission. While WHO recommends contact isolation and droplet precautions for any suspected case and respiratory precautions only for aerosol generating procedures, the CDC promotes air and contact precautions for all the activities related to patient care (Table 2). Other centers recommend intensification of handwashing, contact precautions, ocular protection and the use of facemasks. Currently, any suspected or confirmed MERS-CoV case should be treated in a medical facility. Transfer and transportation of an infected patient in the hospital environment should include a minimum crew, all wearing surgical facemasks. Healthcare workers with direct patient contact should follow the recommendations mentioned before and keep updated on new recommendations. Any transference of MERS-CoV infected patients from one healthcare setting to another should be coordinated with public health authorities [22, 57, 60].
HBoV
Although nosocomial transmission has not been reported, it seems prudent to implement at least contact precautions in patients when this virus is detected (Table 2).
Conclusions
The epidemiology of viral respiratory infections has been better understood and modified in the last years for multiple reasons, including vaccination, improvement in diagnostic assays such as molecular techniques and better knowledge and understanding of mechanisms of transmission.
This is also observed in the healthcare setting where respiratory viruses are recognized as a cause of URI and LRI. These infections are not only limited to children and may cause severe infections in immunocompromised patients.
Knowing the mechanisms of respiratory viral transmission in the healthcare setting allows to implement infection control measures to prevent its dissemination and reduce the risk of a hospital outbreak.
Early detection and strict compliance to infection control measures limit the spread of nosocomial viral respiratory infections. Other measures, such as healthcare workers receiving an annual influenza vaccination, should be encouraged.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
• CDC/NHSN Surveillance Definitions for Specific Types of Infections Surveillance Definitions January 2017 https://www.cdc.gov/nhsn/pdfs/pscmanual/17pscnosinfdef_current.pdf This reference allows the reader to have the latest updated definitions of upper and lower respiratory tract infections.
Tablan OC, Anderson LJ, Besser R, Bridges C, Hajjeh R. CDC, Healthcare Infection Control Practices Advisory Committee. Guidelines for preventing health-care--associated pneumonia, 2003: recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee. MMWR Recomm Rep. 2004;53(RR-3):1–36.
Vakil E, Evans SE. Viral Pneumonia in Patients with Hematologic Malignancy or Hematopoietic Stem Cell Transplantation. Clin Chest Med. 2017;38(1):97–111. https://doi.org/10.1016/j.ccm.2016.11.002.
• Paulsen GC, Danziger-Isakov L. Respiratory Viral Infections in Solid Organ and Hematopoietic Stem Cell Transplantation. Clin Chest Med. 2017;38(4):707–26. https://doi.org/10.1016/j.ccm.2017.07.012. Paulsen GC and co-authors’ reference is important because nosocomial respiratory tract infections are frequent and severe in this group of patients. This article allows the reader to get updated on respiratory viral infections in immunosuppressed hosts.
Diederen BM, Van Der Eerden MM, Vlaspolder F, Boersma WG, Kluytmans JA, Peeters MF. Detection of respiratory viruses and Legionella spp. By real-time polymerase chain reaction in patients with community acquired pneumonia. Scand J Infect Dis. 2009;41(1):45–50. https://doi.org/10.1080/00365540802448799.
Kothari A, Burgess MJ, Crescencio JCR, et al. The role of next generation sequencing in infection prevention in human parainfluenza virus 3 infections in immunocompromised patients. J Clin Virol. 2017;92:53–5. https://doi.org/10.1016/j.jcv.2017.05.010.
Hall CB. Nosocomial viral respiratory infections: perennial weeds on pediatric wards. Am J Med. 1981;70:670–6.
Rhee EG, Barouch DH. Adenovirus 1784-1793. In: Mandell, Douglas, and Bennett’s Principles and practice of infectious diseases, 8th edition.
Micek ST, Chew B, Hamptom N, Kollef MH. A case control study assessing the impact of non-ventilated hospital-acquired pneumonia on patient outcome. Chest. 2016;150:1008–14. https://doi.org/10.1016/j.chest.2016.04.009.
Jhon J. Treanor: influenza (including Avian Influenza and Swine Influenza) 2272-2296. In: Mandell, Douglas, and Bennett’s principles and practice of infectious diseases, 8th Edition.
•• Walter JM, Wunderink RG. Severe respiratory viral infections. New evidence and changing paradigms. Infect Dis Clin N Am. 2017;31:455–74. https://doi.org/10.1016/j.idc.2017.05.004. This reference reviews all the aspects related to respiratory viral infections including those which are of nosocomial origin. It is a very detailed and exhaustive description of the most common and frequent viral respiratory tract infections. It describes each virus, their mechanisms of transmission, most common affected hosts, diagnostics techniques and treatment and preventing strategies.
Michael G. Ison Parainfluenza viruses. 2580-87. In: Mandell, Douglas, and Bennett’s principles and practice of infectious diseases, 8th edition.
Weigt SS, Gregson AL, Deng JC, Lynch JPIII, Belperio JA. Respiratory Viral Infections in Hematopoietic Stem Cell and Solid Organ Transplant Recipients. Semin Respir Crit Care Med. 2011;32:471–93. https://doi.org/10.1055/s-0031-1283286.
van den Hoogen BG, de Jong JC, Groen J, Kuiken T, de Groot R, Fouchier RA, et al. A newly discovered human pneumovirus isolated from young children with respiratory tract disease. Nat Med. 2001;7:719–24. https://doi.org/10.1038/89098.
Rakes GP, Arruda E, Ingram JM, et al. Rhinovirus and respiratory syncytial virus in wheezing children requiring emergency care. IgE and eosinophil analyses. Am J Respir Crit Care Med. 1999;159:785–90.
Arruda E, Pitkaranta A, TJr W, Doyle CA, Hayden FG. Frequency and natural history of rhinovirus infections in adults during autumn. J Clin Microbiol. 1997;35:2864–8.
Kaiser L, Aubert JD, Pache JC, et al. Chronic rhinoviral infection in lung transplant recipients. Am J Respir Crit Care Med. 2006;174:1392–9.
Jacobs SE, Lamson DM, Soave R, et al. Clinical and molecular epidemiology of human rhinovirus infections in patients with hematologic malignancy. J Clin Virol. 2015;71:51–8. https://doi.org/10.1016/j.jcv.2015.07.309.
Abdul-Rasool S, Fielding BC. Undestanding human coronavirus HCoV-NL63. Open Virol J. 2010;4:76–84. https://doi.org/10.2174/1874357901004010076.
World Health Organization. Summary of probable SARS cases with onset of illness from 1 November 2002 to 31 July 2003. Available at: http://www.who.int/csr/sars/country/table2004_04_21/en/. Accessed 2 Feb 2018.
• Arabi YM, Baklhy HH, Hayden FG, et al. Middle east respiratory syndrome. N Engl J Med. 2017;376:584–95. https://doi.org/10.1056/NEJMsr1408795. Middle east respiratory syndrome is a severe and emerging respiratory viral infection that can also be transmitted in the health care setting. This article describes in detail the latest advances in the research of MERS-coV, its epidemiology, mechanisms of transmission, virus characteristics, pathogenesis, clinical manifestations, diagnosis and treatment approaches.
Shapiro M, London B, Nigri D, et al. Middle east respiratory syndrome coronavirus: review of the current situation in the world. Disaster and Mil Med. 2016;2:9. https://doi.org/10.1186/s40696-016-0019-2. eCollection 2016
Allander T, Tammi MT, Eriksson M, Bjerkner A, Tiveljung-Lindell A, Andersson B. Cloning of a human parvovirus by molecular screening of respiratory tract samples. Proc Natl Acad Sci U S A. 2005; https://doi.org/10.1073/pnas.0504666102.
De R, Liu L, Qian Y, Zhu R, Deng J, Wang F, et al. Risk of acute gastroenteritis associated with human bocavirus infection in children: A systematic review and meta-analysis. PLoS ONE. 2017;12(9):e0184833. https://doi.org/10.1371/journal.pone.0184833.
Jensen TO, Stelzer-Braid S, Willenborg C, Cheung C, Andressen D, Rawlinson W, et al. Outbreak of respiratory syncytial virus (RSV) infection in immunocompromised adults on a hematology ward. J Med Virol. 2016;88:1827–31. https://doi.org/10.1002/jmv.24521.
Kulkarni H, Smith CM, Lee Ddo H, Hirst RA, Easton AJ, O’Callaghan C. Evidence of Respiratory Syncytial Virus Spread by Aerosol. Time to Revisit Infection Control Strategies? Am J Respir Crit Care Med. 2016;194:308–16. https://doi.org/10.1164/rccm.201509.1833OC.
Edward E. Walsh and Caroline Breese Hall Respiratory Syncytial Virus (RSV).2597-2613. In: Mandell, Douglas, and Bennett’s principles and practice of infectious diseases, 8th edition.
French CE, McKenzie BC, Coope C, et al. Risk of nosocomial respiratory syncytial virus infection and effectiveness of control measures to prevent transmission events: a systematic review. Influenza Other Respir Viruses. 2016:268–90. https://doi.org/10.1111/irv.12379.
Hall CB, Hall CB. Nosocomial respiratory syncytial virus infections: the “Cold War” has not ended. Clin Infect Dis. 2000;31:590–6.
Nichols WG, Erdman DD, Han A, Zukerman C, Corey L, Boeckh M. Prolonged outbreak of human parainfluenza virus 3 infection in a stem cell transplant outpatient department: insights from molecular epidemiologic analysis. Biol Blood Marrow Transplant. 2004;10:58–64. https://doi.org/10.1016/j.bbmt.2003.09.010.
Machado AF, Sallum MA, Vilas Boas LS, Tateno AF, Machado CM. Molecular characterization of strains of respiratory syncytial virus identified in hematopoyetic stem cell transplant outpatient unit over 2 years: community or nosocomial infection. Biol Blood Marrow Transplant. 2008;14:1348–55. https://doi.org/10.1016/j.bbmt.2008.09.012.
Tomblyn M, Chiller T, Einsele H, et al. Guidelines for preventing infectious complications among hematopoietic cell transplant recipients: a global perspective. Biol Blood Marrow Transplant. 2009;15:1143–238. https://doi.org/10.1016/j.bbmt.2009.06.019.
• Abbas S, Raybould JE, Sastry S, de la Cruz O. Respiratory viruses in transplant recipients: more than just a cold. Clinical syndromes and infection prevention principles. Int J Infect Dis. 2017;62:86–93. https://doi.org/10.1016/j.ijid.2017.07.011. The authors of this article address the importance of RSV, adenovirus, PAI, HRV, influenza and hMPN in both SOT and HSCT patients. They point out the main characteristics of these viruses in immunosuppressed hosts such as prolonged excertion and higher morbidity and mortality in relation to normal hosts. Also, they describe mechanism of transmission and preventive measures.
Douglas RG Jr. Influenza in man. In: Kilborune ED, editor. The influenza viruses and influenza. New York: Academic Press; 1975. p. 395–447.
Elder AG, O'Donnell B, McCruden EA, Symington IS, Carman WF. Incidence and recall of influenza in a cohort of Glasgow healthcare workers during the 1993-4 epidemic: results of serum testing and questionnaire. BMJ. 1996;313:1241–2.
Ison MG, Green M, AST Infectious Diseases Community of Practice. Adenovirus in solid organ transplant recipients. Am J Transplant. 2009;S4:S161–5. https://doi.org/10.1111/j.1600-6143.
Gordon YJ, Gordon RY, Romanowsky E, Araullo-Cruz TP. Prolonged recovery of desiccated adenoviral serotypes 5, 8, and 19 from plastic and metal surfaces in vitro. Ophtalmology. 1993;100:1835–9.
Ansari SA, Springthorpe VS, Sattar SA, Rivard S, Rahman M. Potential role of hands in the spread of respiratory viral infections: studies with human parainfluenza virus 3 and rhinovirus 14. J Clin Microbiol. 1991;29:2115–9.
Raad I, Abbas J, Whimbey E. Infection Control of Nosocomial Respiratory Viral Disease in the Immunocompetent Host. Am J Med. 1997;102:48–52.
Sydnor ER, Greer A, Budd AP, et al. An outbreak of human parainfluenza virus 3 infection in an outpatient hematopoietic stem cell transplantation clinic. Am J Infect Control. 2012;40:601–5. https://doi.org/10.1016/j.ajic.2011.11.011.
•• Dare RK, Talbot TH. Health care – acquired viral respiratory diseases. Infect Dis Clin N Am. 2016;30:1053–70. https://doi.org/10.1016/j.idc.2016.07.004. Dare and Talbot make a very good description of health care acquired viral respiratory infections, their different control measures(education, hand-washing, isolation, PPE, cohorting of patients and personnel) and other measures such as influenza vaccination.
Shah DP, Shah PK, Azzl JM, Chemaly RF. Parainfluenza virus infections in hematopoietic cell transplant recipients and hematologic malignancy patients: a systematic review. Cancer Lett. 2016;370:358–64. https://doi.org/10.1016/j.canlet.2016.05.035.
Peck AJ, Englund JA, Kuypers J, Guthrie KA, Corey L, Morrow R, et al. Respiratory virus infection among hematopoietic cell transplant recipients: evidence for asymptomatic parainfluenza virus infection. Blood. 2007;110:1681–8.
Lee I, Barton TD. Viral respiratory tract infections in transplant patients: epidemiology, recognition and management. Drugs. 2007;67:1411–27.
Musher DM. How contagious are common respiratory tract infections? N Engl J Med. 2003;348(13):1256–66.
Guery B, Poissy J, el Mansouf L, et al. Clinical features and viral diagnosis of two cases of infection with Middle East Respiratory Syndrome coronavirus: a report of nosocomial transmission. Lancet. 2013;381:2265–72. https://doi.org/10.1016/S1473-3099(13)70153-1.
Siegel JD, Rhinehart E, Jackson M, Chiarello L, and the Healthcare Infection Control Practices Advisory Committee, 2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings https://www.cdc.gov/infectioncontrol/guidelines/isolation/index.html
Harrington RD, Hooton TM, Hackman RC. An outbreak of respiratory syncytial virus in a bone marrow transplant center. J Infect Dis. 1992;165:987–93.
Recommendations of the Center for International Blood and Marrow Transplant Research (CIBMTR®), the National Marrow Donor Program (NMDP), the European Blood and Marrow Transplant Group (EBMT), the American Society of Blood and Marrow Transplantation (ASBMT), the Canadian Blood and MarrowTransplant Group (CBMTG), the Infectious Disease Society of America (IDSA), the Society for Healthcare Epidemiology of America (SHEA), the Association of Medical Microbiology and Infectious Diseases Canada (AMMI), and the Centers for Disease Control and Prevention (CDC), Tomblyn M, Chiller T, Einsele H, Gress R, Sepkowitz K, et al. Guidelines for Preventing Infectious Complications among Hematopoietic Cell Transplant Recipients: A Global Perspective. Biol Blood Marrow Transplant. 2009;15:1143–238.
Kassis C, Champlin RE, Hachem RY, et al. Detection and control of a nosocomial respiratory syncytial virus outbreak in a stem cell transplantation unit: the role of palivizumab. Biol Blood Marrow Transplant. 2010;16:1265–71.
Walsh EE. Respiratory syncytial virus infection in adults. Semin Respir Crit Care Med. 2011;32:423–32.
Advisory Committee on Immunization Practices; Center for Diseases Control and Prevention (CDC). Immunization of health-care personnel: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2011;60(RR-7):1–45.
De Serres G, Skowronski DM, Ward BJ, Gardam M, Lemieux C, Yassi A, et al. Influenza Vaccination of Healthcare Workers: Critical Analysis of the Evidence for Patient Benefit Underpinning Policies of Enforcement. PLoS ONE. 2017;12(1):e0163586. https://doi.org/10.1371/journal.pone.0163586.
Doll MK, Winters N, Boikos C. Safety and effectiveness of neuraminidase inhibitors for influenza treatment, prophylaxis, and outbreak control: a systematic review of systematic reviews and/or meta-analyses. J Antimicrob Chemther. 2017;72(11):2990–3007. https://doi.org/10.1093/jac/dkx271.
Anekthananon T, Pukritayakamee S, Ratanasuwan W, et al. Oseltamivir and inhaled zanamivir as influenza prophylaxis in Thai heaith workers: a randomized, double-blind, placebo-controlled safety trial over 16 weeks. J Antimicrob Chemother. 2013;68:697–707. https://doi.org/10.1093/jac/dks418.
Jernigan JA, Bs L, Hayden FG, Kyger SA, Conway BP, Groschel DH, et al. Adenovirus type 8 epidemic keratoconjunctivitis in an eye clinic: risk factors and control. J Infect Dis. 1993;167:1307–13.
Sandkovsky U, Vargas L, Florescu DF. Adenovirus: current epidemiology and emerging approaches to prevention and treatment. Curr Infect Dis Rep. 2014;16:416. https://doi.org/10.1007/s11908-014-0416-y.
Gautret P, Gray GC, Charrel RN, Odezulu NG, Al-Tawfiq JA, Zumla A, et al. Emerging viral respiratory tract infections—environmental risk factors and transmission. Lancet Infect Dis. 2014;14:1113–22. https://doi.org/10.1016/S1473-3099(14)70831-X.
Adderson E, Branum K, Sealy RE, et al. Safety and immunogenicity of an intranasal Sendai virus-based human parainfluenza virus type 1 vaccine in 3- to 6-year-old children. Clin Vaccine Immunol. 2015;22:298–303. https://doi.org/10.1128/CVI.00618-14.
Mackay IM, Arden KE. An opportunistic pathogen afforded ample opportunities: Middle East Respiratory Syndrome Coronavirus. Viruses. 2017;9:369. https://doi.org/10.3390/v9120369.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Treatment and Prevention of Hospital Infections
Rights and permissions
About this article
Cite this article
Bonvehí, P.E., Temporiti, E.R. Transmission and Control of Respiratory Viral Infections in the Healthcare Setting. Curr Treat Options Infect Dis 10, 182–196 (2018). https://doi.org/10.1007/s40506-018-0163-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40506-018-0163-y