Opinion statement
Human factors engineering (HFE), with its focus on studying how humans interact with systems, including their physical and organizational environment, the tools and technologies they use, and the tasks they perform, provides principles, tools, and techniques for systematically identifying important factors, for analyzing and evaluating how these factors interact to increase or decrease the risk of Healthcare-associated infections (HAI), and for identifying and implementing effective preventive measures. We reviewed the literature on HFE and infection prevention and control and identified major themes to document how researchers and infection prevention staff have used HFE methods to prevent HAIs and to identify gaps in our knowledge about the role of HFE in HAI prevention and control. Our literature review found that most studies in the healthcare domain explicitly applying (HFE) principles and methods addressed patient safety issues not infection prevention and control issues. In addition, most investigators who applied human factors principles and methods to infection prevention issues assessed only one human factors element such as training, technology evaluations, or physical environment design. The most significant gap pertains to the limited use and application of formal HFE tools and methods. Every infection prevention study need not assess all components in a system, but investigators must assess the interaction of critical system components if they want to address latent and deep-rooted human factors problems.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
To prevent healthcare-associated infections (HAIs), infection prevention and control staff and other healthcare workers must systematically identify, analyze, and evaluate factors associated with HAIs, and how these factors interact. Such factors include:
-
(1)
people, both patients, and healthcare workers;
-
(2)
medical devices, tools, and technologies;
-
(3)
personal protective equipment used by healthcare workers;
-
(4)
the physical environment; and
-
(5)
infection prevention and control guidelines, policies, and procedures.
Human factors engineering (HFE), with its focus on studying how humans interact with systems, including their physical and organizational environment, the tools and technologies they use, and the tasks they perform, provides principles, tools, and techniques for systematically identifying important factors, for analyzing and evaluating how these factors interact to increase or decrease the risk of HAI, and for identifying and implementing effective preventive measures [1].
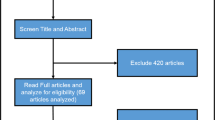
We reviewed the literature on HFE and infection prevention and control and identified major themes to document how researchers and infection prevention staff have used HFE methods to prevent HAIs and to identify gaps in our knowledge about the role of HFE in HAI prevention and control. To accomplish this goal, we searched, with the help of a research librarian, more than 1000 research databases including PubMed, Web of Science, Ingenta Connect, JSTOR and EBSCO to find relevant publications. This paper reports the results of this literature review.
Review findings
We categorized the studies into those that evaluated: HFE and hand hygiene promotion, behavioral science determinants of HAI prevention, the physical environment as a factor in HAI prevention, technological determinants of HAI prevention, HFE and use of personal protective equipment, and overall infection prevention topics. The paper discusses the major thematic areas in the following sections.
Human factors engineering and hand hygiene
Many studies applying HFE techniques to infection prevention and control have investigated hand hygiene practice and efforts to improve hand hygiene compliance. Many of these studies have examined how systems, the environment, cognitive factors, technology, and training affect hand hygiene adherence (Fig. 1).
Hand hygiene improvement using the systems approach
Studies have assessed whether organizational factors such as leadership, organizational support and culture [2], and coordination mechanisms (e.g., huddles), affect hand hygiene compliance. For example, Voss and Widmer [3] calculated that during a single intensive care unit (ICU) shift, 12 nurses would spend 2 h doing hand hygiene with an alcohol-based hand rub if they were 60% compliant and 4 h if they were 100% compliant. Moreover, several groups have found that healthcare workers’ workload affects their hand hygiene compliance [4, 5, 6, 7•]. Lee et al. [4] conducted an observational study in nine European countries and found that the nurses’ workload, as assessed by the patient to nurse ratio, was inversely associated with compliance in the multivariable analysis. Dunn-Navarra et al. [8] found that hospitals with morning huddles were significantly more likely than other hospitals to report hand hygiene compliance rates of ≥95%, suggesting that the “organizational tools to improve teamwork, coordination, and communication” among healthcare workers may facilitate hand hygiene improvement efforts. In contrast, they found that other organizational factors did not influence hand hygiene compliance significantly [8].
Hand hygiene and the built environment
Carter et al. [9••] conducted an observational study to examine how physical layout affects hand hygiene compliance. Their multivariable analysis found that compliance was lowest when the emergency department was most crowded and was lower in “hallway care areas” than in semiprivate areas [9••]. In addition, the location of hand sanitizing products within the geographical space of the care environment significantly affects compliance [10,11,12,13]. Birnbach [12] found that dispenser location and visibility within patient rooms significantly affected hand hygiene adherence (i.e., immediately adjacent to the patient [53.8%] vs. across from the patient’s bed and not clearly visible [11.5%]). Suresh et al. [14] used an ergonomic assessment tool to evaluate ICUs and 59 patient rooms for “structural ergonomic characteristics” that facilitate use of alcohol-based hand rub dispensers. They found “deficiencies in the structural layout” that could hinder use of dispensers. For example, dispensers were in locations where healthcare workers could not see or access them easily and dispensers often were in locations that did not facilitate their use within the sequence of care [14]. To address the visibility issue, Rashidi et al. [15•] and D’ Egidio et al. [16] placed flashing lights to dispensers and found that hand hygiene adherence increased. However, the compliance rates during the intervention periods were still unacceptably low, 20.7 and 25.3%, respectively [16, 15•]. Healthcare workers and companies that make hand hygiene dispensers might avoid the problems described by Birnbach et al. [12] and Suresh et al. [14] or failed interventions, like that described by Rashidi et al. [15•] and D’ Egidio et al. [16] if they apply the HFE principles of salience, perception and attention, and effective display design. For example, dispensers designed based on the principle of salience (e.g., bright color, unique shape, context sensitive blinking lights or audio) could help healthcare workers more easily perceive dispensers in the patient care zone, and remind them to “attend” to hand hygiene more consistently.
Hand hygiene and healthcare worker’s perceptions
Behavioral modeling studies [2] and reviews of current literature on HCW’s hand hygiene-related behaviors [17, 18] have shown that interpersonal factors and individual healthcare workers’ characteristics affect hand hygiene compliance. For example, Pittet et al. [6] found that hand hygiene compliance was associated with a “positive attitude toward hand hygiene after patient contact,” the awareness that one’s hand hygiene was being observed, and the belief that one was a role model for other healthcare workers. In addition, healthcare workers’ perceptions of infection risks associated with improper hand hygiene and their knowledge of hand hygiene guidelines and mechanisms of transmission can influence hand hygiene compliance [19]. McLaughlin et al. [19] found that higher levels of knowledge about hand hygiene were associated with a beneficial effect on healthcare workers’ assessment of the risk that they could transfer pathogens to patients. However, they noted that only very high levels of knowledge affected the risk ratings, suggesting that very high knowledge levels may be required to improve hand hygiene compliance.
Lutze et al. [20••] found that physicians and nurses working in ICUs believed that hand hygiene prevents transmission of pathogens. However, nurses perceived the risk reduction to be greater than did physicians, and nurses’ rated their knowledge of the guidelines higher than physicians rated their own knowledge. The belief that hand hygiene substantially reduced the transmission risk was associated with high response efficacy (the extent to which a person believes that a recommended response is effective), behavioral intention (a person’s assessment of the likelihood that she will engage in a specific behavior), and self-efficacy (a persons’ assessment of his ability to execute specific behaviors), but not with self-rated knowledge. On the basis of these results, Lutze et al. [20••] concluded that both educational measures and skills training are needed to improve hand hygiene compliance and that physicians may require special attention.
Hand hygiene, data monitoring technology and compliance
To date, most hospitals that monitor hand hygiene compliance have had human observers collect the data. However, human observers capture only a small percentage of the possible hand hygiene opportunities and they are susceptible to the Hawthorne effect [21••]. Automated systems are now available that continuously monitor hand hygiene compliance and, thus, provide data for higher percentage of hand hygiene opportunities and likely minimize the Hawthorne effect. Automated systems providing instant feedback may help increase compliance [22]. However, few studies have assessed whether they actually increase compliance [23••]. Automated systems also have the potential to produce standardized data for a hand hygiene metric that could be compared within or across healthcare facilities over time [21••]. Conway [21••] recently reviewed significant HFE issues associated with implementation of automated hand hygiene monitoring systems. We will discuss some of the issues in the following paragraphs.
Currently, automated systems range from devices recording each time a dispenser is used to fully automated systems recording all hand hygiene opportunities, providing feedback or reminders to healthcare workers, and responding to the healthcare workers’ actions [23••, 24, 25]. Results of studies comparing compliance as measured by human observers and by automated systems have varied. For example, Sharma et al. [26] evaluated nearly 1400 hand hygiene-related events recorded by an automated system and by human observers. They found that the details of the observations differed for 38% of the events. They postulated that the discrepancies may have been due to the “distance between the observer and the event” and the clinic’s level of busyness [26]. Swoboda et al. [27] found that hand hygiene compliance assessed by observers was 20% (±2%) higher than that assessed by the electronic monitoring system. They attributed this in part to the fact that the observers monitored compliance for healthcare workers only whereas the system monitored compliance for all persons entering the room. In contrast, Filho et al. [28] evaluated an automatic system and found a 92% (95% confidence interval [CI], 90%–95%) overall concordance with an intraclass correlation coefficient of 0.87 (95% CI, 0.77–0.92) when comparing the electronic system and human observers. Morgan et al. [22] conducted a quasi-experimental study and found that electronic dispenser counts increased significantly but directly observed compliance did not after monthly feedback of compliance data was introduced. They concluded that automatic systems might be more sensitive to changes in hand hygiene compliance and, thus, may assess results of an intervention more accurately than human observers, whereas, human observers provide information (e.g., was hand hygiene done at the appropriate time) necessary for those designing behavioral interventions to improve hand hygiene compliance [29, 22].
In the future, sophisticated intelligent sensing compliance monitoring systems may provide additional benefits. For example, these systems may be able to determine when healthcare workers are doing tasks that require hand hygiene after the task is complete, remind healthcare workers to do hand hygiene, and, provide timely feedback to healthcare workers on their hand hygiene compliance [29]. Additionally, intelligent sensing and monitoring systems could help us identify factors such as healthcare worker job classifications, “situations, locations, and specific times” associated with low hand hygiene compliance [29]. This information could help staff design effective interventions to improve compliance.
Current automatic systems have limitations. In 2014, Dawson et al. [30••] published a review of 19 systems and found that none were fully fit for purpose (FFP) with respect to monitoring, measuring, and providing feedback for all 5 hand hygiene moments specified by the World Health Organization (WHO). Fifteen systems were FFP for moment 1 (before touching a patient) and 14 were FFP for moment 4 (after touching a patient). Only 3 were FFP for moment 5 (after touching the patient’s surroundings) and none were FFP for moments 2 and 3 (before a clean or aseptic procedure and after doing a task with a risk of exposure to body fluids) [30••]. Many current systems do not provide information about contextual factors or work flow such as who enters the room (e.g., staff vs. visitors), the number of people entering a room (e.g., one person entering a room vs. a group of people entering together), or the reason people enter the room (e.g., doing patient care vs. asking the patient a question) [31, 23••, 22]. In addition, “sensor networks record hand hygiene events within a defined care area” and miss those that occur outside that area [23••]. Automatic systems also create issues regarding patient and healthcare worker confidentiality and privacy [32, 21••, 33].
Conway [21••] recently reviewed significant HFE issues associated with implementation of automated hand hygiene monitoring systems. She noted that the system must “minimize disruption to the physical structure and to clinician workflow” and fit with the “organization’s culture and budget.” Leaders must obtain “buy-in” from front–line workers and address their concerns about data accuracy and about “how the data will be used.” Leaders also must provide hand hygiene data to healthcare workers such that they can use the data to improve compliance [21••].
Hand hygiene, training and education
Results of several studies [30••, 34,35,36] suggest that multimodal programs including education and training together with feedback of compliance, effective reminders, and supportive organizational and system factors are necessary to improve hand hygiene compliance. A study by Widmer et al. [37] found that training improved both hand hygiene technique, as measured by the log10 reduction in bacterial colony forming units and hand hygiene compliance. Stewardson et al. [38••] found that a device using video-measurement technology and immediate feedback significantly improved the number of WHO-recommended “poses” healthcare workers used during hand hygiene. However, Kwok et al. [39] found that an automated hand hygiene training system used by 79% of clinicians was not associated with improved hand hygiene compliance. Gluck et al. [40] found that international medical graduates had lower hand hygiene compliance than American graduates during a standardized patient encounter. These investigators suggested that one should consider where physicians went to medical school when designing interventions, such as “intern orientation and clinical education,” to improve hand hygiene behaviors [40].
Several studies have shown that signs (i.e., reminders) alone or in combination with feedback of hand hygiene compliance data do not increase compliance [41, 42, 43•]. However, Reisinger et al. [43•] found that a sign “using messages focused on patient consequences and gain-framed language” was associated with higher absolute compliance compared with other theoretically derived signs, suggesting that the “specific type of messaging strategy” might affect the efficacy of hand hygiene poster campaigns.
Infection prevention and human factors engineering: Other topics
Investigators have used human factors engineering principles to address several other infection prevention issues, including: cognitive aspects of infection prevention, design of the physical environment, technology and tools, and design and use of personal protective equipment (PPE; Fig. 2). We briefly discuss these studies in this section.
Behavioral science and infection prevention and control interventions
Infection prevention experts are investigating the utility of applying methodologies and theories from behavioral sciences to infection prevention interventions [5]. Aside from studies done to improve hand hygiene compliance, most publications addressing social cognitive determinants of infection prevention behavior, including mental models, review the behavioral concepts and theories and then use them as a framework for describing possible multimodal interventions [5, 44••, 45, 46, 47]. In his Lowbury Lecture, Didier Pittet [5] discussed cognitive determinants, such as knowledge, motivation, threat perception, expectations regarding outcomes (attitude; perceived efficacy of an intervention), perceived ability to accomplish a task (self-efficacy), and social pressure (perceived views of important persons or groups), that may affect the efficacy of infection prevention measures. He also asserted that further studies should be done in different populations to identify key determinants of infection prevention behavior and methods for modifying these behaviors.
In a recent paper, Sax and Clack [44••] discussed how healthcare workers’ concepts of reality (i.e., mental models) may determine whether they implement good infection prevention practices. Sax and Clack [44••] noted that mental models are “internal images, gathered through experience and observations to collectively form an internal representation of the individual’s understanding of the world . . . .”. People use mental models as they interpret new observations and make predictions. However, mental models may not be complete or accurate representations of reality and, thus, might prevent people, including healthcare workers, from implementing beneficial practices. Sax and Clack [44••] proposed two ways to help healthcare workers create mental models that would facilitate infection prevention: (1) providing healthcare workers with experiences that optimize their “mental models regarding infection prevention and control”; (2) “designing the workplace so that it aligns with existing mental models” and facilitates safe practices. Given that microbial pathogens and the effect of hand hygiene on microbial counts are not visible to the eye and the contamination event and a related HAI are separated in time, healthcare workers may have difficulty creating correct mental models about HAI and preventive measures. Thus, Sax and Clack [44••] recommended creating educational experiences that help healthcare workers “see” the invisible, such as simulations with fluorescent markers to demonstrate how healthcare workers’ hands and clothes become contaminated during patient care, and creating policies, such as the WHO’s 5 moments for hand hygiene, that enable healthcare workers to know exactly when a specific behavior is required. Sax and Clack [44••] also suggested that designers, who understand healthcare workers’ mental models, might be able to incorporate “cues that trigger automatic behavior,” such as tape on the floor to indicate where the patient-care zone starts and ends, to improve infection prevention behavior.
In addition, infection prevention staff and other clinicians may be able to facilitate long-term compliance with infection prevention guidelines, policies, and procedures if they understand how healthcare worker’s cognitive limitations and capabilities affect their ability to comply and then write guidelines and policies and design procedures that minimize the cognitive demands associated with compliance. These demands include the conscious attention needed to do specific infection prevention tasks, the effort required to do these tasks, distractions in the environment, and overall workload. Alvarado et al. [48] used a human factors and ergonomics task analysis to assess the process of placing central venous catheters with ultrasonic guidance [49]. They found that physicians inserting these catheters were often interrupted to address issues unrelated to placing the catheters. Some interruptions caused “breaks in the primary task” and likely increased the physicians’ cognitive load by forcing them to shift their attention from their task to unrelated issues and preventing them from formulating “a complete and coherent picture of the task at hand.” [48, 49] In addition, organizational policies and practices can further strain healthcare workers’ cognitive abilities. For example when staffing levels decrease, individual healthcare worker’s workloads increase [50], which may cause these healthcare workers to eliminate steps they consider to be extra or unnecessary (i.e., take short cuts), including steps that decrease the infection risk.
Physically designing the care environment
The physical environment can substantially affect healthcare workers’ ability to implement good infection prevention measures and the physical environment itself can limit or enhance the risk of transmission. For example, healthcare workers participating in focus groups conducted by Lavender et al. [51•] noted that hand hygiene products were often placed in inconvenient or in inconsistent locations and some patient rooms did not have sinks that staff could use. In addition, numerous outbreaks of organisms such as the Coronavirus that caused Severe Acute Respiratory Syndrome (SARS) [52, 53], Pseudomonas aeruginosa [54], and Legionella pneumophila [55], in healthcare facilities have been associated with faulty design. To help prevent outbreaks and cross transmission to individual patients, persons designing new healthcare facilities or renovating and maintaining existing facilities must ensure that the physical spaces and facility design and maintenance efforts facilitate infection prevention efforts. For example, the design team must ensure that the materials used for surfaces such as walls, floors, furniture, and equipment can be cleaned and disinfected adequately such that environmental contamination and the risk of cross transmission are minimized [56].
Trudel et al. [57••] studied how the design of products and the environment in a neonatal ICU might undermine infection prevention efforts. They found multiple defective designs including high touch/contact items that were difficult to clean and maintain (e.g., door handles), spaces and objects that required “physical and cognitive effort to navigate, use or maintain,” (e.g., surfaces or equipment that could be cleaned only if healthcare workers contorted their bodies), and designs that did not remind staff when and how to perform specific infection prevention measures [57••].
The size and physical layout of a patient room determines how many patients can be cared for safely in the space and how effectively healthcare workers can navigate the space [57••, 58]. Several studies have suggested that roommates of patients infected or colonized by organisms such as methicillin-resistant Staphylococcus aureus [59, 60] vancomycin-resistant enterococci [60], or Clostridium difficile [60] are at higher risk than other patients of acquiring these organisms. A review by Ulrich et al. [58] found that HAI rates were usually lower in single-patient rooms than in multi-patient rooms. Ulrich et al. [58] also stated that single-patient rooms are easier to clean and that “single rooms with a conveniently located sink or alcohol-gel dispenser” may facilitate hand hygiene compliance compared with multi-bed rooms, where it is easy to go from patient to patient without doing hand hygiene.
A well-designed ventilation system can limit spread of organisms transmitted via airborne or droplet spread [58, 61]. Contaminated ventilation systems and those without adequate filtration or other design flaws have been the source of numerous outbreaks of infection in healthcare facilities [62,63,64]. Engineering controls, such as HEPA filters and ultraviolet (UV) lights, can prevent contamination of ventilation systems and may be required for air handling systems in specific hospital areas [65]. Knibbs et al. [66] modeled the effect of ventilation rates on the risk of influenza, tuberculosis, and rhinovirus infection in a lung function laboratory, an emergency department negative-pressure isolation room, and an outpatient consultation room. The air-exchange rates in the lung function laboratory and the isolation room “limited infection risks to 0.1%–3.6%” but the influenza risk for persons entering an outpatient consultation room after an infectious patient “departed ranged from 3.6% to 20.7%,” depending on how long the person occupied the room [66]. In addition, door type can affect the efficacy of the air handling system. For example, Julian Tang et al., [67] used water-tank models “fitted with programmable door-opening and moving human figure motions” to compare the effect of four different door designs on the ability to prevent air leakage from airborne isolation rooms. In their model, sliding doors had the lowest risk of air leakage and double-hinged doors had the highest risk of leakage and, thus, of transmission [67]. Luongo et al. [68] recently reviewed the literature on the association between ventilation systems and infection and concluded that we need well-designed observational and intervention studies that describe the characteristics of heating, ventilation, and air conditioning (HVAC) systems and measure both airborne exposures and disease outcomes.
Technology use in infection prevention and control
Many healthcare facilities have implemented “no-touch” technologies, such as hydrogen peroxide vapor or mist and UV light, for room disinfection. Each system has its own advantages and disadvantages [69•, 70•]. In general, these technologies can decrease surface contamination over large areas and they address some limitations of traditional methods in that they help disinfect hard to reach surfaces, and they often do not create toxic byproducts [71,72,73]. Moreover, they reduce microbial contamination substantially [69•, 70•] and they have been used to control outbreaks in healthcare facilities [69•]. Studies to date have demonstrated that hydrogen peroxide vapor significantly decreased acquisition of any multidrug-resistant organism [74•], that UV-C use was associated with a significantly decreased incidence of C. difficile infections [75], and that terminal room decontamination enhanced with both bleach and UV-C light significantly decreased the risk of acquiring a target organism (i.e., MRSA, VRE, or C. difficile multidrug-resistant Acinetobacter) [45]. However, these technologies are expensive and they increase the time needed for terminal room disinfection. Furthermore, hospitals should consider human factors issues associated with these technologies before implementing them [71].
The National Health Safety Network (NHSN) is supporting the development of algorithms for computerized detection of HAI [76]. Nevertheless, the results of surveys done between 2008 and 2013 found that only 23–56% [77,78,79] of respondents were using automated systems for HAI surveillance, despite well-documented benefits, including a 61% decrease in the time spent on surveillance [80] and improved implementation of isolation precautions [81]. Some infection prevention programs may have continued to do surveillance manually because their facilities did not have electronic medical records (EMR), their EMR had substantial limitations, the EMR provider did not have an HAI surveillance package, or their administration did not provide funding. However, Hebden [82•] postulated that some infection prevention programs may have been reluctant to implement electronic surveillance because of ambiguity [83] related to tasks, responsibilities, methods, expectations, and exceptions [82•]. For example, infection preventionists might experience task ambiguity because they have limited experience retrieving, managing, validating, and analyzing electronic data. In addition, infection preventionists transitioning from manual to computerized surveillance must change their workflow to fit automated surveillance processes and they will have a substantial learning curve. Consequently, Hebden [82•] recommended that formal qualitative studies be done to assess the role such human factors have in impeding implementation of electronic surveillance programs [82•].
Technology may not enhance infection prevention efforts. Verhoeven et al. [84] used HFE principles to evaluate the usability of a website that provided a guideline on MRSA control. Semi-structured interviews revealed that healthcare workers rated the website’s usability, design, and relevance positively but they questioned the website’s credibility and preferred to depend on their own knowledge and experience, or a peer’s knowledge. Additionally, they perceived “high work pressure” to be a barrier to website use [84]. The study by Verhoeven et al. [84] and the review by Hebden [82•] highlight the value of doing human factors evaluations to uncover barriers to implementation of infection prevention measures, which are often hidden and difficult to resolve.
Technology, including medical devices, computers used to access the EMR, and communication devices (e.g., cell phones, and tablets) can be contaminated [85,86,87]. Recent outbreaks of carbapenem-resistant Enterobacteriaceae related to contaminated duodenoscopes [88] and outbreaks of hepatitis B associated with blood glucose monitoring devices illustrate this point. Investigations of outbreaks associated with duodenoscopes have identified a number of human factors issues, including breaches in cleaning protocols, defects in the endoscopes, and the inherent difficulty in cleaning and disinfecting these complicated devices [88, 89]. Investigations of hepatitis B outbreaks also identified substantial human factors issues, including healthcare workers taking short cuts (did not clean and disinfect blood glucose meters between patients) and violating infection control principles (comingling contaminated and clean equipment and supplies and using single-patient finger stick devices on multiple persons) [90, 91].
Designing and using personal protective equipment
For centuries, healthcare workers have used special clothing and equipment to protect themselves from infectious diseases. Yet, we still lack basic information about the efficacy of most PPE items, optimal removal (doffing) procedures, and optimal methods for educating staff and assessing their competence [92]. PPE, particularly gloves, became important in the 1980s as healthcare workers sought to protect themselves from exposure to bloodborne pathogens, particularly hepatitis B and human immunodeficiency virus. Problems with PPE and PPE use became apparent during epidemics of SARS in 2003 and novel H1N1 influenza in 2009 [93,94,95,96,97,98,99,100,101]. Unfortunately, lessons learned from these outbreaks did not lead to sustained improvements in PPE designs or practices. Consequently, during 2014 hundreds of healthcare workers in West Africa died of Ebola because they either lacked PPE, their PPE was inadequate, or their PPE was difficult to doff safely. Moreover, PPE that was impermeable to infected fluids was extremely uncomfortable and hampered healthcare workers’ ability to care for patients [102].
Well-designed PPE should protect healthcare workers from contaminating themselves and their clothes with patients’ body fluids and infectious agents, facilitate correct donning, allow healthcare workers to work effectively and comfortably, and facilitate safe removal. The nature of the patient’s illness and the healthcare tasks will determine if healthcare workers need one PPE item (e.g., mask, respirator, or gloves) or need an entire ensemble (mask, face protection, gown, gloves, and boots). Additionally, some healthcare workers (e.g., bedside nurses) may don and doff PPE many times during a workday. Furthermore, PPE designs are not standardized and PPE items and doffing protocols were not designed or tested based on human factors principles. Thus, one should not be surprised that healthcare workers’ knowledge [103,104,105,106] about proper PPE use and their use of PPE [107, 108, 103, 106, 109,110,111,112,113,114] are suboptimal and that they contaminate themselves when they doff PPE [115,116,117,118,119,120,121,122].
Zellmer et al. [123••] observed healthcare workers removing PPE and found that only 17% removed and disposed PPE correctly. The errors Zellmer et al. [123••] observed suggested that healthcare workers likely did not know the proper order for removing PPE and that they were unaware of contaminating themselves when they use improper removal methods like rolling their gowns or gloves against their clothes or bare hands. Thus, education to improve PPE removal must help healthcare workers remove PPE items in the correct sequence and also identify subconscious actions that increase their risk of self-contamination. In addition, results of a study by Swanhorst et al. [124•] demonstrated that pictures of a proper removal sequence, which allowed healthcare workers to visualize the process, together with a written protocol helped healthcare workers don and doff a complex PPE ensemble properly.
Recent studies demonstrate the importance of using human factors principles when designing and evaluating PPE to better match the PPE to the healthcare workers’ needs and limitations, their tasks, and the environmental constraints. For example, study by AlGharmri et al. [125] found that full-face, negative pressure respirators impaired users’ motor, visual, and cognitive abilities and were associated with an increased error rate. Strauch et al. [126] put tabs on respirator straps to help healthcare workers remove these devices safely. The investigators noted that “use of the tabs was not intuitive.” Nevertheless, healthcare workers thought respirators with tabs were easier to remove than those without tabs and they were significantly less likely to contaminate themselves with a tracer when removing the respirators with tabs than those without tabs. These results suggest that the tabs may be a good addition to respirator straps but healthcare workers must be taught to use them properly [126].
Knowledge gaps and implications for future
Our literature review found that most studies in the healthcare domain explicitly applying HFE principles and methods addressed patient safety issues not infection prevention and control issues. In addition, most investigators who applied human factors principles and methods to infection prevention issues assessed only one human factors element such as training, technology evaluations, or physical environment design. The most significant gap pertains to the limited use and application of formal HFE tools and methods. Human factors engineers have developed, tested, and validated rigorous formal techniques and tools in numerous domains. However, investigators assessing usability and those assessing the physical environment were the only ones who used rigorous HFE methods to address infection prevention issues. Moreover, few investigators have evaluated the interaction among human factors variables [57••] as described by the systems engineering initiative for patient safety (SEIPS) model. This model posits that people (e.g., healthcare workers) interact in a system that includes other people, the tasks they are doing, the organization (e.g., healthcare facility), the environment, and the available technology and tools [127, 128]. Pressure or change in one portion of the system causes pressure or change in the other portions. Thus, if people designing infection prevention interventions do not take into account the effect the intervention has on all portions of the system, the interventions are likely to be ineffective. For example, if well-designed, usable hand hygiene technology is placed in a location where healthcare workers cannot see it or access it, the device will not promote use. If this device is placed where healthcare workers can see it and access it easily but they have not been trained to use it or trained when to use it, the device is unlikely to increase compliance.
Every infection prevention study need not assess all components in a system, but investigators must assess the interaction of critical system components if they want to address latent and deep-rooted human factors problems. For example, a task analysis might identify details about how and when healthcare workers do or do not practice hand hygiene, the number of hand hygiene opportunities in different clinical settings, barriers intrinsic to the hand hygiene process, inefficiencies in current workflow patterns, and design flaws that discourage healthcare workers from doing hand hygiene. Given this information about the overall system, infection prevention investigators together with frontline staff may be able to create and implement solutions that increase hand hygiene compliance and improve clinical workflow.
Numerous infection prevention studies have found that changing healthcare workers’ behavior is very difficult. Yet few investigators or infection prevention specialists have explored how to use design to promote effective infection prevention behaviors. For example, few studies address questions such as “Can we ‘design out’ barriers to compliance or could we ‘design in forcing functions or strong cues,’ that would direct healthcare workers to do the task properly?”
Human factors engineers have developed, tested, and implemented design principles to help humans change their behavior [129, 130]. For example, the proximity compatibility principle [131, 132] indicates that related products or functions should be linked by location, function, color coding, or other characteristics to direct attention and guide behavior. Examples relevant to infection prevention could include placing alcohol hand rub dispensers conveniently in the patient care area and marking the floor to demarcate clearly the patient care zone from the non-patient care zone.
HFE usability principles indicate that processes and products should be designed such that they minimize the cognitive effort healthcare workers must exert to comply or to use the product appropriately. These principles suggest that infection prevention interventions are more likely to be successful if the procedures require minimal cognitive effort and if they become automatic. Examples pertinent to infection prevention include providing central venous catheter placement kits that include each item needed to maintain sterility during placement and developing simple interventions to prevent interruptions during sterile procedures.
Ergonomic design principles indicate that equipment, technology, and processes should be designed to fit the users’ cognitive and physical capabilities and limitations. Thus, PPE should be designed to accommodate healthcare workers’ physical limitations and should be provided in sizes that facilitate patient care and healthcare worker protection. Nevertheless, manufacturers or hospitals often provide isolation gowns in a few sizes and they rarely make accommodations for healthcare workers with limited mobility. Consequently, some healthcare workers wear gowns that are too big and limit their dexterity, others wear gowns that do not provide adequate coverage, and those with limited shoulder mobility may be unable to don isolation gowns properly or to remove them without contaminating themselves.
User-centered design principles indicate that users should be included in the design, development, and evaluation phases for policies, procedures, equipment, and technology to ensure that users can use the final product in their work environment to accomplish the desired goals without causing unintended negative consequences. User-centered design principles can help infection prevention staff, administrators, or investigators develop policies, procedures, equipment, and technology that enable healthcare workers to care safely and effectively for patients without adversely affecting patient-care processes or care itself. In addition, healthcare workers may be less likely to balk when required to adopt new practices, equipment, or technology if they were included in the processes leading to the required change.
Summary
Infection prevention researchers and specialists have begun using HFE principles and methods to improve infection prevention. Yet, numerous infection prevention practices have been refractory to significant improvement and new problems and issues arise continuously as patient populations, procedures, treatments, equipment, and technology change. To ensure that their efforts are effective, infection prevention specialists and researchers should collaborate with human factors engineers and use the full complement of human factors principles and methods.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
IEA. Definition of Ergonomics. 2016. http://www.iea.cc/whats/index.html. 2016.
Welsh PM. Exploring Fraser Health’s hand hygiene culture - ProQuest. Canada: Royal Roads University; 2010.
Voss A, Widmer AF. No time for handwashing!? Handwashing versus alcoholic rub can we afford 100% compliance? Infect Control Hosp Epidemiol. 1997;18(3):205–8.
Lee A, Chalfine A, Daikos GL, Garilli S, Jovanovic B, Lemmen S, et al. Hand hygiene practices and adherence determinants in surgical wards across Europe and Israel: a multicenter observational study. Am J Infect Control. 2011;39(6):517–20. doi:10.1016/j.ajic.2010.09.007.
Pittet D. The Lowbury lecture: behaviour in infection control. J Hosp Infect. 2004;58(1):1–13. doi:10.1016/j.jhin.2004.06.002.
Pittet D, Simon A, Hugonnet SP, Pessoa-Silva CLC, Sauvan VR, Perneger TV. Hand hygiene among physicians: performance, beliefs, and perceptions. Ann Intern Med. 2004;141(1):1–8. doi:10.7326/0003-4819-141-1-200407060-00008.
• Hanh TTM, Tham NTT, Cong TC. Assessment of knowledge, attitude, factors related to hand hygiene among healthcare workers at Hung Vuong hospital. J Microbiol Immunol Infect. 2015;48(S1):S101. doi:10.1016/j.jmii.2015.02.358. Highlights knowledge and attitudes.
Dunn-Navarra A-M, Cohen B, Stone PW, Pogorzelska M, Jordan S, Larson E. Relationship between systems-level factors and hand hygiene adherence. J Nurs Care Qual. 2011;26(1):30–8. doi:10.1097/NCQ.0b013e3181e15c71.
•• Carter EJ, Wyer P, Giglio J, Jia H, Nelson G, Kauari VE, et al. Environmental factors and their association with emergency department hand hygiene compliance: an observational study. Quality and Safety in Health Care. 2016;25(5):372–8. doi:10.1136/bmjqs-2015-004081. Physical layout and compliance.
Kendall A, Landers T, Kirk J, Young E. Point-of-care hand hygiene: preventing infection behind the curtain. Am J Infect Control. 2012;40(4):S3–S10. doi:10.1016/j.ajic.2012.02.009.
Cure L, Van Enk R, Tiong E. A systematic approach for the location of hand sanitizer dispensers in hospitals. Health Care Management Science. 2013;17(3):245–58. doi:10.1007/s10729-013-9254-y.
Birnbach DJ, Nevo I, Scheinman SR, Fitzpatrick M, Shekhter I, Lombard JL. Patient safety begins with proper planning: a quantitative method to imrpove hospital design. Quality and Safety in Health Care. 2010;19(5):462–5.
Thomas BW, Berg-Copas GM, Vasquez DG, Jackson BL, Wetta-Hall R. Conspicuous vs customary location of hand hygiene agent dispensers on alcohol-based hand hygiene product usage in an intensive care unit. J Am Osteopath Assoc. 2009;109(5):263–7.
Suresh G, Cahill J. How “user friendly” is the hospital for practicing hand hygiene? An ergonomic evaluation. Joint Commission journal on quality and patient …. 2007.
• Rashidi B, Li A, Patel R, Harmsen IE, Sabri E, Kyeremanteng K, et al. Effectiveness of an extended period of flashing lights and strategic signage to increase the salience of alcohol-gel dispensers for improving hand hygiene compliance. Am J Infect Control. 2016;44(7):782–5. doi:10.1016/j.ajic.2016.01.002. Signage and salience in physical environment for compliance.
D’Egidio G, Patel R, Rashidi B, Mansour M, Sabri E, Milgram P. A study of the efficacy of flashing lights to increase the salience of alcohol-gel dispensers for improving hand hygiene compliance. Am J Infect Control. 2014;42(8):852–5. doi:10.1016/j.ajic.2014.04.017.
Whitby M, Pessoa-Silva CL, McLaws ML, Allegranzi B, Sax H, Larson E, et al. Behavioural considerations for hand hygiene practices: the basic building blocks. J Hosp Infect. 2007;65(1):1–8. doi:10.1016/j.jhin.2006.09.026.
Redelmeier DA, Shafir E. Why even good physicians do not wash their hands. Quality and Safety in Health Care. 2015;24(12):744–7. doi:10.1136/bmjqs-2015-004319.
McLaughlin AC, Anxieter GE, Hemmer AT. Nurses’ hand hygiene practices: effects of scenario, knowledge, and locus of control. Proceedings of the Human Factors and Ergonomics Society Annual Meeting. 2010;54(12):909–13. doi:10.1177/154193121005401222.
•• Lutze B, Chaberny IF, Graf K, Krauth C, Lange K, Schwadtke L, et al. Intensive care physicians’ and nurses’ perception that hand hygiene prevents pathogen transmission: belief strength and associations with other cognitive factors. J Health Psychol. 2015; doi:10.1177/1359105315595123. Knowledge regarding guidelines and beliefs on risk reduction, and its effect on compliance.
•• Conway LJ. Challenges in implementing electronic hand hygiene monitoring systems. Am J Infect Control. 2016;44(5):e7–e12. HFE issues in automated monitoring systems.
Morgan DJ, Pineles L, Shardell M, Young A, Ellingson K, Jernigan JA, et al. Automated hand hygiene count devices may better measure compliance than human observation. Am J Infect Control. 2012;40(10):955–9. doi:10.1016/j.ajic.2012.01.026.
•• Ward MA, Schweizer ML, Polgreen PM, Gupta K, Reisinger HS, Perencevich EN. Automated and electronically assisted hand hygiene monitoring systems: a systematic review. Am J Infect Control. 2014;42(5):472–8. doi:10.1016/j.ajic.2014.01.002. Systematic review of electronic and auotmated monitoring systems.
McGuckin M, Govednik J. Commentary: electronic hand hygiene compliance interventions: a descriptive guide for the infection prevention team. Am J Med Qual. 2012;27(6):540–1. doi:10.1177/1062860612439091.
Ferenc J. Handy solutions. Marketplace. 2016;07:1–6.
Sharma D, Thomas GW, Foster ED. The precision of human-generated hand-hygiene observations: a comparison of human observation with an automated monitoring system. Infection Control & …. 2012.
Swoboda SM, Earsing K, Strauss K, Lane S, Lipsett PA. Electronic monitoring and voice prompts improve hand hygiene and decrease nosocomial infections in an intermediate care unit. Crit Care Med. 2004;32:358–63.
Filho MAO, Marra AR, Magnus TP, Rodrigues RD, Prado M, de Souza Santini TR, et al. Comparison of human and electronic observation for the measurement of compliance with hand hygiene. Am J Infect Control. 2014;42(11):1188–92. doi:10.1016/j.ajic.2014.07.031.
Boscart V, Gorski S, Holliday P, Hufton G, Levchenko A, Marquez-Chin C, et al. Advanced technologies to curb healthcare-associated infections. HealthcarePapers. 2009;9(3):52–5. doi:10.12927/hcpap.2009.20927.
•• Dawson CH, Mackrill JB. Review of technologies available to improve hand hygiene compliance – are they fit for purpose? J Infect Prev. 2014;15(6):222–8. doi:10.1177/1757177414548695. Fit for purpose evaluation of automated systems.
Thomas G, Polgreen P, Herman T, Sharma D, Johns B, Chen H, et al. Improving patient safety with hand hygiene compliance monitoring. Proceedings of the Human Factors and Ergonomics Society Annual Meeting. 2011;55(1):823–7. doi:10.1177/1071181311551171.
Palmore TN, Henderson DK. Big brother is washing...Video surveillance for hand hygiene adherence, through the lenses of efficacy and privacy. Clin Infect Dis. 2011;54(1):8–9.
Boscart V, McGilton K, Levchenko A, Hufton G, Holliday P, Fernie G. Acceptability of a wearable hand wash device with monitoring capabilities. J Hosp Infect. 2008;70:216–22.
Storr J, Kilpatrick C. Improving adherence to hand hygiene practice. Nurs Times. 2012; doi:10.1163/1872-9037_afco_asc_2268.
Stewardson A, Pittet D. Anatomy of a successful multimodal hand hygiene campaign. Quality and Safety in Health Care. 2012;21(12):973–5. doi:10.1136/bmjqs-2012-001452.
Sax H, Allegranzi B, Uçkay I, Larson E, Boyce J, Pittet D. ‘My five moments for hand hygiene’: a user-centred design approach to understand, train, monitor and report hand hygiene. J Hosp Infect. 2007;67(1):9–21. doi:10.1016/j.jhin.2007.06.004.
Widmer AF, Conzelmann M, Tomic M, Frei R, Stranden AM. Introducing alcohol-based hand rub for hand hygiene: the critical need for training. Infect Control Hosp Epidemiol. 2007;28(1):50–4. doi:10.1086/510788.
•• Stewardson AJ, Iten A, Camus V, Gayet-Ageron A, Caulfield D, Lacey G, et al. Efficacy of a new educational tool to improve handrubbing technique amongst healthcare workers: a controlled. Before-After Study PLoS ONE. 2014;9(9):e105866. doi:10.1371/journal.pone.0105866. Education and hand hygiene.
Kwok YLA, Callard M, McLaws M-L. An automated hand hygiene training system improves hand hygiene technique but not compliance. Am J Infect Control. 2015;43(8):821–5. doi:10.1016/j.ajic.2015.04.201.
Gluck PA, Nevo I, Lenchus JD, Sanko JS, Everett-Thomas R, Fitzpatrick M, et al. Factors impacting hand hygiene compliance among new interns: findings from a mandatory patient safety course. Journal of Graduate Medical Education. 2010;2(2):228–31. doi:10.4300/JGME-D-09-00106.1.
Wearn A, Bhoopatkar H, Nakatsuji M. Evaluation of the effect of hand hygiene reminder signs on the use of antimicrobial hand gel in a clinical skills center. Journal of Infection and Public Health. 2015;8(5):425–31. doi:10.1016/j.jiph.2014.12.002.
de Almeida e Borges LF, Rocha LA, Nunes MJ, Filho PPG. Low compliance to handwashing program and high nosocomial infection in a Brazilian hospital. Interdisciplinary Perspectives on Infectious Diseases. 2012;2012(2):1–5. doi:10.1155/2012/579681.
• Reisinger HS, Perencevich EN, Morgan DJ, Forrest GN, Shardell M, Schweizer ML, et al. Improving hand hygiene compliance with point-of-use reminder signs designed using theoretically grounded messages. Infect Control Hosp Epidemiol. 2014;35(5):593–4. Education and hand hygiene.
•• Sax H, Clack L. Mental models: a basic concept for human factors design in infection prevention. J Hosp Infect. 2015;89(4):335–9. doi:10.1016/j.jhin.2014.12.008. Behavioral science models for infection prevention.
Anderson D, Chen LF, Weber DJ, Moehring RW, Lewis SS, Triplett PF, et al. Enhanced terminal room disinfection and acquisition and infection caused by multidrug-resistant organisms and Clostridium Difficile (the benefits of enhanced terminal room disinfection study): a cluster-randomised, multicentre, crossover study. Lancet. 2017;389(10071):805–14. doi:10.1016/S0140-6736(16)31588-4.
Clack L, Kuster SP, Giger H, Giuliani F, Sax H. Low-hanging fruit for human factors design in infection prevention—still too high to reach? Am J Infect Control. 2014;42(6):679–81. doi:10.1016/j.ajic.2014.03.002.
Clack L, Schmutz J, Manser T, Sax H. Infectious risk moments: a novel, human factors–informed approach to infection prevention. Infect Control. 2015;35(08):1051–5. doi:10.1086/677166.
Alvarado CJ, Wood K, Carayon P. Pre-implementation technology assessment of ultrasonic placement of central venous catheter insertion. Human factors in organizational design and management. Santa Monica: IEA Press; 2008.
Alvarado CJ, Wood K, Carayon P, editors. Human factors and ergonomics task analysis in ultrasonic guidance and infection control for CVC cannulation. Proceedings of the IEA 2006 Congress; 2006; Maastricht, The Netherlands. New York: Elsevier.
Vicente KJ. From patients to politicians: a cognitive engineering view of patient safety. Quality and Safety in Health Care. 2002;11(4):302–4. doi:10.1136/qhc.11.4.302.
• Lavender SA, Sommerich CM, Patterson ES, Sanders EBN, Evans KD, Park S, et al. Hospital patient room design: the issues facing 23 occupational groups who work in medical/surgical patient rooms. HERD: health environments research &. Design Journal. 2015;8(4):98–114. doi:10.1177/1937586715586391. Physical layout design and infection prevention.
Borgundvaag D, Ovens H, Goldman B, Schull M, Rutledge T, Boutis K, et al. SARS outbreak in the Greater Toronto Area: the emergency department experience. CMAJ. 2004;171(11):1342–4.
Farquharson C, Baguley K. Responding to the severe acute respiratory syndrome (SARS) outbreak: lessons learned in a Toronto emergency department. J Emerg Nurs. 2003;29(3):222–8.
Berrouane YF, McNutt LA, Buschelman BJ, Rhomberg PR, Sanford MD, Hollis RJ, et al. An outbreak of severe P. aeruginosa infections caused by a contaminated whirlpool tub drain. Clin Inf Dis. 2000;31:1331–7.
Hoepelman IM. Legionella epidemic in the Netherlands. Ned Tijdschr Geneeskd. 1999;143(23):1192–6.
Bartley J, Streifel AJ. Design of the environment of care for safety of patients and personnel: does form follow function or vice versa in the intensive care unit? Crit Care Med. 2010;38:S388–S98. doi:10.1097/CCM.0b013e3181e6d0c1.
•• Trudel C, Cobb S, Momtahan K, Brintnell J, Mitchell A. Disconnects in design and infection prevention and control—how the design of products and the environment in neonatal intensive care may be undermining infection prevention practice. Proceedings of the International Symposium on Human Factors and Ergonomics in Health Care. 2016;5(1):44–9. doi:10.1177/2327857916051011. Design of products and physical environment influences infection prevention efforts.
Ulrich R, Quan X, Zimring C, Joseph A, Choudhary R. The role of the physical environment in the 21st century: a once in a lifetime opportunity. Report to the Center for Health Design for the Designing the 21st-Century Hospital Project 2004.
Moore C, Dhaliwal J, Tong A, Eden S, Wigston C, Willey B, et al. Risk factors for methicillin-resistant Staphylococcus aureus (MRSA) acquisition in roommate contacts of patients colonized or infected with MRSA in an acute-care hospital. Infect Control Hosp Epidemiol. 2008;29(7):600–6.
Hamel M, Zoutman D, O’Callaghan C. Exposure to hospital roommates as a risk factor for healthcare–associated infection. Am J Infect Control. 2010;38:173–81.
Cole EC, Cook CE. Characterization of infectious aerosols in health care facilities: an aid to effective engineering controls and preventive strategies. American Journal of Infection Control. 1998;
Kumari DN, Haji TC, Keer V, Hawkey PM, Duncanson V, Flower E. Ventilation grilles as a potential source of methicillin-resistant Staphylococcus aureus causing an outbreak in an orthopaedic ward at a district general hospital. The Journal of Hospital Infection. 1998;39(2):127–33.
Lutz BD, Jin J, Rinaldi MG, Wickes BL, Huycke MM. Outbreak of invasive aspergillus infection in surgical patients, associated with a contaminated air-handling system. Clin Infect Dis. 2003;37(6):786–93. doi:10.1086/377537.
Fridkin SK, Kremer FB, Bland LA, Padhye A, McNeil MM, Jarvis WR. Acremonium Kiliense endophthalmitis that occurred after cataract extraction in an ambulatory surgical center and was traced to an environmental reservoir. Clin Infect Dis. 1996;22(2):222–7.
Institute FG. 2014 Hospital/Outpatient Guidelines. 2014. https://www.fgiguidelines.org/guidelines/2014-hospital-outpatient/.
Knibbs LD, Morawska L, Bell SC, Grzybowski P. Room ventilation and the risk of airborne infection transmission in 3 health care settings within a large teaching hospital. Am J Infect Control. 2011;39(10):866–72. doi:10.1016/j.ajic.2011.02.014.
Tang JW, Nicolle A, Pantelic J, Klettner CA, Su R, Kalliomaki P, et al. Different types of door-opening motions as contributing factors to containment failures in hospital isolation rooms. PLoS One. 2013;8(6):e66663. doi:10.1371/journal.pone.0066663.
Luongo JC, Fennelly KP, Keen JA, Jones BW, Miller SL. Role of mechanical ventilation in the airborne transmission of infectious agents in buildings. Indoor Air. 2016;26(5):666–78.
• Boyce JM. Modern technologies for improving cleaning and disinfection of environmental surfaces in hospitals. Antimicrob Resist Infect Control. 2016;11:5–10. doi:10.1186/s13756-016-0111-x. Technology use in infection prevention.
• Weber DJ, Rutala WA, Anderson DJ, Chen LF, Sickbert-Bennett EE, Boyce JM. Effectiveness of ultraviolet devices and hydrogen peroxide systems for terminal room decontamination: focus on clinical trials. Am J Infect Control. 2015;44(5):77–84. Technology use in infection prevention.
Davies A, Pottage T, Bennett A, Walker J. Gaseous and air decontamination technologies for Clostridium difficile in the healthcare environment. J Hosp Infect. 2011;77(3):199–203. doi:10.1016/j.jhin.2010.08.012.
Zoutman D, Shannon M, Mandel A. Effectiveness of a novel ozone-based system for the rapid high-level disinfection of health care spaces and surfaces. Am J Infect Control. 2011;39(10):873–9. doi:10.1016/j.ajic.2011.01.012.
Schneider PM. New technologies and trends in sterilization and disinfection. Am J Infect Control. 2013;41(S):S81–S6. doi:10.1016/j.ajic.2012.12.007.
• Passaretti CL, Otter JA, Reich NG, Myers J, Shepard J, Ross T, et al. An evaluation of environmental decontamination with hydrogen peroxide vapor for reducing the risk of patient acquisition of multidrug-resistant organisms. Clin Infect Dis. 2013;56(1):27–35. Technology use in infection prevention.
Pegues D, Gilmar C, Denno M, Gaynes S, editors. Reducing Clostridium difficile infection among hematology-oncology patients using ultraviolet irradiation for terminal disinfection. Abstract 1715. Abstract presented at: IDweek; 2015; San Diego.
Hebden JN. Rationale for accuracy and consistency in applying standardized definitions for surveillance of health care-associated infections. Am J Infect Control. 2012;40(5):S29–31. doi:10.1016/j.ajic.2012.03.009.
Grota PG, Stone PW, Jordan S, Pogorzelska M, Larson E. Electronic surveillance systems in infection prevention: organizational support, program characteristics, and user satisfaction. Am J Infect Control. 2010;38(7):509–14.
Halpin H, Shortell SM, Milstein A, Vanneman M. Hospital adoption of automated surveillance technology and the implementation of infection prevention and control programs. Am J Infect Control. 2011;39(4):270–6.
Masnick M, Morgan DJ, Wright M-O, Lin MY, Pineles L, Harris AD. Survey of infection prevention informatics use and practitioner satisfaction in US hospitals. Infect Control Hosp Epidemiol. 2014;35(7):891–3.
Leal J, Laupland KB. Validity of electronic surveillance systems: a systematic review. J Hosp Infect. 2008;69(3):220–9.
Larson E, Behta M, Cohen B, Jia H. Impact of electronic surveillance on isolation practices. Infect Control Hosp Epidemiol. 2013;34(7):694–9.
• Hebden JN. Slow adoption of automated infection prevention surveillance: are human factors contributing? Am J Infect Control. 2015;43(6):559–62. doi:10.1016/j.ajic.2015.02.007. Automated surveillance systems and ambiguity.
Gurses AP, Xiao Y, Seidl K, Vaidya V, Bochicchio G, editors. Systems ambiguity: A framework to assess risks and predict potential systems failures. Proceedings of the Human Factors and Ergonomics Society Annual Meeting; 2007: Human Factors and Ergonomics Society.
Verhoeven F, Steehouder MF, Hendrix RMG, van Gemert-Pijnen JEWC. Factors affecting health care workers’ adoption of a website with infection control guidelines. Int J Med Inform. 2009;78(10):663–78. doi:10.1016/j.ijmedinf.2009.06.001.
Schultz M, Gill J, Zubairi S, Huber R. Bacterial contamination of computer keyboards in a teaching hospital. Infect Control Hosp Epidemiol. 2003;24(4):302–3.
Devine J, Cooke RPD, Wright EP. Is methicillin-resistant Staphylococcus aureus (MRSA) contamination of ward-based computer terminals a surrogate marker for nococomial MRSA transmission and handwashing compliance? J Hosp Infect. 2001;48(1):72–5.
Ramesh J, Carter AO, Campbell MH, Gibbons N, Powlett C, Moseley H Sr, et al. Use of mobile phones by medical staff at Queen Elizabeth Hospital, Barbados: evidence for both beenfit and harm. J Hosp Infect. 2008;70:160–5.
CDC. https://www.cdc.gov/hai/outbreaks/cdcstatement-la-cre.html.
O’Horo JC, Farell A, Sohail MR, Safdar N. Carbapenem-resistant Enterobateriaceae and endoscopy: an evolving threat. Am J Infect Control. 2016;44(9):1032–6.
Thompson ND, Perz JF. Eliminating the blood: ongoing outbreaks of hepatitis B virus infection and the need for innovative flucose monitoring technqiues. J Diabetes Sci Technol. 2009;3(2):283–8.
Thompson ND, Schaefer MK. “Never Events”: hepatitis B outbreaks and patient notifications resulting from unsafe practices during assisted monitoring of blood glucose, 2009-2010. J Diabetes Sci Technol. 2011;5(6):1396–402.
Guideline PPEitCoFDORRA. WHO guidelines approved by the guidelines review committee. Geneva: World Health Organization; 2014.
Kilmarx PH, Clarke KR, Dietz PM, Hamel MJ, Husain F, McFadden JD, et al. Ebola virus disease in health care workers—Sierra Leone. MMWR Morb Mortal Wkly Rep. 2014;63(49):1168–71.
Seto WH, Tsang D, Yung RW, Ching TY, Ng TK, Ho M, et al. Effectiveness of precautions against droplets and contact in prevention of nosocomial transmission of severe acute respiratory syndrome (SARS). Lancet. 2003;361(9368):1519–20.
Loeb M, McGeer A, Henry B, Ofner M, Rose D, Hlywka T, et al. SARS among critical care nurses. Toronto Emerg Infect Dis. 2004;10(2):251–5.
Shears P, O’Dempsey TJ. Ebola virus disease in Africa: epidemiology and nosocomial transmission. J Hosp Infect. 2015; doi:10.1016/j.jhin.2015.01.002.
Le DH, Bloom SA, Nguyen QH, Maloney SA, Le QM, Leitmeyer KC, et al. Lack of SARS transmission among public hospital workers, Vietnam. Emerg Infect Dis. 2004;10(2):265–8.
Yeom JS, Lee JH, Bae IG, Oh WS, Moon CS, Park KH, et al. H1N1 influenza infection in Korean healthcare personnel. Eur J Clin Microbiol Infect Dis. 2009;30(10):1201–6.
Lee V, Yap J, Cook AR, Chen M, Tay J, Barr I, et al. Effectiveness of public health measures in mitigating pandemic influenza spread: a prospective sero-epidemiological cohort study. J Infect Dis. 2010;202(9):1319–26.
Cowling BJ, Chan KH, Fang VJ, Cheng CK, Fung RO, Wai W, et al. Facemasks and hand hygiene to prevent influenza transmission in households: a cluster randomized trial. Ann Intern Med. 2009;151(7):437–46.
Loeb M, Dafoe N, Mahony J, John M, Sarabia A, Glavin V, et al. Surgical mask vs N95 respirator for preventing influenza among health care workers: a randomized trial. JAMA. 2009;302(17):1865–71.
Verbeek JH, Ijaz S, Mischke C, Ruotsalainen JH, Makela E, Neuvonen K et al. Personal protective equipment for preventing highly infectious diseases due to contact with contaminated body fluids in health care staff. Cochrane Database Syst Rev. 2015.
Daugherty EL, Perl TM, Needham DM, Rubinson L, Bilderback A, Rand CS. The use of personal protective equipment for control of influenza among critical care clinicians: a survey study. Crit Care Med. 2009;37(4):1210–6.
Reid SM, Farion KJ, Suh KN, Audcent T, Barrownman NJ, Plint AC. Use of personal protective equipment in Canadian pediatric emergency departments. CJEM. 2011;13(2):71–8.
Hu X, Zhang Z, Li N, Liu D, Zhang L, He W, et al. Self-reported use of personal protective equipment among Chinese critical care clinicians during 2009 H1N1 influenza pandemic. PLoS One. 2012;7(9):e44723.
Watson CM, Duval-Arnould JM, McCrory MC, Froz S, Connors C, Perl TM, et al. Simulated pediatric resuscitation use for personal protective equipment adherence measurement and training during the 2009 influenza (H1N1) pandemic. Jt Comm J Qual Patient Saf. 2011;37(11):515–23.
Jaeger JL, Patel M, Dharan N, Hancock K, Meites E, Mattson C, et al. Transmission of 2009 pandemic influenza a (H1N1) virus among healthcare personnel-Southern California, 2009. Infect Control Hosp Epidemiol. 2011;32(12):1149–57.
Banach DB, Bielang R, Calfee DP. Factors associated with unprotected exposure to 2009 H1N1 influenza a among healthcare workers during the first wave of the pandemic. Infect Control Hosp Epidemiol. 2011;32(3):293–5.
Phin NF, Rylands AJ, Allan J, Edwards C, Enstone JE, Nguyen-Van-Tam JS. Personal protective equipment in an influenza pandemic: a UK simulation exercise. J Hosp Infect. 2009;71(1):15–21.
Parker MJ, Goldman RD. Paediatric emergency department staff perceptions of infection control measures against severe acute respiratory syndrome. Emerg Med J. 2006;23(5):349–53.
Shigayeva A, Green K, Raboud JM, Henry B, Simor AE, Vearncombe M, et al. Factors associated with critical-care healthcare workers’ adherence to recommended barrier precautions during the Toronto severe acute respiratory syndrome outbreak. Infect Control Hosp Epidemiol. 2007;28(11):1275–83.
Swaminathan A, Martin R, Gamon S, Aboltins C, Athan E, Braitberg G, et al. Personal protective equipment and antiviral drug use during hospitalization for suspected avian or pandemic influenza. Emerg Infect Dis. 2007;13(10):1541–7.
Casanova LM, Rutala WA, Weber DJ, Sobsey MD. Effect of single- versus double-gloving on virus transfer to health care workers’ skin and clothing during removal of personal protective equipment. Am J Infect Control. 2012;40(4):369–74.
Yap FH, Ho PL, Joynt GM. Reply to Bassetti et al. Clin Infect Dis. 2005;40(4):634–5.
Beam EL, Gibbs SG, Boulter KC, Beckerdite ME, Smith PW. A method for evaluating health care workers’ personal protective equipment technique. Am J Infect Control. 2011;39(5):415–20.
Zamora JE, Murdoch J, Simchison B, Day AG. Contamination: a comparison of 2 personal protective systems. CMAJ. 2006;175(3):249–54.
Rawson BV, Cocker J, Evans PG, Wheeler JP, Akrill PM. Internal contamination of gloves: routes and consequences. Ann Occup Hyg. 2005;49(6):535–41.
Wong TK, Chung JW, Li Y, Chan WF, Ching PT, Lam CH, et al. Effective personal protective clothing for health care workers attending patients with severe acute respiratory syndrome. Am J Infect Control. 2004;32(2):90–6.
Guo YP, Li Y, Wong PL. Environment and body contamination: a comparison of two different removal methods in three types of personal protective clothing. Am J Infect Control. 2014;42(4):e39–45.
Beam EL, Gibbs SG, Hewlett AL, Iwen PC, Nuss SL, Smith PW. Method for investigating nursing behaviors related to isolation care. Am J Infect Control. 2014;42(11):1152–6.
Tomas M, Kundrapu S, Thota P, Sunkesula V, Cadnum J, Mana T, et al. Frequent contamination of the skin and clothing of healthcare personnel during removal of personal protective equipment: a multicenter evaluation and educational intervention. Orlando: SHEA Spring 2015: Science Guiding Prevention; 2015.
Casanova LM, Alfano-Sobsey E, Rutala WA, Weber DJ, Sobsey M. Virus transfer from personal protective equipment to healthcare employees’ skin and clothing. Emerg Infect Dis. 2008;14(8):1291–3.
•• Zellmer C, Van Hoof S, Safdar N. Variation in health care worker removal of personal protective equipment. Am J Infect Control. 2015;43(7):750–1. doi:10.1016/j.ajic.2015.02.005. PPE doffing sequence and education.
• Swanhorst J, Boulter K, Vasa A, Boeckman B, Schwedhelm M. A detailed instructional process for donning and doffing level C personal protective equipment in a healthcare setting. Am J Infect Control. 2014;42(6):S93. doi:10.1016/j.ajic.2014.03.211. PPE doffing sequence and education.
AlGhamri AA, Murray SL, Samaranayake VA. The effects of wearing respirators on human fine motor, visual, and cognitive performance. Ergonomics. 2013;56(5):791–802. doi:10.1080/00140139.2013.767383.
Strauch AL, Brady TM, Niezgoda G, Almaguer CM, Shaffer RE, Fisher EM. Assessing the efficacy of tabs on filtering facepiece respirator straps to increase proper doffing techniques while reducing contact transmission of pathogens. J Occup Environ Hyg. 2016;13(10):794–801. doi:10.1080/15459624.2016.1179386.
Smith MJ, Carayon-Sainfort P. A balance theory of job design for stress reduction. Int J Ind Ergon. 1989;4:67–79.
Carayon P, Smith MJ. Work organization and ergonomics. Appl Ergon. 2000;31(6):649–62.
Wickens CD, Gordon SE, Liu Y, Lee J. An introduction to human factors engineering. 1998.
Wickens C. The multiple resources model of human performance: Implications for display design: DTIC Document 1984.
Wickens CD, Andre AD. Proximity compatibility and information display: effects of color, space, and objectness on information integration. Human Factors: The Journal of the Human Factors and Ergonomics Society. 1990;32(1):61–77.
Wickens CD, Carswell CM. The proximity compatibility principle: its psychological foundation and relevance to display design. Hum Factors. 1995;37(3):473–94.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Priyadarshini R. Pennathur and Dr. Loreen A. Herwaldt were supported by a grant from The Centers for Disease Control and Prevention CK000448-02 to conduct this work. Dr. Pennathur was also supported by a grant from the National Library of Medicine, NIH (5R00 LM0111384-03).
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on New Technologies and Advances in Infection Prevention
Rights and permissions
About this article
Cite this article
Pennathur, P.R., Herwaldt, L.A. Role of Human Factors Engineering in Infection Prevention: Gaps and Opportunities. Curr Treat Options Infect Dis 9, 230–249 (2017). https://doi.org/10.1007/s40506-017-0123-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40506-017-0123-y