Abstract
Purpose of Review
This review aims to summarize the literature on biomaterials used as scaffolds, focusing on strategies for tooth tissue engineering, ideal requirements, and classifications of scaffold biomaterials.
Recent Findings
Biomaterials have a significant influence in the arena of tooth tissue engineering. The involvement of biomaterial scaffolds in tissue regeneration is essential, as they provide a porous framework or a carrier for stem cells and/or growth factor delivery to the pivotal target site. Many natural and synthetic biomaterials could be used to serve as scaffolds for tooth tissue engineering.
Summary
Nanotechnology and surface coating technology, together with advancement of biomaterial bioactivity and biomimicry, have a great influence in cellular response, rate of tissue healing, and finally long-term success of tissue engineering treatment. A limitation of the current study is mainly due to a lack of clinical trials.




Similar content being viewed by others
Data Availability
All data generated or analyzed during this study are included in this published article.
Abbreviations
- MSCs:
-
Mesenchymal stem cells
- EMD:
-
Enamel matrix derivative
- rh-PDGF-BB:
-
Recombinant human platelet-derived growth factor BB
- FGF-2:
-
Fibroblast growth factor 2
- GDF-5:
-
Growth and differentiation factor 5
- BMPs:
-
Bone morphogenic proteins
- DPSCs::
-
Dental pulp stem cells
- ECM:
-
Extracellular matrix
- 3D:
-
Three dimensional
- PLA:
-
Polylactic acid
- PCL:
-
Polycaprolactone
- PGA:
-
Polyglycolic acid
- PLGA:
-
Polylactic-co-glycolic acid
- PMMA:
-
Polymethylmethacrylate
- PTFE:
-
Polytetrafluoroethylene
- ACP:
-
Amorphous calcium phosphate
- OCP:
-
Octacalcium phosphate
- α-TCP:
-
α-Tricalcium phosphate
- β-TCP:
-
β-Tricalcium phosphate
- CDHA:
-
Calcium-deficient hydroxyapatite
- HA:
-
Hydroxyapatite
- TTCP:
-
Tetracalcium phosphate
- TCP:
-
Tricalcium phosphate
- BAG:
-
Bioactive glass
- CAD/CAM:
-
Computer-aided design and computer-aided manufacturing
- AgNPs:
-
Silver nanoparticles
- QPS:
-
Quaternary pyridinium salts
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Grawish ME, Grawish LM, Grawish HM, et al. Challenges of engineering biomimetic dental and paradental tissues. Tissue Eng Regen Med. 2020;17:403–21.
Hu L, Liu Y, Wang S. Stem cell-based tooth and periodontal regeneration. Oral Dis. 2018;24:696–705.
Hamdy TM. Polymers and ceramics biomaterials in Orthopedics and dentistry: a review article. Egypt J Chem. 2018;61:723–30.
Pereira HF, Cengiz IF, Silva FS, et al. Scaffolds and coatings for bone regeneration. J Mater Sci: Mater Med. 2020;31:27–42
Hamdy TM. Interfacial microscopic examination and chemical analysis of resin-dentin interface of self-adhering flowable resin composite. F1000Research. 2017;6:1688–99
Stratton S, Shelke NB, Hoshino K, et al. Bioactive polymeric scaffolds for tissue engineering. Bioact Mater. 2016;1:93–108.
Kumar P, Keerthi KL, Jayasri D, et al. Biodontics: a new paradigm in dentistry. Dent Hypotheses. 2021;12:47–9.
Matichescu A, Ardelean LC, Rusu LC, et al. Advanced biomaterials and techniques for oral tissue engineering and regeneration—a review. Mater. 2020;13:1–37.
Sharma S, Srivastava D, Grover S, et al. Biomaterials in tooth tissue engineering: a review. J Clin Diagn Res. 2014;8:309–15.
Ahmed GM, Abouauf EA, Abubakr N, et al. Tissue engineering approaches for enamel, dentin, and pulp regeneration: an update. Stem Cells Int. 2020;25:1–15
Smith EE, Angstadt S, Monteiro N, et al. Bioengineered tooth buds exhibit features of natural tooth buds. J Dent Res. 2018;97:1144–51.
Dave JR, Tomar GB. Dental tissue–derived mesenchymal stem cells: applications in tissue engineering. Crit Rev Biomed Eng. 2018;46:429–68.
Galli M, Yao Y, Giannobile W V., et al. Current and future trends in periodontal tissue engineering and bone regeneration. Plast Aesthetic Res. 2021;8:3,1–29
Bowler D, Dym H. Bone morphogenic protein: application in implant dentistry. Dent Clin North Am. 2015;59:493–503.
Xu C, Liu H, Yang H, et al. A green biocompatible fabrication of highly porous functional ceramics with high strength and controllable pore structures. J Mater Sci Technol. 2016;32:729–32.
Amrollahi P, Shah B, Seifi A, et al. Recent advancements in regenerative dentistry: a review. Mater Sci Eng C. 2016;69:1383–90.
Zafar MS, Amin F, Fareed MA, et al. Biomimetic aspects of restorative dentistry biomaterials. Biomimetics. 2020;5:1–42.
• Nikolova MP, Chavali MS. Recent advances in biomaterials for 3D scaffolds: a review. Bioact Mater. 2019;4:271–92. This comprehensive literature review discusses the future outlook for the development of bioactive scaffolds.
Malhotra N, Kundabala M, Acharya S. Current strategies and applications of tissue engineering in dentistry--a review Part 2. Dental update. 2009;36:577–82.
Eliaz N, Metoki N. Calcium phosphate bioceramics: a review of their history, structure, properties, coating technologies and biomedical applications. Mater (Basel). 2017;10:334–40.
Wu X, Walsh K, Hoff BL, et al. Mineralization of biomaterials for bone tissue engineering. Bioeng. 2020;7:1–24.
Hamdy T. Polymerization shrinkage in contemporary resin-based dental composites: a review article. Egypt J Chem. 2021;64:3087–92.
Fernandes HR, Gaddam A, Rebelo A, et al. Bioactive glasses and glass-ceramics for healthcare applications in bone regeneration and tissue engineering. Mater (Basel). 2018;11:2530.
•• Jazayeri HE, Lee SM, Kuhn L, et al. Polymeric scaffolds for dental pulp tissue engineering: a review. Dent Mater. 2020;36:e47–58. This recently published review article presented the fundamental use of biomaterial scaffolds and stem cells for safe and potent regeneration of pulp tissue and reestablishment of tooth vitality.
Virlan MJR, Miricescu D, Totan A, et al. Current uses of poly(lactic-co-glycolic acid) in the dental field: a comprehensive review. J Chem. 2015;2015:1–15.
Aboulgheit S, Abdelkader S, Aboushelib M, et al. Collagen chitosan scaffolds on induced skin defect in a rat model (an experimental study). Alexandria Dent J. 2021;0:0–0.
Abdelraouf RM. Chemical analysis and microstructure examination of extended-pour alginate impression versus conventional one (characterization of dental extended-pour alginate). Int J Polym Mater Polym Biomater. 2018;67:612–8.
De Olyveira GM, Dos Santos ML, Manzine Costa LM, et al. Bacterial cellulose nanobiocomposites for dental materials scaffolds. J Biomater Tissue Eng. 2014;4:536–42.
Abdelraouf RM, Bayoumi RE, Hamdy TM. Effect of powder/water ratio variation on viscosity, tear strength and detail reproduction of dental alginate impression material (in vitro and clinical study). Polym (Basel). 13. 2021;13:2923–34.
Hamdy TM, Mousa SMA, Sherief MA. Effect of incorporation of lanthanum and cerium-doped hydroxyapatite on acrylic bone cement produced from phosphogypsum waste. Egypt J Chem. 2020;63:1823–32.
Hamdy TM, Saniour SH, Sherief MA, et al. Effect of incorporation of 20 wt% amorphous nano-hydroxyapatite fillers in poly methyl methacrylate composite on the compressive strength. Res J Pharm Biol Chem Sci. 2015;6:1136–41.
Gangapurwala G, Vollrath A, De San LA, et al. PLA/PLGA-based drug delivery systems produced with supercritical CO2—a green future for particle formulation? Pharm. 2020;12:1–26.
Fabricky MMC, Gabor AG, Milutinovici RA, et al. Scaffold-type structure dental ceramics with different compositions evaluated through physicochemical characteristics and biosecurity profiles. Mater (Basel). 14. 2021;14:2266–84.
Zaki DY, Zaazou MH, Khallaf ME, et al. In vivo comparative evaluation of periapical healing in response to a calcium silicate and calcium hydroxide based endodontic sealers. Open Access Maced J Med Sci. 2018;6:1475–9.
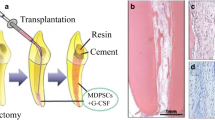
Uchikawa E, Yoshizawa M, Li X, et al. Tooth transplantation with a β-tricalcium phosphate scaffold accelerates bone formation and periodontal tissue regeneration. Oral Dis. 2021;27:1226–37.
Hamdy TM, Saniour SH, Sherief MA, et al. Effect of incorporation of 20 wt% amorphous nano-hydroxyapatite fillers in poly methyl methacrylate composite on the compressive strength. Res J Pharm Biol Chem Sci. 2015;6:975–8585.
Guillen-Romero LD, Oropeza-Guzmán MT, López-Maldonado EA, et al. Synthetic hydroxyapatite and its use in bioactive coatings. J Appl Biomater Funct Mater. 2019;7:1–12.
Li Z, Chu D, Gao Y, et al. Biomimicry, biomineralization, and bioregeneration of bone using advanced three-dimensional fibrous hydroxyapatite scaffold. Mater Today Adv. 2019;31–10.
Hamdy TM, El-Korashy SA. Novel bioactive zinc phosphate dental cement with low irritation and enhanced microhardness. e-Journal Surf Sci Nanotechnol 2018;16:431–36.
van Vugt TA, Geurts JAP, Arts JJ, et al. Biomaterials in treatment of orthopedic infections. In: Management of Periprosthetic Joint Infections (PJIs). 2017;2017:41–68.
Skallevold HE, Rokaya D, Khurshid Z, et al. Bioactive glass applications in dentistry. Int J Mol Sci. 2019;20(23):5690.
Abdelnabi A, Hamza MK, El-Borady OM, et al. Effect of different formulations and application methods of coral calcium on its remineralization ability on carious enamel. Open Access Maced J Med Sci. 2020;8:94–9.
Olaru M, Sachelarie L, Calin G. Hard dental tissues regeneration—approaches and challenges. Mater. 2021;14:2558–93.
Sergi R, Bellucci D, Cannillo V. A review of bioactive glass/natural polymer composites: state of the art. Mater. 2020;13:1–38.
Shi YZ, Liu J, Yu L, et al. β-TCP scaffold coated with PCL as biodegradable materials for dental applications. Ceram Int. 2018;44:15086–91.
Sadeghinia A, Davaran S, Salehi R, et al. Nano-hydroxy apatite/chitosan/gelatin scaffolds enriched by a combination of platelet-rich plasma and fibrin glue enhance proliferation and differentiation of seeded human dental pulp stem cells. Biomed Pharmacother. 2019;109:1924–31.
Aboushelib MN, Shawky R. Osteogenesis ability of CAD/CAM porous zirconia scaffolds enriched with nano-hydroxyapatite particles. Int J Implant Dent. 2017;3:21–27.
Hammad HGH, Salama MNF. Porosity pattern of 3D chitosan/bioactive glass tissue engineering scaffolds prepared for bone regeneration. Open Dent J. 2021;15:41–56.
Spicer CD. Hydrogel scaffolds for tissue engineering: the importance of polymer choice. Polym Chem. 2020;11:184–219.
Samiei M, Fathi M, Barar J, et al. Bioactive hydrogel-based scaffolds for the regeneration of dental pulp tissue. J Drug Deliv Sci Technol. 2021;64:1–12.
Diogenes A, Ruparel NB, Shiloah Y, et al. Regenerative endodontics a way forward. J Am Dent Assoc. 2016;147:372–80.
Alipour M, Firouzi N, Aghazadeh Z, et al. The osteogenic differentiation of human dental pulp stem cells in alginate-gelatin/Nano-hydroxyapatite microcapsules. BMC Biotechnol. 2021;2:6–16.
Funda G, Taschieri S, Bruno GA, et al. Nanotechnology scaffolds for alveolar bone regeneration. Mater. 2021;13:201–21.
Zhu L, Luo D, Liu Y. Effect of the nano/microscale structure of biomaterial scaffolds on bone regeneration. Int J Oral Sci. 2020;12:6–21.
Amani H, Arzaghi H, Bayandori M, et al. Controlling cell behavior through the design of biomaterial surfaces: a focus on surface modification techniques. Adv Mater Interfaces. 2019;6:1–31.
Mehdikhani-Nahrkhalaji M, Fathi MH, Mortazavi V, et al. Biodegradable nanocomposite coatings accelerate bone healing: in vivo evaluation. Dent Res J (Isfahan). 2015;12:89–99.
Zhang K, Wang S, Zhou C, et al. Advanced smart biomaterials and constructs for hard tissue engineering and regeneration. Bone Res. 2018;6:31–46.
Pfau MR, Grunlan MA. Smart scaffolds: shape memory polymers (SMPs) in tissue engineering. J Mater Chem B. 2021;9:4287–97.
Acknowledgements
The authors are grateful to Professor Roger Watson, Professor of Nursing, Faculty of Health Sciences, University of Hull, UK, for his support and help through English editing.
Author information
Authors and Affiliations
Contributions
T. M. Hamdy contributed to the conception and design of the review, collection of data, interpretation of the analyzed data, writing the manuscript, revised and reviewed the draft manuscript, and read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hamdy, T.M. Dental Biomaterial Scaffolds in Tooth Tissue Engineering: a Review. Curr Oral Health Rep 10, 14–21 (2023). https://doi.org/10.1007/s40496-023-00329-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40496-023-00329-0