Abstract
The discovery of immune checkpoint inhibitors (ICIs) such as programmed cell death protein 1 (PD-1) inhibitors, nivolumab and pembrolizumab, and programmed cell death ligand 1 (PD-L1) inhibitors, atezolizumab and durvalumab, has revolutionized the treatment of advanced non-small cell lung cancer (NSCLC). Concurrent radiotherapy (RT) is of particular interest with regard to the potential role for this combination in many settings. The purpose of this commentary is to evaluate the potential for the combination of immune checkpoint inhibitors and radiotherapy, including analysis of studies that have considered this combination in various settings.
Similar content being viewed by others
Commentary
Immunotherapy in patients with advanced non-small cell lung cancer (NSCLC) has revolutionized the treatment of the disease in many settings. Radiotherapy, for both cytoreductive and palliative purposes, remains a powerful weapon for patients with stage IIIB and IV NSCLC.
The effect of ionizing radiation on tumor cells and on the microenvironment, inducing the presentation of tumor antigens on dendritic cells in order to stimulate the response of the immune adaptive system, has garnered particular interest during this period, especially considering the potential combined activity with immunotherapy [1].
There is a strong rationale for combining radiotherapy and immune checkpoint inhibitors. RT enhances the expression of major histocompatibility complex I (MHC I) on the surface of tumor cells, which promotes immunogenic tumor cell death [2]. Otherwise, the tumor is normally characterized by an immune-suppressive microenvironment. Up-regulated expression of immune checkpoint ligands in tumor cells is a known immune resistance mechanism [3]. The same radiation treatment can up-regulate programmed cell death ligand 1 (PD-L1), PD-L2, and cytotoxic T-lymphocyte antigen 4 (CTLA4), favoring the effect of specific antibodies [4]. Furthermore, tumors can resist immune elimination by up-regulating the expression of PD-1 on tumor-specific regulator lymphocytes that consequently inhibit anti-tumor immune responses [5].
Radiotherapy can mediate both negative and positive effects on the tumor. It can recruit immunosuppressive myeloid cells that directly promote tumor growth, contributing to an immunosuppressive environment by causing T cells to become dysfunctional [6,7,8]. On the other hand, a positive abscopal effect (i.e. the regression of metastases outside the radiation field) can be mediated by boosting T cells against the tumor, as observed in mice by combining local radiation with growth factors for dendritic cells [9]. This abscopal effect appears to be related to the biologically effective radiation dose [10]. The effects of RT and ICIs have been investigated in many preclinical studies. Deng et al. [8] demonstrated that PD-L1 was up-regulated in the tumor microenvironment after RT. Administration of anti-PD-L1 improved the efficacy of RT through a cytotoxic T cell-dependent mechanism, suppressing the accumulation of tumor-infiltrating myeloid-derived suppressor cells (MDSC). Furthermore, reduction in MDSC also appeared to be caused by tumor necrosis factor (TNF), possibly derived from the activation of cytotoxic T cells by the RT-ICI combination itself.
Several immune response modifiers, including interleukin-2 (IL-2), have demonstrated synergistic anti-tumor effects with RT [11]. Some studies have shown positive outcomes in mouse models with RT and cytokines including IL-3, IL-12, and TNF [12, 13]; however, the clinical use of these combinations has been limited due to interleukin toxicity. A role for Flt3-L growth factor in inducing anti-tumor immunity in mouse tumors has been reported. Concomitant RT (60 Gy) prevented the development of lung metastases and improved disease-free survival compared to RT or Flt3-L alone. However, the high single radiation dose has limited clinical feasibility [14, 15].
The combination of radiation therapy and CTLA-4 blockade (9H10 monoclonal antibody anti CTLA-4) has been tested in a metastatic mouse mammary carcinoma 4T1 model: mice treated with radiation and 9H10 monoclonal antibody had improved survival, which was associated with fewer lung metastases, likely related to an immune-mediated abscopal effect. [16].
It is important to consider that, in addition to the effects of RT on the microenvironment and on the release of tumor-specific antigens for T-cell recognition, RT also has immunosuppressive effects. In fact, RT of pancreatic cancers in mice resulted in a higher proportion of activated macrophages with immunosuppressive phenotypes and increased recruitment of T cells with regulatory phenotypes [7]. However, treatment with macrophage colony-stimulating factor 1 (m-CSF) blockade has been shown to partially reduce the immunosuppressive effect of RT [16]. Radiation also increases CCL2 chemokine production, causing recruitment of Ly6C+/CCR2+ monocytes that enhance cancer proliferation and neoangiogenesis. This mechanism can be prevented by combining RT with an anti-CCL2 antibody. In a study on murine lung cancer, the combination of NHS-IL2, an antibody specific for necrotic DNA fused to modified human IL-2, and cisplatin (CDDP) with RT was more effective than control [17].
These preclinical studies have shown how important the combination of RT and immune response modifiers can be, some of which have been subsequently investigated in clinical trials.
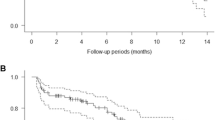
Our observation of increased survival with combined radiotherapy and immunotherapy in lung cancer patients is in line with these preclinical data [18]. In particular, 20% of our patients (all highly pretreated) are still reporting disease control after long-term follow-up. Two patients received stereotactic radiation treatment on pulmonary lesions. One of these patients developed radio-induced interstitiopathy requiring discontinuation of treatment with nivolumab for more than 3 months, but maintained stable disease even without immunotherapy. The other patient received palliative radiation on the mediastinum (36 Gy in 12 fractions) before ICI. In our series, the best results in terms of both overall survival (OS) and progression-free survival (PFS) have been achieved in patients who received combined treatment comprising immunotherapy and stereotactic RT on primary pulmonary lesions. This scenario is actually evaluated in some clinical trials, such as the randomized I-SABR study, which explores the addition of nivolumab to stereotactic radiotherapy in early lung cancer and solitary pulmonary metastases, and the PembroX phase II trial, in which patients with NSCLC planned for surgical resection (stages I–IIIA) are randomized to preoperative pembrolizumab alone or pembrolizumab and radiotherapy with a single stereotactic fraction of 12 Gy delivered to 50% of the primary tumor.
Many other studies have been conducted or are currently ongoing to evaluate concurrent radiation-immunotherapy and sequential radiation-immunotherapy in different tumor settings (Table 1).
Preliminary results have been reported for some of these trials. In a phase Ib trial, a necrotic DNA-specific antibody conjugated with a modified human IL-2 (NHS-IL2) has been investigated in NSCLC patients who achieved disease control after first-line platinum-based chemotherapy for metastatic disease, in combination with palliative radiotherapy to the primary tumor or metastasis (20 Gy in five daily fractions): a median PFS of 2.9 months and median OS of 8.6 months were reported [17]. In another phase II trial, patients with chemo-refractory advanced NSCLC were treated with anti-CTLA4 ipilimumab within 24 h of starting palliative radiotherapy to at least one metastatic lesion (30 Gy in five fractions), with two achieving complete response, three with stable disease or partial response, and seven with disease progression, with significant toxicity [19]. The combination of recombinant MAGE-3 protein and radiotherapy in patients with unresectable stage III NSCLC was investigated in one of four study cohorts; in this cohort the patients were treated with at least two cycles of chemotherapy followed by sequential radiotherapy and then MAGE-A3 immunotherapy [20]. A phase III trial studied the role of adjuvant MAGE-A3 in resected NSCLC without prolongation of disease-free survival compared to placebo. Tecemotide (L-BLP25) is the best-studied immunotherapeutic agent that has been administered with chemoradiotherapy. Tecemotide is a mucin 1-specific immunotherapy and is a synthetic peptide designed to induce T-cell responses to the mucin 1 that is expressed on the surface of tumors [21, 22].
The results of a phase III trial comparing maintenance tecemotide with placebo in stage IIIB/IV patients who had not progressed on either prior chemotherapy or chemoradiotherapy offer insights into the interplay between radiation and immunotherapy [23]. The trial did not demonstrate improvement in median OS between the maintenance and placebo arms; however, it did suggest that the patients randomized to tecemotide within 12 weeks of completing first-line treatment had better rates of OS than those on placebo. Moreover, patients who received radiation as part of first-line treatment prior to tecemotide also saw an OS advantage. The phase III START trial randomized patients with stage IIIA or IIIB NSCLC in a 2:1 fashion to receive placebo or tecemotide in the maintenance setting following the completion of concurrent or sequential chemotherapy and radiation [24]. The authors determined that tecemotide was not associated with an OS benefit in the general population of unresectable stage III patients; however, the trial did show a benefit for patients receiving concurrent chemoradiotherapy.
However, the most important results have been reported from the PACIFIC trial, which was the first study to show a clear benefit for the integration of immunotherapy with concurrent chemoradiotherapy [25]. The PACIFIC trial was a phase III double-blind randomized placebo-controlled trial. Patients who did not progress following definitive platinum-based chemotherapy (≥ 2 cycles) concurrently with radiotherapy were enrolled. Patients were randomized in a 2:1 fashion to 10 mg/kg of durvalumab (PDL-1 inhibitor) every 2 weeks versus a similarly administered placebo. The median PFS was 5.6 months in the placebo arm and 16.8 months in the durvalumab arm. In addition to the impressive PFS data, the objective response rate (ORR) was significantly higher in the durvalumab arm than in the placebo arm (28.4 versus 16%, respectively; P = 0.001). Responses in the placebo group were attributed to continued tumor regression following radiotherapy. Treatment with durvalumab also reduced the incidence of progression with brain metastases. On the basis of this trial, durvalumab was approved by the US Food and Drug Administration for use as a maintenance therapy following the completion of platinum-based chemoradiation in unresectable lung cancer [26]. In December 2018, Antonia et al. published updated results for the PACIFIC study, which showed a 24-month OS rate of 66.3% in the durvalumab group, compared with 55.6% in the placebo group. Durvalumab significantly prolonged OS as compared with placebo (stratified hazard ratio for death, 0.68; 99.73% CI, 0.47–0.997; P = 0.0025). Updated analyses regarding PFS were similar to those previously reported, with a median duration of 17.2 months in the durvalumab group and 5.6 months in the placebo group [27].
Other ICIs have also been used in combination with RT. Concurrent atezolizumab (PD-L1 inhibitor) and chemoradiation followed by atezolizumab consolidation and maintenance was found to be safe and showed promising efficacy in patients with locally advanced non-small cell lung cancer in the phase II DETERRED trial. In part I of this single-institution study, 10 patients underwent chemoradiation therapy (CRT) with low-dose carboplatin/paclitaxel followed by high-dose consolidation chemotherapy plus atezolizumab and atezolizumab maintenance for 1 year. Six patients in this group (60%) experienced grade 3 or higher adverse events (AEs). In part II of the study, 30 patients received concurrent atezolizumab and CRT followed by the same consolidation and maintenance used in part I, and 17 (57%) experienced grade 3 or higher AEs. Preliminary survival data showed median PFS of 20.1 months in part I, whereas PFS was not reached in part II. Median OS at 1 year was 60 and 77% in parts I and II, respectively. Grade 3 or higher AEs were associated with atezolizumab in 30 and 23% of patients in parts I and part II, respectively. Grade 2 radiation pneumonitis was seen in two patients in each group [28]. A comparison of the regimens used in the DETERRED and PACIFIC trials is planned.
Results of the phase II LUN14-179 trial of consolidation pembrolizumab following concurrent CRT in patients with unresectable stage III NSCLC were recently published. The primary endpoint was time to metastatic disease or death (TMDD). Median TMDD was not reached, but the estimates of 1-year and 2-year OS were 80.5 and 68.7%, respectively. Median PFS was 15.4 months, while 12-, 18-, and 24-month PFS were 59.9, 49.5, and 45.4%, respectively. Sixteen (17.2%) patients developed grade 2 or higher pneumonitis, with five (5.4%) experiencing grade 3/4 pneumonitis. Consolidation pembrolizumab following CRT substantially improved TMDD and PFS compared with historical controls. Preliminary OS data are promising and suggest a substantial improvement in outcomes for patients with stage III NSCLC [29].
The success of ICIs in NSCLC has opened the door to studies combining immunotherapy with radiation, which remains an important weapon against locally advanced and metastatic disease. Although the preclinical studies have expanded our knowledge regarding the interaction of RT and ICI with the tumor microenvironment, it is difficult to translate these new data to the clinical setting. The mechanisms inducing the synergistic effect of RT and immunotherapy are not completely elucidated, and much effort is needed on this front. Based on the results published thus far, the safety of the combination is not a limiting factor, but the potential risk of pneumonitis in patients treated with combined RT and ICIs seems to be an important consideration.
Many studies are evaluating the role of biomarkers such as PD-L1 or tumor mutational burden (TMB) in defining molecular predictors of response. The evaluation of factors derived from both the tumor microenvironment and the immune system as proxies of treatment efficacy could be important. The dynamic nature of immune functioning and response suggests the need for dynamic testing as well, such as repeated biopsies during combination treatment.
In conclusion, the integration of immunotherapy and radiotherapy is a biology-based and clinically feasible approach, particularly in early-stage NSCLC. Further prospective studies are needed to better assess the timing, efficacy and safety of this combination.
References
Dovedi SJ, Lipowska-Bhalla G, Beers SA, et al. Antitumor efficacy of radiation plus immunotherapy depends upon dendritic cell activation of effector CDS+ T cells. Cancer Immunol Res. 2016;4:621–30.
Reits EA, Hodge JW, Herberts CA, et al. Radiation modulates the peptide repertoire, enhances MHC class I expression, and induces successful antitumor immunotherapy. J Exp Med. 2006;203:1259–71.
Kim J, Myers AC, Chen L, et al. Constitutive and inducible expression of b7 family of ligands by human airway epithelial cells. Am J Respir Cell Mol Biol. 2005;33:280–9.
Zhou Q, Munger ME, Veenstra RG, et al. Coexpression of Tim-3 and PD-1 identifies a CD8+ T-cell exhaustion phenotype in mice with disseminated acute myelogenous leukemia. Blood. 2011;117:4501–10.
Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer. 2012;12:252–64.
Kalbasi A, Komar C, Tooker GM, et al. Tumor-derived CCL2 mediates resistance to radiotherapy in pancreatic ductal adenocarcinoma. Clin Cancer Res. 2017;23:137–48.
Seifert L, Werba G, Tiwari S, et al. Radiation therapy induces macrophages to suppress T-cell responses against pancreatic tumors in mice. Gastroenterology. 2016;150(1659-72):E5.
Deng L, Liang H, Burnette B, et al. Irradiation anf anti-PD-L1 treatment synergistically promote antitumor immunity in mice. J Clin Invest. 2017;124:687–95.
Demaria S, Ng B, Devitt ML, et al. Ionizing radiation inhibition of distant untreated tumors (abscopal effect) is immune mediated. Int J Radiat Oncol Biol Phys. 2004;58:862–70.
Marconi R, Strolin S, Bossi G, et al. A meta-analysis of the abscopal effect in preclinical models: is the biologically effective dose a relevant physical trigger? PLoS One. 2017;12:e0171559.
Cameron RB, Spiess PJ, Rosenberg SA. Synergistic antitumor activity of tumor-infiltranting lymphocytes, interleukin 2, and local tumor irradiation. Studies on the mechanism of action. J Exp Med. 1990;171:249–63.
Seetharam S, Staba MJ, Schumm LP, et al. Enhanced eradication of local and distant tumors by genetically produced interleukin-12 and radiation. Int J Oncol. 1999;15:769–73.
Chiang CS, Hong JH, Wu YC, et al. Combining radiation therapy with interleukine-3 gene immunotherapy. Cancer Gene Ther. 2000;7:1172–8.
Chakravarty PK, Alfieri A, Thomas EK, et al. Flt3-ligand administration after radiation therapy prolongs survival in a murine model of metastatic lung cancer. Cancer Res. 1999;59:6028–32.
Demaria S, Bhardwaj N, McBride WH, et al. Combining radiotherapy and immunotherapy: a revived parternship. Int J Radiat Oncol Biol Phys. 2005;63:655–66.
Demaria S, Kawahima N, Yang AM, et al. Immune-mediated inhibition of metastases following treatment with local radiation and CTLA-4 blockade in a mouse model of breast cancer. Clin Cancer Res. 2005;11:728–34.
van den Heuvel MM, Verheiji M, Boshuizen R, et al. NHS-IL2 combined with radiotherapy: preclinical rationale and phase Ib trial results in metastatic non-small cell lung cancer following first-line chemotherapy. J Transl Med. 2015;13:3.
Fiorica F, Belluomini L, Stefanelli A, et al. Immune checkpoint inhibitor Nivolumab and radiotherapy in pretreated lung cancer patients: efficacy and safety of combination. Am J Clin Oncol. 2018;14:18. https://doi.org/10.1097/coc.0000000000000428.
Golden EB, Chachoua A, Fenton-Kerimian MB, et al. Abscopal responses in metastatic non-small cell lung cancer (NSCLC) patients treated on a phase 2 study of combined radiation therapy and Ipilimumab: evidence for the in situ vaccination hypothesis of radiation. Int J Radiat Oncol Biol Phys. 2015;93:S66–7.
Pujol JL, Vansteenkiste JF, De Pas TM, et al. Safety and immunogenicity of MAGE-A3 cancer immunotherapeutic with or without adjuvant chemotherapy in patients with resected stage IB to III MAGE-A3-positive non-small-cell lung cancer. J Thorac Oncol. 2015;10:1458–67.
Butts C, Socinski MA, Mitchell PL, et al. START trial team tecemotide (L-BLP25) versus placebo after chemoradiotherapy for stage III non-small-cell lung cancer (START): a randomised, double-blind, phase 3 trial. Lancet Oncol. 2014;15(1):59–68.
Wurz GT, Gutierrez AM, Greenberg BE, et al. Antitumor effects of L-BLP25 antigen-specific tumor immunotherapy in a novel human MUC1 transgenic lung cancer mouse model. J Transl Med. 2013;11:64.
Giaccone G, Bazhenova LA, Nemunaitis J, et al. A phase III study of belagenpumatucel-L, an allogeneic tumour cell vaccine, as maintenance therapy for non-small cell lung cancer. Eur J Cancer. 2015;51(16):2321–9.
Butts C, Socinski MA, Mitchell PL, et al. START trial team tecemotide (L-BLP25) versus placebo after chemoradiotherapy for stage III non-small-cell lung cancer (START): a randomised, double-blind, phase 3 trial. Lancet Oncol. 2014;15(1):59–68.
Antonia SJ, Villegas A, Daniel D, et al. Durvalumab after chemo-radiotherapy in stage III non-small-cell lung cancer. N Engl J Med. 2017;377(20):1919–29.
Administration FnD (webpage on the Internet). FDA expands approval of imfinzi to reduce the risk of non-small cell lung cancer progressing. 2018. https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm597217.htm. Accessed March 23, 2018.
Antonia SJ, Villegas A, Daniel D, et al. Overall survival with Durvalumab after chemoradiotherapy in stage III NSCLC. N Engl J Med. 2018;379:2342–50.
Lin SH, Lin Y, Price J, et al. DETERRED: PD-L1 blockade to evaluate the safety of lung cancer therapy using carboplatin, paclitaxel, and radiation combined with MPDL3280A (atezolizumab). J Clin Oncol. 2017;35((15 suppl)):3064.
Durm GA, Althouse SK, Sadiq AA. Phase II trial of concurrent chemoradiation with consolidation pembrolizumab in patients with unresectable stage III non-small cell lung cancer: Hoosier cancer research network LUN 14–179. J Clin Oncol. 2018;36(15 suppl):8500.
Acknowledgements
Funding
No funding or sponsorship was received for this work or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
All named authors, Lorenzo Belluomini, Francesco Fiorica and Antonio Frassoldati, have nothing to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced Digital Features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.7553870.
Commentary on “Immune Checkpoint Inhibitor Nivolumab and Radiotherapy in Pretreated Lung Cancer Patients: Efficacy and Safety of Combination [18].”
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Belluomini, L., Fiorica, F. & Frassoldati, A. Immune Checkpoint Inhibitors and Radiotherapy in NSCLC Patients: Not Just a Fluke. Oncol Ther 7, 83–91 (2019). https://doi.org/10.1007/s40487-019-0092-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40487-019-0092-z