Abstract
Background
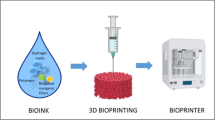
The shortage of available organs for transplantation is the major obstacle hindering the application of regenerative medicine, and has also become the desperate problem faced by more and more patients nowadays. The recent development and application of 3D printing technique in biological research (bioprinting) has revolutionized the tissue engineering methods, and become a promising solution for tissue regeneration.
Results
In this review, we summarize the current application of bioprinting in producing tissues and organoids, and discuss the future directions and challenges of 3D bioprinting.
Conclusions
Currently, 3D bioprinting is capable to generate patient-specialized bone, cartilage, blood vascular network, hepatic unit and other simple components/tissues, yet pure cell-based functional organs are still desired.

Article PDF
Similar content being viewed by others
References
Langer, R. and Vacanti, J. P. (1993) Tissue engineering. Science, 260, 920–926
Atala, A., Bauer, S. B., Soker, S., Yoo, J. J. and Retik, A. B. (2006) Tissue-engineered autologous bladders for patients needing cystoplasty. Lancet, 367, 1241–1246
Lu, T.-Y., Lin, B., Kim, J., Sullivan, M., Tobita, K., Salama, G. and Yang, L. (2013) Repopulation of decellularized mouse heart with human induced pluripotent stem cell-derived cardiovascular progenitor cells. Nat. Commun., 4, 2307
Pati, F., Jang, J., Ha, D. H., Won Kim, S., Rhie, J. W., Shim, J. H., Kim, D. H. and Cho, D. W. (2014) Printing three-dimensional tissue analogues with decellularized extracellular matrix bioink. Nat. Commun., 5, 3935
Murphy, S. V. and Atala, A. (2014) 3D bioprinting of tissues and organs. Nat. Biotechnol., 32, 773–785
Giannopoulos, A. A., Mitsouras, D., Yoo, S. J., Liu, P. P., Chatzizisis, Y. S. and Rybicki, F. J. (2016) Applications of 3D printing in cardiovascular diseases. Nat. Rev. Cardiol., 13, 701–718
Powers, M. K., Lee, B. R. and Silberstein, J. (2016) Threedimensional printing of surgical anatomy. Curr. Opin. Urol., 26, 283–288
Zopf, D. A., Hollister, S. J., Nelson, M. E., Ohye, R. G. and Green, G. E. (2013) Bioresorbable airway splint created with a threedimensional printer. N. Engl. J. Med., 368, 2043–2045
Xiao, Z., Tang, F., Tang, J., Yang, H., Zhao, Y., Chen, B., Han, S., Wang, N., Li, X., Cheng, S., et al. (2016) One-year clinical study of NeuroRegen scaffold implantation following scar resection in complete chronic spinal cord injury patients. Sci. China Life Sci., 59, 647–655
Dababneh, A. B. and Ozbolat, I. T. (2014) Bioprinting technology: a current state-of-the-art review. J. Manuf. Sci. Eng., 136, 061016
Hölzl, K., Lin, S., Tytgat, L., Van Vlierberghe, S., Gu, L. and Ovsianikov, A. (2016) Bioink properties before, during and after 3D bioprinting. Biofabrication, 8, 032002
Jose, R. R., Rodriguez, M. J., Dixon, T. A., Omenetto, F. and Kaplan, D. L. (2016) Evolution of bioinks and additive manufacturing technologies for 3D bioprinting. ACS Biomater. Sci. Eng., 2, 1662–1678
Fricain, J. C., Schlaubitz, S., Le Visage, C., Arnault, I., Derkaoui, S. M., Siadous, R., Catros, S., Lalande, C., Bareille, R., Renard, M., et al. (2013) A nano-hydroxyapatite—pullulan/dextran polysaccharide composite macroporous material for bone tissue engineering. Biomaterials, 34, 2947–2959
Lee, C. H., Rodeo, S. A., Fortier, L. A., Lu, C., Erisken, C. and Mao, J. J. (2014) Protein-releasing polymeric scaffolds induce fibrochondrocytic differentiation of endogenous cells for knee meniscus regeneration in sheep. Sci. Transl. Med., 6, 266ra171
Yan, Y., Wang, X., Pan, Y., Liu, H., Cheng, J., Xiong, Z., Lin, F., Wu, R., Zhang, R. and Lu, Q. (2005) Fabrication of viable tissueengineered constructs with 3D cell-assembly technique. Biomaterials, 26, 5864–5871
Ahn, S. H., Lee, H. J., Lee, J. S., Yoon, H., Chun, W. and Kim, G. H. (2015) A novel cell-printing method and its application to hepatogenic differentiation of human adipose stem cell-embedded mesh structures. Sci. Rep., 5, 13427
Mannoor, M. S., Jiang, Z., James, T., Kong, Y. L., Malatesta, K. A., Soboyejo, W. O., Verma, N., Gracias, D. H. and McAlpine, M. C. (2013) 3D printed bionic ears. Nano Lett., 13, 2634–2639
Ng, W. L., Wang, S., Yeong, W. Y. and Naing, M. W. (2016) Skin bioprinting: impending reality or fantasy? Trends Biotechnol., 34, 689–699
Koch, L., Deiwick, A., Schlie, S., Michael, S., Gruene, M., Coger, V., Zychlinski, D., Schambach, A., Reimers, K., Vogt, P. M., et al. (2012) Skin tissue generation by laser cell printing. Biotechnol. Bioeng., 109, 1855–1863
Michael, S., Sorg, H., Peck, C. T., Koch, L., Deiwick, A., Chichkov, B., Vogt, P. M. and Reimers, K. (2013) Tissue engineered skin substitutes created by laser-assisted bioprinting form skin-like structures in the dorsal skin fold chamber in mice. PLoS One, 8, e57741
Lee, V., Singh, G., Trasatti, J. P., Bjornsson, C., Xu, X., Tran, T. N., Yoo, S. S., Dai, G. and Karande, P. (2014) Design and fabrication of human skin by three-dimensional bioprinting. Tissue Eng. Part C Methods, 20, 473–484
Norotte, C., Marga, F. S., Niklason, L. E. and Forgacs, G. (2009) Scaffold-free vascular tissue engineering using bioprinting. Biomaterials, 30, 5910–5917
Kolesky, D. B., Homan, K. A., Skylar-Scott, M. A. and Lewis, J. A. (2016) Three-dimensional bioprinting of thick vascularized tissues. Proc. Natl. Acad. Sci. USA, 113, 3179–3184
Homan, K. A., Kolesky, D. B., Skylar-Scott, M. A., Herrmann, J., Obuobi, H., Moisan, A. and Lewis, J. A. (2016) Bioprinting of 3D convoluted renal proximal tubules on perfusable chips. Sci. Rep., 6, 34845
Miller, J. S., Stevens, K. R., Yang, M. T., Baker, B. M., Nguyen, D. H., Cohen, D. M., Toro, E., Chen, A. A., Galie, P. A., Yu, X., et al. (2012) Rapid casting of patterned vascular networks for perfusable engineered three-dimensional tissues. Nat. Mater., 11, 768–774
Kolesky, D. B., Truby, R. L., Gladman, A. S., Busbee, T. A., Homan, K. A. and Lewis, J. A. (2014) 3D bioprinting of vascularized, heterogeneous cell-laden tissue constructs. Adv. Mater. Weinheim, 26, 3124–3130
Cui, X., Breitenkamp, K., Finn, M. G., Lotz, M. and D’ Lima, D. D. (2012) Direct human cartilage repair using three-dimensional bioprinting technology. Tissue Eng. Part A, 18, 1304–1312
Cui, X. and Boland, T. (2009) Human microvasculature fabrication using thermal inkjet printing technology. Biomaterials, 30, 6221–6227
Wang, H., Li, Y., Zuo, Y., Li, J., Ma, S. and Cheng, L. (2007) Biocompatibility and osteogenesis of biomimetic nano-hydroxyapatite/ polyamide composite scaffolds for bone tissue engineering. Biomaterials, 28, 3338–3348
Keriquel, V., Guillemot, F., Arnault, I., Guillotin, B., Miraux, S., Amédé e, J., Fricain, J. C. and Catros, S. (2010) In vivo bioprinting for computer- and robotic-assisted medical intervention: preliminary study in mice. Biofabrication, 2, 014101
Xu, T., Binder, K. W., Albanna, M. Z., Dice, D., Zhao, W., Yoo, J. J. and Atala, A. (2013) Hybrid printing of mechanically and biologically improved constructs for cartilage tissue engineering applications. Biofabrication, 5, 015001
Reichert, J. C., Cipitria, A., Epari, D. R., Saifzadeh, S., Krishnakanth, P., Berner, A., Woodruff, M. A., Schell, H., Mehta, M., Schuetz, M. A., et al. (2012) A tissue engineering solution for segmental defect regeneration in load-bearing long bones. Sci. Transl. Med., 4, 141ra93
Sadtler, K., Singh, A., Wolf, M. T., Wang, X., Pardoll, D. M. and Elisseeff, J. H. (2016) Design, clinical translation and immunological response of biomaterials in regenerative medicine. Nat. Rev. Mater., 1, 16040
Chia, H. N. and Wu, B. M. (2015) Recent advances in 3D printing of biomaterials. J. Biol. Eng., 9, 4
Caliari, S. R. and Burdick, J. A. (2016) A practical guide to hydrogels for cell culture. Nat. Methods, 13, 405–414
Pereira, R. F. and Bártolo, P. J. (2015) 3D bioprinting of photocrosslinkable hydrogel constructs. J. Appl. Polym. Sci., 132, 42458
Lei, M. and Wang, X. (2016) Biodegradable polymers and stem cells for bioprinting. Molecules, 21, 539
Zhu, W., Ma, X., Gou, M., Mei, D., Zhang, K. and Chen, S. (2016) 3D printing of functional biomaterials for tissue engineering. Curr. Opin. Biotechnol., 40, 103–112
Ma, X., Qu, X., Zhu, W., Li, Y.-S., Yuan, S., Zhang, H., Liu, J., Wang, P., Lai, C. S. E., Zanella, F., et al. (2016) Deterministically patterned biomimetic human iPSC-derived hepatic model via rapid 3D bioprinting. Proc. Natl. Acad. Sci. USA, 113, 2206–2211
Kang, H. W., Lee, S. J., Ko, I. K., Kengla, C., Yoo, J. J. and Atala, A. (2016) A 3D bioprinting system to produce human-scale tissue constructs with structural integrity. Nat. Biotechnol., 34, 312–319
Hoch, E., Tovar, G. E. M. and Borchers, K. (2014) Bioprinting of artificial blood vessels: current approaches towards a demanding goal. Eur. J. Cardiothorac. Surg., 46, 767–778
Irvine, S. A. and Venkatraman, S. S. (2016) Bioprinting and Differentiation of Stem Cells. Molecules, 21, 1188
Saunders, R. E. and Derby, B. (2014) Inkjet printing biomaterials for tissue engineering: bioprinting. Int. Mater. Rev., 59, 430–448
Zhao, Y., Li, Y., Mao, S., Sun, W. and Yao, R. (2015) The influence of printing parameters on cell survival rate and printability in microextrusion-based 3D cell printing technology. Biofabrication, 7, 045002
Devillard, R., Pagès, E., Correa, M. M., Kériquel, V., Rémy, M., Kalisky, J., Ali, M., Guillotin, B. and Guillemot, F. (2014). Chapter 9 — Cell Patterning by Laser-Assisted Bioprinting. In Methods in Cell Biology, Matthieu, P. and Manuel, T., eds. 159–174. New York: Academic Press
Wang, X., Ao, Q., Tian, X., Fan, J., Wei, Y., Hou, W., Tong, H. and Bai, S. (2016) 3D bioprinting technologies for hard tissue and organ engineering. Materials (Basel), 9, 802
Yi, H., Ur Rehman, F., Zhao, C., Liu, B. and He, N. (2016) Recent advances in nano scaffolds for bone repair. Bone Res., 4, 16050
Skardal, A., Mack, D., Kapetanovic, E., Atala, A., Jackson, J. D., Yoo, J. and Soker, S. (2012) Bioprinted amniotic fluid-derived stem cells accelerate healing of large skin wounds. Stem Cells Transl. Med., 1, 792–802
Kim, J. J., Hou, L. and Huang, N. F. (2016) Vascularization of three-dimensional engineered tissues for regenerative medicine applications. Acta Biomater., 41, 17–26
Mandrycky, C., Wang, Z., Kim, K. and Kim, D.-H. (2016) 3D bioprinting for engineering complex tissues. Biotechnol. Adv., 34, 422–434
Li, S., Xiong, Z., Wang, X., Yan, Y., Liu, H. and Zhang, R. (2009) Direct fabrication of a hybrid cell/hydrogel construct by a doublenozzle assembling technology. J. Bioact. Compat. Polym., 24, 249–265
Acknowledgements
This work is supported by grants 31271349 from the National Natural Science Foundation of China, China 973 Program 2014CB964901 and CAS Strategic Priority Research Program grant XDA01020105.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, Z., Wang, XJ. Current progresses of 3D bioprinting based tissue engineering. Quant Biol 5, 136–142 (2017). https://doi.org/10.1007/s40484-017-0103-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40484-017-0103-8