Abstract
Purpose of the Review
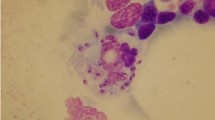
In this review, we summarized information regarding two neglected parasitic infestations by arthropods belonging to order Diptera and the order Siphonaptera, causing myiasis and tungiasis, respectively.
Recent Findings
Although there has been an increase in the number of publications on myiasis and tungiasis, over the last decades, these are still neglected conditions among the tropical disease, with not more 200 papers per year combined, in databases such as PubMed. Besides that, these are problems that disproportionally affect the more vulnerable populations in the world.
Summary
Both myiasis and tungiasis are ectoparasitic pathologies affecting mainly the skin, but, specially the first, also mucous membranes and organs of humans and animals.



Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Nanda S, Carr P, Noland M. Image Gallery: A case of botfly myiasis due to Dermatobia hominis in the U.S.A. with no history of international travel. Br J Dermatol. 2020;182(6): e184.
Francesconia F, Lupi O. Myiasis. Clin Microbiol Rev. 2012;25(1):79–105.
Bernhardt V, Finkelmeier F, Verhoff MA, Amendt J. Myiasis in humans—a global case report evaluation and literature analysis. Parasitol Res. 2019;118(2):389–97.
Calvopina M, Ortiz-Prado E, Castañedaid B, Cueva I, Rodriguez-Hidalgo R, Cooperid PJ. Human myiasis in Ecuador. PLoS Negl Trop Dis. 2020;14(2):1–13.
Norgan AP, Pritt BS. Parasitic infections of the skin and subcutaneous tissues. Adv Anat Pathol. 2018;25(2):106–23.
Kollipara R, Peranteau AJ, Nawas ZY, Tong Y, Woc-Colburn L, Yan AC, et al. Emerging infectious diseases with cutaneous manifestations fungal, helminthic, protozoan and ectoparasitic infections. J Am Acad Dermatol. 2016;75(1):19–30. Available from:. https://doi.org/10.1016/j.jaad.2016.04.032.
Lachish T, Marhoom E, Mumcuoglu KY, Tandlich M, Schwartz E. Myiasis in travelers. J Travel Med. 2015;22(4):232–6.
Korzeniewski K, Juszczak D, Jerzemowski J. Skin lesions in returning travellers. Int Marit Health. 2015;66(3):173–80.
Di Tullio F, Mandel VD, Miglietta R, Pellacani G. Cutaneous myiasis in a traveler returning from Argentina. Dermatol Ther. 2019;32(5):1–4.
Hall MJR, Wall RL, Stevens JR. Traumatic myiasis: a neglected disease in a changing world. Annu Rev Entomol. 2016;61(1):159–76.
McGarry JW. Tropical myiases: neglected and well travelled. Lancet Infect Dis. 2014;14(8):672–4. Available from:. https://doi.org/10.1016/S1473-3099(14)70830-8.
Sweileh WM. Global output of research on epidermal parasitic skin diseases from 1967 to 2017. Infect Dis Poverty. 2018;7(1):1–10.
Robbins K, Khachemoune A. Cutaneous myiasis: a review of the common types of myiasis. Int J Dermatol. 2010;49(10):1092–8.
Otranto D. The immunology of myiasis: parasite survival and host defense strategies. Trends Parasitol. 2001;17(4):176–82.
Moiré N, Bigot Y, Periquet G, Boulard C. Sequencing and gene expression of hypodermins A, B, C in larval stages of Hypoderma lineatum. Mol Biochem Parasitol. 1994 Aug;66(2):233–40.
Farkas R, Hornok S, Gyurkovszky M. Preliminary studies on humoral immune response of sheep to wohlfahrtiosis. Vet Parasitol. 1998;75(2–3):279–84.
Oliveira-Sequeira TCG, Sequeira JL, Schmitt FL, De Lello E. Histological and immunological reaction of cattle skin to first-instar larvae of Dermatobia hominis. Med Vet Entomol. 1996;10(4):323–30.
Solomon M, Lachish T, Schwartz E. Cutaneous Myiasis [Internet]. Current Infectious Disease Reports. Current Medicine Group LLC 2016;18(1):1–7. Available from: https://link.springer.com/article/10.1007/s11908-016-0537-6.
Giacobbe DR, Riccardi N, Vena A, Bassetti M. Mould Infections of Traumatic Wounds: A Brief Narrative Review. Infect Dis Ther. 2020;9(1):1–15.
Singh A, Kaur J. Occurrence of human urogenital myiasis due to neglected personal hygiene: a review. Trans R Soc Trop Med Hyg. 2019;113(1):4–10.
Diociaiuti A, Oranges T, Giancristoforo S, Dini V, El Hachem M. A novel dermoscopic pattern observed in furuncular myiasis. Australas J Dermatol. 2019;60(1):e46–7.
• Cunha PR, Flora TB, Kroumpouzos G. Travelers’ tropical skin diseases: challenges and interventions. Dermatol Ther. 2019;32(4):1–9 Article reviews the main tropical diseases of travelers, with an emphasis on diagnosis, management, and prevention.
Shukla D, Kamath AT, Kudva A, Pai D, Patel N. Our Experience in the Management of Traumatic Wound Myiasis: Report of 3 Cases and Review of the Literature. Case Reports in Dentistry. 2016;2016(7030925):4. https://doi.org/10.1155/2016/7030925.
Uysal S, Ozturk AM, Tasbakan M, Simsir IY, Unver A, Turgay N, et al. Human myiasis in patients with diabetic foot: 18 cases. Ann Saudi Med. 2018;38(3):208–13.
Jain A. Myiasis in patients with oral squamous cell carcinoma-a systematic review and protocol for management. Oral Maxillofac Surg. 2019;23(3):265–269. https://doi.org/10.1007/s10006-019-00757-2.
Shi C, Xu R, Tang X, Hui Z. Sulfur ointment treatment of cutaneousmyiasis caused by the tumbu fly. JAMA Dermatol. 2018;154(6):737–8.
Patel BC, Ostwal S, Sanghavi PR, Joshi G, Singh R. Management of malignant wound myiasis with ivermectin, albendazole, and clindamycin (triple therapy) in advanced head-and-neck cancer patients: a prospective observational study. Indian J Palliat Care. 2018;24(4):459–64.
Biradar S, Wankhede P, Munde A, Shaikh S. Extensive myiasis infestation associated with oral squamous cell carcinoma: report of two cases. Dent Res J (Isfahan). 2015;12(1):100.
Zia MK, Asad SI, Wase HA, Salam O, Hassan SZ, Musab M, et al. Case report: myiasis as a rare complication of invasive ductal carcinoma [version 1; peer review: 1 approved with reservations]. F1000Research. 2019;8:774.
•• Ashour DS. Ivermectin: from theory to clinical application. Int J Antimicrob Agents. 2019;54(2):134–42. Available from: https://doi.org/10.1016/j.ijantimicag.2019.05.003Article reviews the highlights the most common human uses of ivermectin and new and promising properties.
Osorio J, Moncada L, Molano A, Valderrama S, Gualtero S, Franco-Paredes C. Role of ivermectin in the treatment of severe orbital myiasis due to Cochliomyia hominivorax. Clin Infect Dis. 2006;43(6):e57–9.
Arria M, Rodríguez Morales AJ, Medina M, Blanco JJ. Tungiasis en el estado Táchira: ¿Una Ectoparasitosis Reemergente? Academia. 2004;3(6):02–3.
Arria M, Rodriguez-Morales AJ, Franco-Paredes C. Ecoepidemiología de las Enfermedades Tropicales en Países de la Cuenca Amazónica. Rev Peru Med Exp Salud Publica. 2005;22(3):236–40.
•• Cardoso AEC, Cardoso AEO, Talhari C, Santos M. Update on parasitic dermatoses. An Bras Dermatol. 2020;95(1):1–14 Article reviews the main clinical and therapeutic aspects of scabies, pediculosis, myiasis, tungiasis, larva migrans, Lyme disease, and onchocerciasis.
Coates SJ, Thomas C, Chosidow O, Engelman D, Chang AY. Ectoparasites: pediculosis and tungiasis. J Am Acad Dermatol. 2020;82(3):551–69.
Feldmeier H, Heukelbach J, Ugbomoiko US, Sentongo E, Mbabazi P, von Samson-Himmelstjerna G, et al. Tungiasis--a neglected disease with many challenges for global public health. PLoS Negl Trop Dis. 2014;8(10):e3133.
Miller H, Ocampo J, Ayala A, Trujillo J, Feldmeier H. Very severe tungiasis in Amerindians in the Amazon lowland of Colombia: a case series. PLoS Negl Trop Dis. 2019;13(2):e0007068.
Sánchez-Carmona D, Montoya C, Cardona-Ospina JA, Ramirez V, Quintero L, Bedoya-Arias JE, et al. Estimating the neglected incidence of tungiasis in Colombia, 2009-2013. Biomédica. 2015;35(Supl.4):173.
CDC. DPDx. Tungiasis. Available at: https://www.cdc.gov/dpdx/613tungiasis/index.html. Accessed 27 June 2020.
Maco V, Maco VP, Tantalean ME, Gotuzzo E. Histopathological features of tungiasis in Peru. Am J Trop Med Hyg. 2013;88(6):1212–6.
Mumcuoglu K. Other ectoparasites: leeches, myiasis and sand fleas. In: Farrar J, Junghanss T, Lalloo D, Hotez P, Kang G, White NJ (Eds) Manson’s tropical infectious diseases. 23rd ed: Elsevier; 2014;843–47.
Diaz JH. Myiasis and tungiasis. In: Bennett JE, Dolin R, Blaser MJ, editors. Mandell, Douglas, and Bennett's Principles and practice of infectious diseases. 8th ed: Elsevier; 2015;3255–59.
Wardhaugh AD, Norris JF. A case of imported tungiasis in Scotland initially mimicking verrucae vulgaris. Scott Med J. 1994;39(5):146–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Skin and Soft Tissue Infections in Returning Travelers from the Tropics
Rights and permissions
About this article
Cite this article
Osorio-Pinzon, J., Palencia, A., Cruz-Calderon, S. et al. Myiasis and Tungiasis. Curr Trop Med Rep 8, 112–120 (2021). https://doi.org/10.1007/s40475-021-00233-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40475-021-00233-6