Abstract
Purpose of the Review
To provide an overview of the concept of comorbidity, research that supports the common co-occurrence of neurodevelopmental disorders and directions for future research.
Recent Findings
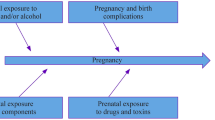
Neurodevelopmental disorders including attention-deficit/hyperactivity disorder, developmental coordination disorder, autism spectrum disorder, and learning disorders co-occur more commonly than would be expected by chance. The potential causes for this comorbidity suggested in the research literature are genetic, epigenetic, neurobiological, and environmental.
Summary
Directions for research such as imaging genetics and epidemiological studies examining prenatal environmental exposures could increase our understanding of the mechanism underlying the high rates of symptom comorbidity among neurodevelopmental disorders. This in turn could lead to improvements in diagnosis, a better understanding of the course of these disorders, and the development of more effective treatments.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 5th edition (5th ed.). Arlington: American Psychiatric Publishing; 2013.
Reiss AL. Childhood developmental disorders: an academic and clinical convergence point for psychiatry, neurology, psychology and pediatrics. J Child Psychol Psychiatry. 2009;50(1–2):87–98.
Johnson MR, Shorvon SD. Heredity in epilepsy: neurodevelopment, comorbidity, and the neurological trait. Epilepsy Behav. 2011;22(3):421–7.
Rapoport JL, Giedd JN, Gogtay N. Neurodevelopmental model of schizophrenia: update 2012. Mol Psychiatry. 2012;17(12):1228–38.
Bloom B, Cohen RA, Freeman G. Summary health statistics for U.S. children: National Health Interview Survey, 2010. Vital Health Stat 10. 2011;250:1–80.
Atladottir HO, Gyllenberg D, Langridge A, Sandin S, Hansen SN, Leonard H, et al. The increasing prevalence of reported diagnoses of childhood psychiatric disorders: a descriptive multinational comparison. Eur Child Adolesc Psychiatry. 2014;24(2):173–83.
Grandjean P, Landrigan PJ. Neurobehavioural effects of developmental toxicity. Lancet Neurol. 2014;13(7):330–8.
Gillberg C, Rasmussen P. Perceptual, motor and attentional deficits in seven-year-old children: background factors. Dev Med Child Neurol. 1982;24:752–70.
Anderson JC, Williams S, McGee R, Silva PA. DSM-III disorders in preadolescent children: prevalence in a large sample from the general population. Arch Gen Psychiatry. 1987;44(1):69–76.
Gillberg C. Perceptual, motor and attentional deficits in Swedish primary school children. Some child psychiatric aspects. J Child Psychol Psychiatry. 1983;24(3):377–403.
Feinstein AR. The pre-therapeutic classification of comorbidity in chronic disease. J Chronic Dis. 1970;23(7):455–68.
Angold A, Costello EJ, Erkanli A. Comorbidity. J Child Psychol Psychiatry. 1999;40(1):57–87.
Clements DS. Minimal brain dysfunction in children. NINDB Monograph No 3. 1966. 76–349.
Capute AJ, Palmer FB. A pediatric overview of the spectrum of developmental disabilities. J Dev Behav Pediatr. 1980;1(2):66–9.
Capute PJ, Capute AJ, Accardo PJ. A neurodevelopmental perspective on the continuum of developmental disabilities. In: Capute AJ, Accardo PJ, editors. Developmental disabilities in infancy and childhood: neurodevelopmental diagnosis and treatment (3 Ed, Vol 1). Baltimore: Paul H Brooks Publishing Co; 2007. p. 3–23.
Gilger JW, Kaplan BJ. Atypical brain development: a conceptual framework for understanding developmental learning disabilities. Dev Neuropsychol. 2001;20(2):465–8.
Gillberg C. The ESSENCE in child psychiatry: early symptomatic syndromes eliciting neurodevelopmental clinical examinations. Res Dev Disabil. 2010;31(6):1543–51.
Moreno-De-Luca A, Myers SM, Challman TD, Moreno-De-Luca D, Evans DW, Ledbetter DH. Developmental brain dysfunction: revival and expansion of old concepts based on new genetic evidence. Lancet Neurol. 2013;12(4):406–14.
Cantell MH, Smyth MM, Ahonen TP. Two distinct pathways for developmental coordination disorder: persistence and resolution. Hum Mov Sci. 2003;22:413–31.
Harpin VA. The effect of ADHD on the life of an individual, their family, and community from preschool to adult life. Arch Dis Child. 2005;90(Suppl1):i2–7.
Gotham K, Pickles A, Lord C. Trajectories of autism severity in children using standardized ADOS scores. Pediatrics. 2012;130(5):e1278–84.
• Barnevik Olsson M, Lundström S, Westerlund J, Giacobini MB, Gillberg C, Fernell E. Preschool to school in autism: neuropsychiatric problems 8 years after diagnosis at 3 years of age. J Autism Dev Disord. 2016;46(8):2749–55 This paper found that at 11 years of age, 90% children diagnosed with ASD prior to 4.5 years met criteria for at least one neurodevelopmental disorder: ASD, ADHD, DCD or learning disorder.
Jensen M, Girirajan S. Mapping a shared genetic basis for neurodevelopmental disorders. Genome Med. 2017;9(1):109.
Lichtenstein P, Carlström E, Råstam M, Gillberg C, Anckarsäter H. The genetics of autism spectrum disorders and related neuropsychiatric disorders in childhood. Am J Psychiatry. 2010;167(11):1357–63.
•• Jokiranta-Olkoniemi E, Cheslack-Postava K, Sucksdorff D, Suominen A, Gyllenberg D, Chudal R, et al. Risk of psychiatric and neurodevelopmental disorders among siblings of probands with autism spectrum disorders. JAMA Psychiatry. 2016;73(6):622–9 This epidemiological study included children with ASD born in Finland from 1987-2005 and diagnosed with ASD by December 2007. Siblings were born between 1977 and 2005 and were diagnosed between 1987 and 2009. The relative risk of having a sibling diagnosed with any psychiatric or neurodevelopmental disorder as 2.5 times greater for among chlldren diagnosed with ASD compared to controls. The largest associations were for child-onset disorders including ASD, tic disorders, ADHD, learning and coordination disorders, intellectual disability, conduct and oppositional disorders and emotional disorders. These findings support the contention that several psychiatric and neurodevelopmental disorders have common risk factors.
•• Jokiranta-Olkoniemi E, Cheslack-Postava K, Joelsson P, Suominen A, Brown AS, Sourander A. Attention-deficit/hyperactivity disorder and risk for psychiatric and neurodevelopmental disorders in siblings. Psychol Med. 2018. This large epidemiological study included every children born in Finland from 1991-2005 and diagnosed with ADHD between 2005-2011. Results revealed that siblings of children with ADHD were at higher risk of child onset disorders including ADHD, ASD, DCD, learning disorders, intellectual disability, conduct and oppositional disorders and emotional and social interaction disorders. These findings provide support for the idea that neurodevelopmental disorders may have common etiologies.
World Health Organization. ICD 11: International Classification of Diseases 11th Revision [Internet]. 2018 [cited 2018 Jun 20]. Available from: https://icd.who.int
Cruddace SA, Riddell PM. Attention processes in children with movement difficulties, reading difficulties or both. J Abnorm Child Psychol. 2006;34(5):675–83.
Yeargin-Allsopp M, Boyle C, Braun KVN, Trevathan E. The epidemiology of developmental disabilities. In: Capute AJ, Accardo PJ, editors. Developmental disabilities in infancy and childhood: neurodevelopmental diagnosis and treatment (3 Ed, Vol 1). 2007. p. 61–104.
Visser J. Developmental coordination disorder: a review of research on subtypes and comorbidities. Hum Mov Sci. 2003;22(4–5):479–93.
Kadesjö B, Gillberg C. The comorbidity of ADHD in the general population of Swedish school-age children. J Child Psychol Psychiatry. 2001;42(4):487–92.
Piek JP, Pitcher TM, Hay D. a. Motor coordination and kinaesthesis in boys with attention deficit-hyperactivity disorder. Dev Med Child Neurol. 1999;41(3):159–65.
Querne L, Berquin P, Vernier-Hauvette MP, Fall S, Deltour L, Meyer ME, et al. Dysfunction of the attentional brain network in children with developmental coordination disorder: a fMRI study. Brain Res. 2008;1244:89–102.
Lahey BB, Van Hulle CA, Singh AL, Waldman ID, Rathouz PJ. Higher-order genetic and environmental structure of prevalent forms of child and adolescent psychopathology. Arch Gen Psychiatry 2011;68(2):181–189.
Kaplan BJ, Wilson BN, Dewey D, Crawford SG. DCD may not be a discrete disorder. Hum Mov Sci. 1998;17(4–5):471–90.
Pieters S, de Block K, Scheiris J, Eyssen M, Desoete A, Deboutte D, et al. How common are motor problems in children with a developmental disorder: rule or exception? Child Care Health Dev. 2012;38(1):139–45.
Dewey D, Kaplan BJ, Crawford SG, Wilson BN. Developmental coordination disorder: associated problems in attention, learning, and psychosocial adjustment. Hum Mov Sci. 2002;21(5–6):905–18.
Hill EL, Bishop DVM, Nimmo-Smith I. A dyspraxic deficit in specific language impairment and developmental coordination disorder? Evidence from hand and arm movements. Dev Med Child Neurol. 1998;17(6):388–95.
Pitcher TM, Piek JP, Hay DA. Fine and gross motor ability in males with ADHD. Dev Med Child Neurol. 2007;45(8):525–35.
Taurines R, Schmitt J, Renner T, Conner AC, Warnke A, Romanos M. Developmental comorbidity in attention-deficit/hyperactivity disorder. Atten Defic Hyperact Disord. 2012;4(3):115–39.
Taurines R, Schwenck C, Westerwald E, Sachse M, Siniatchkin M, Freitag C. ADHD and autism: differential diagnosis or overlapping traits? A selective review. Atten Defic Hyperact Disord. 2012;4(3):115–39.
Willcutt EG, Pennington BF, Duncan L, Smith SD, Keenan JM, Wadsworth S, et al. Understanding the complex etiologies of developmental disorders: behavioral and molecular genetic approaches. J Dev Behav Pediatr. 2010;31(7):533–44.
Davis NO, Kollins SH. Treatment for co-occurring attention deficit/hyperactivity disorder and autism spectrum disorder. Neurotherapeutics. 2012;9(3):518–30.
Dewey D, Cantell M, Crawford SG. Motor and gestural performance in children with autism spectrum disorders, developmental coordination disorder, and/or attention deficit hyperactivity disorder. J Int Neuropsychol Soc. 2007;13(2):246–56.
Green D, Charman T, Pickles A, Chandler S, Loucas T, Simonoff E, et al. Impairment in movement skills of children with autistic spectrum disorders. Dev Med Child Neurol. 2009;51(4):311–6.
Kaplan B, Crawford S, Cantell M, Kooistra L, Dewey D. Comorbidity, co-occurrence, continuum: what’s in a name? Child Care Health Dev. 2006;32(6):723–31.
Zhang Y, Haraksingh R, Grubert F, Abyzov A, Gerstein M, Weissman S, et al. Child development and structural variation in the human genome. Child Dev. 2013;84(1):34–48.
van Mil NH, Steegers-Theunissen RPM, Bouwland-Both MI, Verbiest MMPJ, Rijlaarsdam J, Hofman A, et al. DNA methylation profiles at birth and child ADHD symptoms. J Psychiatr Res. 2014;49(1):51–9.
•• Walton E, Pingault JB, CAM C, Gaunt TR, Relton CL, Mill J, et al. Epigenetic profiling of ADHD symptoms trajectories: a prospective, methylome-wide study. Mol Psychiatry. 2017;22(2):250–6 Results revealed that DNA methylation at birth differentiated ADHD trajectories across multiple genomic locations, including probes annotated to SKI (involved in neural tube development), ZNF544 (previously implicated in ADHD), ST3GAL3 (linked to intellectual disability) and PEX2 (related to perixosomal processes). None of these probes maintained an association with ADHD trajectories at age 7. These findings highlight the potential importance of DNA methylation variation in genes related to neurodevelopment.
Richter M, Murtaza N, Scharrenberg R, White SH, Johanns O, Walker S, et al. Altered TAOK2 activity causes autism-related neurodevelopmental and cognitive abnormalities through RhoA signaling. Mol Psychiatry. 2018.
Elia J, Gai X, Xie HM, Perin JC, Geiger E, Glessner JT, et al. Rare structural variants found in attention-deficit hyperactivity disorder are preferentially associated with neurodevelopmental genes. Mol Psychiatry. 2010;15(6):637–46.
• Mosca SJ, Langevin LM, Dewey D, Micheil Innes A, Lionel AC, Marshall CC, et al. Copy-number variations are enriched for neurodevelopmental genes in children with developmental coordination disorder. J Med Genet. 2016;53(12):812–9 This is the first paper to show that genes play an important role in developmental coordination disorder.
Lionel AC, Crosbie J, Barbosa N, Goodale T, Thiruvahindrapuram B, Rickaby J, et al. Rare copy number variation discovery and cross-disorder comparisons identify risk genes for ADHD. Sci Transl Med. 2011;3(95):95ra75.
Glessner JT, Connolly JJM, Hakonarson H. Rare genomic deletions and duplications and their role in neurodevelopmental disorders. Curr Top Behav Neurosci. 2012;12:345–60.
Kaminsky EB, Kaul V, Paschall J, Church DM, Bunke B, Kunig D, et al. An evidence-based approach to establish the functional and clinical significance of copy number variants in intellectual and developmental disabilities. Genet Med. 2011;13(9):777–84.
Girirajan S, Brkanac Z, Coe BP, Baker C, Vives L, Vu TH, et al. Relative burden of large CNVs on a range of neurodevelopmental phenotypes. PLoS Genet. 2011;7(11):e1002334.
Chen ES, Gigek CO, Rosenfeld JA, Diallo AB, Maussion G, Chen GG, et al. Molecular convergence of neurodevelopmental disorders. Am J Hum Genet. 2014;95(5):490–508.
Cristino AS, Williams SM, Hawi Z, An J-Y, Bellgrove MA, Schwartz CE, et al. Neurodevelopmental and neuropsychiatric disorders represent an interconnected molecular system. Mol Psychiatry. 2014;19(3):294–301.
Viding E, Williamson D, Hariri A. Developmental imaging genetics: challenges and promises for translational research. Dev Psychopathol. 2006;18(3):877–92.
Langevin LM, Macmaster FP, Crawford S, Lebel C, Dewey D. Common white matter microstructure alterations in pediatric motor and attention disorders. J Pediatr. 2014;164(5):1157–64.
Langevin LM, Macmaster FP, Dewey D. Distinct patterns of cortical thinning in concurrent motor and attention disorders. Dev Med Child Neurol. 2015 Aug;57(3):257–64.
McLeod KR, Langevin LM, Goodyear BG, Dewey D. Functional connectivity of neural motor networks is disrupted in children with developmental coordination disorder and attention-deficit/hyperactivity disorder. Neuroimage Clin. 2014;4:566–75.
McLeod KR, Langevin LM, Dewey D, Goodyear BG. Atypical within- and between-hemisphere motor network functional connections in children with developmental coordination disorder and attention-deficit/hyperactivity disorder. Neuroimage Clin. 2016;12:157–64.
Dehue T, Bijl D, de Winter M, Scheepers F, Vanheule S, van Os J, et al. Subcortical brain volume differences in participants with attention deficit hyperactivity disorder in children and adults. Lancet Psychiatry. 2017;4(6):438–9.
Zeng K, Kang J, Ouyang G, Li J, Han J, Wang Y, et al. Disrupted brain network in children with autism spectrum disorder. Sci Rep. 2017;7(1):16253.
Thornton S, Bray S, Langevin LM, Dewey D. Functional brain correlates of motor response inhibition in children with developmental coordination disorder and attention deficit/hypractivity disorder. Hum Mov Sci. 2018;59:134–42.
Vandenberg LN, Hauser R, Marcus M, Olea N, Welshons WV. Human exposure to bisphenol A (BPA). Reprod Toxicol. 2007;24(2):139–77.
Health Canada. Third report on human biomonitoring of environmental chemicals in Canada: results of the canadian health measures survey cycle 3 (2012-2013). [Internet]. 2015 [cited 2016 Aug 28]. Available from: http://www.hc-sc.gc.ca/ewh-semt/pubs/contaminants/chms-ecms-cycle3/index-eng.php
World Health Organization. Human biomonitoring: facts and figures. Copenhagen; 2015.
Shapiro GD, Dodds L, Arbuckle TE, Ashley-Martin J, Fraser W, Fisher M, et al. Exposure to phthalates, bisphenol A and metals in pregnancy and the association with impaired glucose tolerance and gestational diabetes mellitus: the MIREC study. Environ Int. 2015;83:63–71.
Ejaredar M, Nyanza EC, Ten Eycke K, Dewey D. Phthalate exposure and childrens neurodevelopment: a systematic review. Environ Res 2015;142:51–60.
Ejaredar M, Lee Y, Roberts DJ, Sauve R, Dewey D. Bisphenol A exposure and children’s behavior: a systematic review. J Expo Sci Environ Epidemiol. 2017;27(2):175–83.
Barouki R, Gluckman PD, Grandjean P, Hanson M, Heindel JJ. Developmental origins of non-communicable disease: implications for research and public health. Environ Health. 2012;11:42.
Porrini S, Belloni V, Della SD, Farabollini F, Giannelli G, Dessi-Fulgheri F. Early exposure to a low dose of bisphenol A affects socio-sexual behavior of juvenile female rats. Brain Res Bull. 2005;65(3):261–6.
Fujimoto T, Kubo K, Aou S. Prenatal exposure to bisphenol a impairs sexual differentiation of exploratory behavior and increases depression-like behavior in rats. Brain Res. 2006;1068(1):49–55.
Matsuda S, Matsuzawa D, Ishii D, Tomizawa H, Sutoh C, Nakazawa K, et al. Effects of perinatal exposure to low dose of bisphenol A on anxiety like behavior and dopamine metabolites in brain. Prog Neuro-Psychopharmacol Biol Psychiatry. 2012;39(2):273–9.
Bale TL, Baram TZ, Brown AS, Goldstein JM, Insel TR, McCarthy MM, et al. Early life programming and neurodevelopmental disorders. Biol Psychiatry. 2010;68:314–9.
Darney S, Fowler B, Grandjean P, Heindel J, Mattison D, Slikker W Jr. Prenatal programming and toxicity II (PPTOX II): role of environmental stressors in the developmental origins disease. Reprod Toxicol. 2011;31(3):271.
Hodyl NA, Roberts CT, Bianco-Miotto T. Cord blood DNA methylation biomarkers for predicting neurodevelopmental outcomes. Genes (Basel). 2016;7(12)
Kinch CD, Ibhazehiebo K, Jeong J-H, Habibi HR, Kurrasch DM. Low-dose exposure to bisphenol A and replacement bisphenol S induces precocious hypothalamic neurogenesis in embryonic zebrafish. Proc Natl Acad Sci U S A. 2015;112(5):1475–80.
Xu X-H, Wang Y-M, Zhang J, Luo Q-Q, Ye Y-P, Ruan Q. Perinatal exposure to bisphenol-A changes N-methyl-D-aspartate receptor expression in the hippocampus of male rat offspring. Environ Toxicol Chem. 2010;29(1):176–81.
Poimenova A, Markaki E, Rahiotis C, Kitraki E. Corticosterone-regulated actions in the rat brain are affected by perinatal exposure to low dose of bisphenol A. Neuroscience. 2010;167(3):742–9.
Dewey D, Reardon A, Grohs MN, Liu J, Ten Eycke KD, Ejaredar M, et al. Effects of prenatal exposure to environmental neurotoxicants on health and neurodevelopment. 2018 ISES-ISEE joint annual meeting. 2018.
Trasande L, Zoeller RT, Hass U, Kortenkamp A, Grandjean P, Myers JP, et al. Burden of disease and costs of exposure to endocrine disrupting chemicals in the European Union: an updated analysis. Andrology. 2016;4(4):565–72.
Jensen PS, Hinshaw SP, Kraemer HC, Lenora N, Newcorn JH, Abikoff HB, et al. ADHD comorbidity findings from the MTA study: comparing comorbid subgroups. J Am Acad Child Adolesc Psychiatry. 2001;40(2):147–58.
Crawford SG, Dewey D. Co-occurring disorders: a possible key to visual perceptual deficits in children with developmental coordination disorder? Hum Mov Sci. 2008;27(1):154–69.
Crawford SG, Kaplan BJ, Dewey D. Effects of coexisting disorders on cognition and behavior in children with ADHD. J Atten Disord. 2006;10(2):192–9.
Casey BJ, Soliman F, Bath KG, Glatt CE. Imaging genetics and development: challenges and promises. Hum Brain Mapp. 2010;31:838–51.
Durston S. Imaging genetics in ADHD. NeuroImage. 2010;53(3):832–8.
Pine DS, Ernst M, Leibenluft E. Imaging-genetics applications in child psychiatry. J Am Acad Child Adolesc Psychiatry. 2010;49(8):772–82.
Flint J, Timpson N, Munaf M. Assessing the utility of intermediate phenotypes for genetic mapping of psychiatric disease. Trends Neurosci. 2014;37(12):733–41.
Rasetti R, Weinberger DR. Intermediate phenotypes in psychiatric disorders. Curr Opin Genet Dev. 2011;21(3):340–8.
Gottesman II, Gould TD. The endophenotype concept in psychiatry: etymology and strategic intentions. Am J Psychiatry. 2003;160(4):636–45.
Liu J, Calhoun VD. A review of multivariate analyses in imaging genetics. Front Neuroinform. 2014;8:29.
Sui J, He H, Yu Q, Chen J, Rogers J, Pearlson GD, et al. Combination of resting state fMRI, DTI, and sMRI data to discriminate schizophrenia by N-way MCCA + jICA. Front Hum Neurosci. 2013;7:235.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The author declares that there are no competing interests.
Human and Animal Rights and Informed Consent
These studies were approved by the Conjoint Health Research Ethics Board of the University of Calgary and informed consent was obtained from study participants.
Additional information
This article is part of the Topical Collection on Comorbidities
Rights and permissions
About this article
Cite this article
Dewey, D. What Is Comorbidity and Why Does It Matter in Neurodevelopmental Disorders?. Curr Dev Disord Rep 5, 235–242 (2018). https://doi.org/10.1007/s40474-018-0152-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40474-018-0152-3