Abstract
Purpose of Review
Diabetes mellitus is a top contributor to the global burden of mortality and disability in adults. There has also been a slow but steady rise in prediabetes and type 2 diabetes in youth. The current review summarizes recent findings regarding the impact of increased exposure to air pollutants on the type 2 diabetes epidemic.
Recent Findings
Human and animal studies provide strong evidence that exposures to ambient and traffic-related air pollutants such as particulate matter (PM), nitrogen dioxide (NO2), and nitrogen oxides (NOx) play an important role in metabolic dysfunction and type 2 diabetes etiology. This work is supported by recent findings that have observed similar effect sizes for increased exposure to air pollutants on clinical measures of risk for type 2 diabetes in children and adults. Further, studies indicate that these effects may be more pronounced among individuals with existing risk factors, including obesity and prediabetes.
Summary
Current epidemiological evidence suggests that increased air pollution exposure contributes to alterations in insulin signaling, glucose metabolism, and beta (β)-cell function. Future work is needed to identify the specific detrimental pollutants that alter glucose metabolism. Additionally, advanced tools and new areas of investigation present unique opportunities to study the underlying mechanisms, including intermediate pathways, that link increased air pollution exposure with type 2 diabetes onset.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1545–602.
Dabelea D, Mayer-Davis EJ, Saydah S, Imperatore G, Linder B, Divers J, et al. Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. JAMA. 2014;311:1778–86.
Imperatore G, Boyle JP, Thompson TJ, Case D, Dabelea D, Hamman RF, et al. Projections of type 1 and type 2 diabetes burden in the U.S. population aged <20 years through 2050: dynamic modeling of incidence, mortality, and population growth. Am Diabetes Assoc Diabetes Care. 2012;35:2515–20.
Ljungman PL, Mittleman MA. Ambient air pollution and stroke. Stroke. 2014;45:3734–41.
Koulova A, Frishman WH. Air pollution exposure as a risk factor for cardiovascular disease morbidity and mortality. Cardiol Rev. 2014;22:30–6.
Sava F, Carlsten C. Respiratory health effects of ambient air pollution: an update. Clin Chest Med. 2012;33:759–69.
Eze IC, Foraster M, Schaffner E, Vienneau D, Héritier H, Rudzik F, et al. Long-term exposure to transportation noise and air pollution in relation to incident diabetes in the SAPALDIA study. Int J Epidemiol. 2017;46:1115–25.
Honda T, Pun VC, Manjourides J, Suh H. Associations between long-term exposure to air pollution, glycosylated hemoglobin and diabetes. Int J Hyg Environ Health. 2017;220:1124–32.
Jerrett M, Brook R, White LF, Burnett RT, Yu J, Su J, et al. Ambient ozone and incident diabetes: a prospective analysis in a large cohort of African American women. Environ Int. 2017;102:42–7.
Mazidi M, Speakman JR. Ambient particulate air pollution (PM2.5) is associated with the ratio of type 2 diabetes to obesity. Sci Rep. 2017;7(1):9144.
O'Donovan G, Chudasama Y, Grocock S, Leigh R, Dalton AM, Gray LJ, et al. The association between air pollution and type 2 diabetes in a large cross-sectional study in Leicester: The CHAMPIONS study. Environ Int. 2017;104:41–7.
Requia WJ, Adams MD, Koutrakis P. Association of PM2.5 with diabetes, asthma, and high blood pressure incidence in Canada: a spatiotemporal analysis of the impacts of the energy generation and fuel sales. Sci Total Environ. 2017;584-585:1077–83.
Sohn D, Gender-dependent Differences OH. In the relationship between diabetes mellitus and ambient air pollution among adults in South Korean cities. Iran J Public Health. 2017;46:293–300.
Strak M, Janssen N, Beelen R, Schmitz O, Vaartjes I, Karssenberg D, et al. Long-term exposure to particulate matter, NO2 and the oxidative potential of particulates and diabetes prevalence in a large national health survey. Environ Int. 2017;108:228–36.
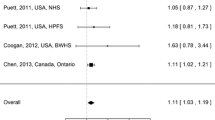
Coogan PF, White LF, Yu J, Burnett RT, Marshall JD, Seto E, et al. Long term exposure to NO2 and diabetes incidence in the Black Women’s Health Study. Environ Res. 2016;148:360–6.
Dzhambov A, Dimitrova D. Exposures to road traffic, noise, and air pollution as risk factors for type 2 diabetes: a feasibility study in Bulgaria. Noise Health. 2016;18:133–11.
•• Hansen AB, Ravnskjær L, Loft S, Andersen KK, Bräuner EV, Baastrup R, et al. Long-term exposure to fine particulate matter and incidence of diabetes in the Danish Nurse Cohort. Environ Int. 2016;91:243–50. Large prospective cohort study among 28,731 female nurses in Denmark. Results indicate that long-term exposures to PM 2.5 were associated with greater diabetes incidence from year 1993–2013. No significant associations were observed for NO 2 , PM 10 , and NO x exposures. The associations with PM 2.5 were larger in nonsmokers and obese participants.
Lazarevic N, Dobson AJ, Barnett AG, Knibbs LD. Long-term ambient air pollution exposure and self-reported morbidity in the Australian Longitudinal Study on Women’s Health: a cross-sectional study. BMJ Open. 2015;5(10):e008714.
• Liu C, Yang C, Zhao Y, Ma Z, Bi J, Liu Y, et al. Associations between long-term exposure to ambient particulate air pollution and type 2 diabetes prevalence, blood glucose and glycosylated hemoglobin levels in China. Environ Int. 2016;92–93:416–21. Large, cross-sectional study ( n =11,847) conducted in China with relatively high pollution levels. Results suggest that long-term exposures to ambient PM 2.5 were associated with higher risk of type 2 diabetes. These findings suggest that air pollution exposures impact type 2 diabetes risk in high polluted areas. Notably, similar findings were also observed in Europe and North America, where air pollution levels are relatively low.
•• Park SK, Adar SD, O’Neill MS, Auchincloss AH, Szpiro A, Bertoni AG, et al. Long-term exposure to air pollution and type 2 diabetes mellitus in a multiethnic cohort. Am J Epidemiol. 2015;181:327–36. A large multiethnic, prospective study ( n =5,839) across six sites in the USA, which found long-term exposures to NO 2 and PM 2.5 were associated with a higher prevalence of type 2 diabetes across all sites. However, the longitudinal associations between long-term exposures to NO 2 and PM 2.5 and type 2 diabetes incidence were largely nonsignificant in across study sites .
To T, Zhu J, Villeneuve PJ, Simatovic J, Feldman L, Gao C, et al. Chronic disease prevalence in women and air pollution—a 30-year longitudinal cohort study. Environ Int. 2015;80:26–32.
Weinmayr G, Hennig F, Fuks K, Nonnemacher M, Jakobs H, Möhlenkamp S, et al. Long-term exposure to fine particulate matter and incidence of type 2 diabetes mellitus in a cohort study: effects of total and traffic-specific air pollution. Environ Health. 2015;14:53.
Chien L-C, Alamgir H, Yu H-L. Spatial vulnerability of fine particulate matter relative to the prevalence of diabetes in the United States. Sci Total Environ. 2015;508:136–44.
Eze IC, Schaffner E, Fischer E, Schikowski T, Adam M, Imboden M, et al. Long-term air pollution exposure and diabetes in a population-based Swiss cohort. Environ Int. 2014;70:95–105.
Chen H, Burnett RT, Kwong JC, Villeneuve PJ, Goldberg MS, Brook RD, et al. Risk of incident diabetes in relation to long-term exposure to fine particulate matter in Ontario, Canada. Environ Health Perspect. 2013;121:804–10.
Andersen ZJ, Raaschou-Nielsen O, Ketzel M, Jensen SS, Hvidberg M, Loft S, et al. Diabetes incidence and long-term exposure to air pollution: a cohort study. Am Diabetes Assoc Diabetes Care. 2012;35:92–8.
Coogan PF, White LF, Jerrett M, Brook RD, Su JG, Seto E, et al. Air pollution and incidence of hypertension and diabetes mellitus in black women living in Los Angeles. Circulation. 2012;125:767–72.
•• Chen Z, Salam MT, Toledo-Corral C, Watanabe RM, Xiang AH, Buchanan TA, et al. Ambient air pollutants have adverse effects on insulin and glucose homeostasis in Mexican Americans. Diabetes Care. 2016a;39:547–54. First adult study to examine ambient air pollution exposure with robust measures of insulin sensitivity estimated from a FSIVGTT. Results indicate that short-term and long-term exposures to PM 2.5 were associated with lower insulin sensitivity as well as higher fasting glucose and dyslipidemia.
Wallwork RS, Colicino E, Zhong J, Kloog I, Coull BA, Vokonas P, et al. Ambient fine particulate matter, outdoor temperature, and risk of metabolic syndrome. Am J Epidemiol. 2017;185:30–9.
Brook RD, Sun Z, Brook JR, Zhao X, Ruan Y, Yan J, et al. Extreme air pollution conditions adversely affect blood pressure and insulin resistance: the Air Pollution and Cardiometabolic Disease Study. Hypertension. 2016;67:77–85.
• Chen L, Zhou Y, Li S, Williams G, Kan H, Marks GB, et al. Air pollution and fasting blood glucose: a longitudinal study in China. Sci Total Environ. 2016b;541:750–5. A large longitudinal study that shows that NO 2 , PM 10 , and SO 2 were associated with fasting glucose, a clinical marker of glucose metabolism dysfunction.
Jiang S, Bo L, Gong C, Du X, Kan H, Xie Y, et al. Traffic-related air pollution is associated with cardio-metabolic biomarkers in general residents. Int Arch Occup Environ Health. 2016;89:911–21.
Peng C, Bind M-AC, Colicino E, Kloog I, Byun H-M, Cantone L, et al. Particulate air pollution and fasting blood glucose in nondiabetic individuals: associations and epigenetic mediation in the normative aging study, 2000–2011. Environ Health Perspect. 2016;124:1715–21.
• Sade MY, Kloog I, Liberty IF, Katra I, Novack L, Novack V. Air pollution and serum glucose levels: a population-based study. Medicine (Baltimore). 2015;94:e1093. A large ( n =27,685) longitudinal study in China that indicates that acute exposures (prior 0–3 day average) to NO 2 , PM 10 , and SO 2 were associated higher fasting glucose, a clinical marker of glucose metabolism dysfunction.
• Wolf K, Popp A, Schneider A, Breitner S, Hampel R, Rathmann W, et al. Association between long-term exposure to air pollution and biomarkers related to insulin resistance, subclinical inflammation, and adipokines. Diabetes. 2016;65:3314–26. Large cross-sectional study ( n =2,944) in German adults where air pollution levels are relatively low. Results show that higher long-term exposures to a wide spectrum of ambient and traffic-related air pollutants (e.g., NO 2 , NOx, PM 2.5 , and PM 10 ) were associated with higher fasting glucose, HOMA-IR, and leptin. Notably, the associations were strongest among prediabetic participants.
Eze IC, Schaffner E, Foraster M, Imboden M, von Eckardstein A, Gerbase MW, Rothe T, Rochat T, Künzli N, Schindler C, Probst-Hensch N. Long-Term Exposure to Ambient Air Pollution and Metabolic Syndrome in Adults. PLoS One. 2015;10(6):e0130337.
Brook RD, Xu X, Bard RL, Dvonch JT, Morishita M, Kaciroti N, et al. Reduced metabolic insulin sensitivity following sub-acute exposures to low levels of ambient fine particulate matter air pollution. Sci Total Environ. 2013;448:66–71.
Teichert T, Vossoughi M, Vierkötter A, Sugiri D, Schikowski T, Schulte T, et al. Association between traffic-related air pollution, subclinical inflammation and impaired glucose metabolism: results from the SALIA Study. PLoS ONE. 2013;8:e83042.
Yitshak Sade M, Kloog I, Liberty IF, Schwartz J, Novack V. The association between air pollution exposure and glucose and lipids levels. J Clin Endocrinol Metab. 2016;101:2460–7.
Bergman RN. Lilly lecture 1989. Toward physiological understanding of glucose tolerance. Minimal-model approach. Diabetes. 1989;38:1512–27.
Mayer-Davis EJ, Lawrence JM, Dabelea D, Divers J, Isom S, Dolan L, et al. Incidence trends of type 1 and type 2 diabetes among youths, 2002–2012. N Engl J Med. 2017;376:1419–29.
Eppens MC, Craig ME, Cusumano J, Hing S, Chan AKF, Howard NJ, et al. Prevalence of diabetes complications in adolescents with type 2 compared with type 1 diabetes. Diabetes Care. 2006;29(6):1300–6.
•• Alderete TL, Habre R, Toledo-Corral CM, Berhane K, Chen Z, Lurmann FW, et al. Longitudinal associations between ambient air pollution with insulin sensitivity, β-cell function, and adiposity in Los Angeles Latino children. Diabetes. 2017a;66:1789–96. First longitudinal study to examine ambient air pollutants (NO 2 and PM 2.5 ) with robust measures of insulin sensitivity and β-cell function estimated by FSIVGTT. Results indicate that long-term exposures to NO 2 and PM 2.5 were associated with faster declines in insulin sensitivity and β-cell function among overweight and obese children.
• Ghosh R, Gauderman WJ, Minor H, Youn HA, Lurmann F, Cromar KR, et al. Air pollution, weight loss and metabolic benefits of bariatric surgery: a potential model for study of metabolic effects of environmental exposures. Pediatr Obes. 2017. https://doi.org/10.1111/ijpo.12210. [Epub ahead of print]. The only current intervention study in children showing an attenuation of the metabolic benefits associated with bariatric surgery with increased air pollution exposure.
Thiering E, Markevych I, Brüske I, Fuertes E, Kratzsch J, Sugiri D, et al. Associations of residential long-term air pollution exposures and satellite-derived greenness with insulin resistance in German adolescents. Environ Health Perspect. 2016;124:1291–8.
• Toledo-Corral CM, Alderete TL, Habre R, Berhane K, Lurmann FW, Weigensberg MJ, et al. Effects of air pollution exposure on glucose metabolism in Los Angeles minority children. Pediatr Obes. 2016;312:1218. First cross-sectional study in children examining the associations of chronic exposures to ambient and traffic-related air pollutants with type 2 diabetes-related quantitative traits including robust measures of insulin sensitivity estimated from a FSIVGTT.
Calderón-Garcidueñas L, Franco-Lira M, D'Angiulli A, Rodríguez-Díaz J, Blaurock-Busch E, Busch Y, et al. Mexico City normal weight children exposed to high concentrations of ambient PM2.5 show high blood leptin and endothelin-1, vitamin D deficiency, and food reward hormone dysregulation versus low pollution controls. Relevance for obesity and Alzheimer disease. Environ Res. 2015;140:579–92.
Thiering E, Cyrys J, Kratzsch J, Meisinger C, Hoffmann B, Berdel D, et al. Long-term exposure to traffic-related air pollution and insulin resistance in children: results from the GINIplus and LISAplus birth cohorts. Diabetologia. 2013;56:1696–704.
Nemmar A. Passage of inhaled particles into the blood circulation in humans. Circulation. 2002;105:411–4.
Tamagawa E, Bai N, Morimoto K, Gray C, Mui T, Yatera K, et al. Particulate matter exposure induces persistent lung inflammation and endothelial dysfunction. Am J Physiol Lung Cell Mol Phys. 2008;295:L79–85.
Happo MS, Salonen RO, Hälinen AI, Jalava PI, Pennanen AS, Kosma VM, et al. Dose and time dependency of inflammatory responses in the mouse lung to urban air coarse, fine, and ultrafine particles from six European cities. Inhal Toxicol. 2007;19:227–46.
van Eeden SF, Tan WC, Suwa T, Mukae H, Terashima T, Fujii T, et al. Cytokines involved in the systemic inflammatory response induced by exposure to particulate matter air pollutants (PM(10)). Am J Respir Crit Care Med. 2001;164:826–30.
Dadvand P, Nieuwenhuijsen MJ, Agustí À, de Batlle J, Benet M, Beelen R, et al. Air pollution and biomarkers of systemic inflammation and tissue repair in COPD patients. Eur Respir J. 2014;44:603–13.
Fry RC, Rager JE, Zhou H, Zou B, Brickey JW, Ting J, et al. Individuals with increased inflammatory response to ozone demonstrate muted signaling of immune cell trafficking pathways. Respir Res. 2012;13:89.
González-Guevara E, Martínez-Lazcano JC, Custodio V, Hernández-Cerón M, Rubio C, Paz C. Exposure to ozone induces a systemic inflammatory response: possible source of the neurological alterations induced by this gas. Inhal Toxicol. 2014;26:485–91.
Rajagopalan S, Brook RD. Air pollution and type 2 diabetes: mechanistic insights. Diabetes. 2012;61:3037–45.
Xu X, Liu C, Xu Z, Tzan K, Zhong M, Wang A, et al. Long-term exposure to ambient fine particulate pollution induces insulin resistance and mitochondrial alteration in adipose tissue. Toxicol Sci. 2011;124:88–98.
Xu X, Yavar Z, Verdin M, Ying Z, Mihai G, Kampfrath T, et al. Effect of early particulate air pollution exposure on obesity in mice: role of p47phox. Arterioscler Thromb Vasc Biol. 2010;30:2518–27.
Irigaray P, Ogier V, Jacquenet S, Notet V, Sibille P, Mejean L, et al. Benzo[a]pyrene impairs beta-adrenergic stimulation of adipose tissue lipolysis and causes weight gain in mice. A novel molecular mechanism of toxicity for a common food pollutant. FEBS J. 2006;273:1362–72.
Sun Q, Yue P, Deiuliis JA, Lumeng CN, Kampfrath T, Mikolaj MB, et al. Ambient air pollution exaggerates adipose inflammation and insulin resistance in a mouse model of diet-induced obesity. Circulation. 2009;119:538–46.
Sas KM, Karnovsky A, Michailidis G, Pennathur S. Metabolomics and diabetes: analytical and computational approaches. Diabetes. 2015;64:718–32.
Breitner S, Schneider A, Devlin RB, Ward-Caviness CK, Diaz-Sanchez D, Neas LM, et al. Associations among plasma metabolite levels and short-term exposure to PM2.5 and ozone in a cardiac catheterization cohort. Environ Int. 2016;97:76–84.
Sourij H, Meinitzer A, Pilz S, Grammer TB, Winkelmann BR, Boehm BO, et al. Arginine bioavailability ratios are associated with cardiovascular mortality in patients referred to coronary angiography. Atherosclerosis. 2011;218:220–5.
Schooneman MG, Vaz FM, Houten SM, Soeters MR. Acylcarnitines: reflecting or inflicting insulin resistance? Diabetes. 2013;62:1–8.
Menni C, Metrustry SJ, Mohney RP, Beevers S, Barratt B, Spector TD, et al. Circulating levels of antioxidant vitamins correlate with better lung function and reduced exposure to ambient pollution. Am J Respir Crit Care Med. 2015;191:1203–7.
Wang-Sattler R, Yu Z, Herder C, Messias AC, Floegel A, He Y, et al. Novel biomarkers for pre-diabetes identified by metabolomics. Mol Syst Biol. 2012;8:615.
Ferrannini E, Natali A, Camastra S, Nannipieri M, Mari A, Adam K-P, et al. Early metabolic markers of the development of dysglycemia and type 2 diabetes and their physiological significance. Diabetes. 2013;62:1730–7.
Floegel A, Stefan N, Yu Z, Mühlenbruch K, Drogan D, Joost H-G, et al. Identification of serum metabolites associated with risk of type 2 diabetes using a targeted metabolomic approach. Diabetes. 2013;62:639–48.
Zhao Y-Y, Wang H-L, Cheng X-L, Wei F, Bai X, Lin R-C, et al. Metabolomics analysis reveals the association between lipid abnormalities and oxidative stress, inflammation, fibrosis, and Nrf2 dysfunction in aristolochic acid-induced nephropathy. Sci Rep. 2015;5:12936.
Miller DB, Karoly ED, Jones JC, Ward WO, Vallanat BD, Andrews DL, et al. Inhaled ozone (O3)-induces changes in serum metabolomic and liver transcriptomic profiles in rats. Toxicol Appl Pharmacol. 2015;286:65–79.
Miller DB, Ghio AJ, Karoly ED, Bell LN, Snow SJ, Madden MC, et al. Ozone exposure increases circulating stress hormones and lipid metabolites in humans. Am J Respir Crit Care Med. 2016;193:1382–91.
Kodavanti UP. Air pollution and insulin resistance: do all roads lead to Rome? Diabetes. 2015;64:712–4.
Vella RE, Pillon NJ, Zarrouki B, Croze ML, Koppe L, Guichardant M, et al. Ozone exposure triggers insulin resistance through muscle c-Jun N-terminal kinase activation. Diabetes. 2015;64:1011–24.
Wei Y, Zhang J, Li Z, Gow A, Chung KF, Hu M, et al. Chronic exposure to air pollution particles increases the risk of obesity and metabolic syndrome: findings from a natural experiment in Beijing. FASEB J. 2016;30:2115–22.
Bolton JL, Smith SH, Huff NC, Gilmour MI, Foster WM, Auten RL, et al. Prenatal air pollution exposure induces neuroinflammation and predisposes offspring to weight gain in adulthood in a sex-specific manner. FASEB J. 2012;26:4743–54.
Elmquist JK, Scherer PE. The cover. Neuroendocrine and endocrine pathways of obesity. JAMA. 2012;308:1070–1.
Kodavanti UP. Stretching the stress boundary: linking air pollution health effects to a neurohormonal stress response. Biochim Biophys Acta. 2016;1860:2880–90.
Gackière F, Saliba L, Baude A, Bosler O, Strube C. Ozone inhalation activates stress-responsive regions of the CNS. J Neurochem. 2011;117:961–72.
Beamish LA, Osornio-Vargas AR, Wine E. Air pollution: an environmental factor contributing to intestinal disease. J Crohns Colitis. 2011;5:279–86.
Möller W, Häussinger K, Winkler-Heil R, Stahlhofen W, Meyer T, Hofmann W, et al. Mucociliary and long-term particle clearance in the airways of healthy nonsmoker subjects. J Appl Physiol. 2004;97(6):2200–6.
Nemmar A, Hoet PM, Vanquickenborne B, Dinsdale D, Thomeer M, Hoylaerts MF, et al. Passage of inhaled particles into the blood circulation in humans. Circulation. 2002;105:411–4.
Salim SY, Kaplan GG, Madsen KL. Air pollution effects on the gut microbiota: a link between exposure and inflammatory disease. Gut Microbes. 2014;5:215–9.
Dybdahl M. DNA adduct formation and oxidative stress in colon and liver of Big Blue(R) rats after dietary exposure to diesel particles. Carcinogenesis. 2003;24:1759–66.
Kish L, Hotte N, Kaplan GG, Vincent R, Tso R, Gänzle M, et al. Environmental particulate matter induces murine intestinal inflammatory responses and alters the gut microbiome. PLoS ONE. 2013a;8:e62220.
Mutlu EA, Engen PA, Soberanes S, Urich D, Forsyth CB, Nigdelioglu R, et al. Particulate matter air pollution causes oxidant-mediated increase in gut permeability in mice. Part Fibre Toxicol. 2011;8:19.
Kish L, Hotte N, Kaplan GG, Vincent R, Tso R, Gänzle M, et al. Environmental particulate matter induces murine intestinal inflammatory responses and alters the gut microbiome. PLoS One. 2013b;8:e62220.
Shen J, Obin MS, Zhao L. The gut microbiota, obesity and insulin resistance. Mol Asp Med. 2013;34:39–58.
Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. 2006;444:1027–31.
Amar J, Lange C, Payros G, Garret C, Chabo C, Lantieri O, et al. Blood microbiota dysbiosis is associated with the onset of cardiovascular events in a large general population: the D.E.S.I.R. study. PLoS One. 2013;8:e54461.
Kaplan GG, Hubbard J, Korzenik J, Sands BE, Panaccione R, Ghosh S, et al. The inflammatory bowel diseases and ambient air pollution: a novel association. Am J Gastroenterol. 2010;105:2412–9.
Kaplan GG, Szyszkowicz M, Fichna J, Rowe BH, Porada E, Vincent R, et al. Non-specific abdominal pain and air pollution: a novel association. PLoS One. 2012;7:e47669.
Alderete TL, Jones RB, Chen Z, Kim JS, Habre R, Lurmann F, et al. Exposure to traffic-related air pollution and the composition of the gut microbiota in overweight and obese adolescents. Environ Res. 2017b;161:472–8.
Lerner A, Neidhöfer S, Matthias T. The gut microbiome feelings of the brain: a perspective for non-microbiologists. Microorganisms. 2017;12;5(4). https://doi.org/10.3390/microorganisms.
Funding
Southern California Environmental Health Sciences Center grant (5P30ES007048) funded by the National Institute of Environmental Health Sciences
National Institute of Environmental Health Sciences (5P01ES011627)
Southern California Children's Environmental Health Center grant funded by National Institute of Environmental Health Sciences (5P01ES022845-03) and United States Environmental Protection Agency (RD83544101)
National Institute of Environmental Health Sciences (K99ES027853)
National Institute of Environmental Health Sciences (K99ES027870)
National Institute of Environmental Health Sciences (T32ES013678)
National Institute of Environmental Health Sciences, National Institute on Minority Health and Health Disparities (P50ES026086)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Tanya L. Alderete, Zhanghua Chen, Claudia Toledo-Corral, Zuelma A. Contreras, and Jennifer S. Kim report grants from NIH outside the submitted work.
Rima Habre, Leda Chatzi, and Frank D. Gilliland declare no conflicts of interest.
Theresa Bastain reports grants from NIH, during the conduct of the study.
Carrie V. Breton reports grants from NIH, outside the submitted work.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Environmental Epidemiology
Rights and permissions
About this article
Cite this article
Alderete, T.L., Chen, Z., Toledo-Corral, C.M. et al. Ambient and Traffic-Related Air Pollution Exposures as Novel Risk Factors for Metabolic Dysfunction and Type 2 Diabetes. Curr Epidemiol Rep 5, 79–91 (2018). https://doi.org/10.1007/s40471-018-0140-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40471-018-0140-5