Abstract
Purpose of Review
Novel integrative reviews that give detail information regarding various psychoactive substances (PS) with ability of inducing psychosis in adults are lacking. This review aims to scope the latest knowledge about substance-induced psychosis (SIP) through the comprehensive review of the most common misused PS inducing psychosis.
Recent Findings
Epidemiological data on the prevalence of SIP are insufficiently harmonized, so clear conclusions for most PS can not be drawn. Etiological mechanisms include three pathophysiological mechanisms: the modulation of GABA transmission, NMDA antagonism, and effects on the monoaminergic system. Beside positive symptoms, PS may induce negative and cognitive symptoms. There are no uniform therapeutic guidelines for specific SIP, but some antipsychotics appear to be more effective than others. It is likely that the conversion rate of SIP to schizophrenia may be higher in the future because novel PS with a higher psychotic potential are increasingly being consumed.
Summary
This review presents epidemiological data, etiological mechanisms, details of clinical pictures, and treatment options for psychoses induced by specific PS.
Similar content being viewed by others
Data Availability
Data sharing is not applicable to this paper as no new data were created in this paper.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Fiorentini A, Cantù F, Crisanti C, Cereda G, Oldani L, Brambilla P. Substance-induced psychoses: an updated literature review. Front Psychiatry. 2021;12:694863. Very important because it is updated literature review.
Garson E, Castle DJ, George TP. Substance-induced psychosis: a narrative review. Curr Addict Rep. 2023;10:335–40. Provides a detailed overview of the latest insights on how to differentiate substance-induced psychosis and schizophrenia.
Thirthalli J, Benegal V. Psychosis among substance users. Curr Opin Psychiatry. 2006;19(3):239–45.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5™. 5th ed. Washington, DC: American Psychiatric Publishing, Inc.; 2013.
World Health Organization. International statistical classification of diseases and related health problems,11th ed. Genève; 2019. https://icd.who.int/. Accessed 15 Jan 2023.
Mauri MC, Di Pace C, Reggiori A, Paletta S, Colasanti A. Primary psychosis with comorbid drug abuse and drug-induced psychosis: diagnostic and clinical evolution at follow up. Asian J Psychiatr. 2017;29:117–22.
Starzer MSK, Nordentoft M, Hjorthøj C. Rates and predictors of conversion to schizophrenia or bipolar disorder following substance-induced psychosis. Am J Psychiatry. 2017;175:343–50. A register-based study with a large number of subjects investigated the convert rates of substance-induced psychosis to schizophrenia.
European Monitoring Centre for Drugs and Drug Addiction. European Drug Report: Trends and Developments 2022. https://www.emcdda.europa.eu/publications-database_en?f[0]=:404&f[1]=publication_type:404. Accessed 1 May 2023.
Hjorthøj C, Madsen T, Starzer M, Erlangsen A, Nordentoft M. Mortality in substance-induced psychosis: a register-based national cohort study. Addiction. 2021;116(12):3515–24. A register-based study showing that substance-induced psychosis is associated with an increased mortality risk, even among cases who did not convert to schizophrenia.
Barbic D, Whyte M, Sidhu G, Luongo A, Stenstrom R, Chakraborty TA, et al. What is the risk of returning to the emergency department within 30 days for patients diagnosed with substance-induced psychosis? CJEM. 2022;24(7):702–9.
Ham S, Kim TK, Chung S, Im HI. Drug abuse and psychosis: new insights into drug-induced psychosis. Exp Neurobiol. 2017;26(1):11–24.
Paparelli A, Di Forti M, Morrison PD, Murray RM. Drug-induced psychosis: how to avoid star gazing in schizophrenia research by looking at more obvious sources of light. Front Behav Neurosci. 2011;5:1. https://doi.org/10.3389/fnbeh.2011.00001.
Maremmani AG, Rovai L, Rugani F, Bacciardi S, Dell'Osso L, Maremmani I. Substance abuse and psychosis. The strange case of opioids. Eur Rev Med Pharmacol Sci. 2014;18(3):287–302.
Connor JP, Stjepanović D, Le Foll B, Hoch E, Budney AJ, Hall WD. Cannabis use and cannabis use disorder. Nat Rev Dis Primers. 2021;7(1):16.
Chong WW, Acar ZI, West ML, Wong F. A scoping review on the medical and recreational use of cannabis during the COVID-19 pandemic. Cannabis Cannabinoid Res. 2022;7(5):591–602.
Hjorthøj C, Larsen MO, Starzer MSK, Nordentoft M. Annual incidence of cannabis-induced psychosis, other substance-induced psychoses and dually diagnosed schizophrenia and cannabis use disorder in Denmark from 1994 to 2016. Psychol Med. 2021;51(4):617–22. A register-based study demonstrating an increase in the incidence of cannabis-induced psychosis over a ten-year period.
Wilkinson ST, Radhakrishnan R, D'Souza DC. Impact of cannabis use on the development of psychotic disorders. Curr Addict Rep. 2014;1(2):115–28.
Chesney E, Oliver D, McGuire P. Cannabidiol (CBD) as a novel treatment in the early phases of psychosis. Psychopharmacology. 2022;239(5):1179–90.
Sorkhou M, Bedder RH, George TP. The behavioral sequelae of cannabis use in healthy people: a systematic review. Front Psychiatry. 2021;12:630247. https://doi.org/10.3389/fpsyt.2021.630247.
Pearson NT, Berry JH. Cannabis and psychosis through the Lens of DSM-5. Int J Environ Res Public Health. 2019;16(21):4149. https://doi.org/10.3390/ijerph16214149.
Wainberg M, Jacobs GR, di Forti M, Tripathy SJ. Cannabis, schizophrenia genetic risk, and psychotic experiences: a cross-sectional study of 109,308 participants from the UK biobank. Transl Psychiatry. 2021;11(1):211.
Di Forti M, Quattrone D, Freeman TP, Tripoli G, Gayer-Anderson C, Quigley H, et al.; EU-GEI WP2 group. The contribution of cannabis use to variation in the incidence of psychotic disorder across Europe (EU-GEI): a multicentre case-control study. Lancet Psychiatry. 2019;6(5):427–36. A multinational study revealed that daily cannabis use increases the odds of psychotic disorder. The odds are higher with highly potent cannabis, according to the study.
Woolridge SM, Wood-Ross C, Voleti R, Harrison GW, Berisha V, Bowie CR. A neuropsychological approach to differentiating cannabis-induced and primary psychotic disorders. Early Interv Psychiatry. 2023;17(6):564–72.
Kendler KS, Ohlsson H, Sundquist J, Sundquist K. Prediction of onset of substance-induced psychotic disorder and its progression to schizophrenia in a Swedish National Sample. Am J Psychiatry. 2019;176:711–9.
Little R, D'Mello D. A cannabinoid hypothesis of schizophrenia: pathways to psychosis. Innov Clin Neurosci. 2022;19(7–9):38–43.
Caspi A, Moffitt TE, Cannon M, McClay J, Murray R, Harrington H, et al. Moderation of the effect of adolescent-onset cannabis use on adult psychosis by a functional polymorphism in the catechol-O-methyltransferase gene: longitudinal evidence of a gene X environment interaction. Biol Psychiatry. 2005;57:1117–27.
Hasan A, von Keller R, Friemel CM, Hall W, Schneider M, Koethe D, et al. Cannabis use and psychosis: a review of reviews. Eur Arch Psychiatry Clin Neurosci. 2020;270(4):403–12.
Cohen K, Weinstein AM. Synthetic and non-synthetic cannabinoid drugs and their adverse effects-a review from public health prospective. Front Public Health. 2018;6:162.
Fattore L. Synthetic cannabinoids-further evidence supporting the relationship between cannabinoids and psychosis. Biol Psychiatry. 2016;79(7):539–48.
Krabseth HM, Tuv SS, Strand MC, Karinen RA, Wiik E, Vevelstad MS, et al. Novel psychoactive substances. Tidsskr Nor Laegeforen. 2016;3(136):714–7.
Roberto AJ, Lorenzo A, Li KJ, Young J, Mohan A, Pinnaka S, et al. First-episode of synthetic cannabinoid-induced psychosis in a young adult, successfully managed with hospitalization and risperidone. Case Rep Psychiatry. 2016;2016:7257489. https://doi.org/10.1155/2016/7257489.
Murray RM, Quigley H, Quattrone D, Englund A, Di Forti M. Traditional marijuana, high-potency cannabis and synthetic cannabinoids: increasing risk for psychosis. World Psychiatry. 2016;15(3):195–204.
Shah D, Chand P, Bandawar M, Benegal V, Murthy P. Cannabis induced psychosis and subsequent psychiatric disorders. Asian J Psychiatr. 2017;30:180–4.
Compton MT, Manseau M, editors. The complex connection between cannabis and schizophrenia. Academic Press; 2017. https://www.sciencedirect.com/book/9780128047910/the-complex-connection-between-cannabis-and-schizophrenia. Accessed 1 Sep 2023.
Rentero D, Arias F, Sánchez-Romero S, Rubio G, Rodríguez-Jiménez R. Cannabis-induced psychosis: clinical characteristics and its differentiation from schizophrenia with and without cannabis use. Adicciones. 2021;33(2):95–108. English, Spanish
Mills B, Yepes A, Nugent K. Synthetic cannabinoids. Am J Med Sci. 2015;350(1):59–62.
Tait RJ, Caldicott D, Mountain D, Hill SL, Lenton S. A systematic review of adverse events arising from the use of synthetic cannabinoids and their associated treatment. Clin Toxicol (Phila). 2016;54(1):1–13.
Lappin JM, Sara GE. Psychostimulant use and the brain. Addiction. 2019;114(11):2065–77. An extensive and detailed review that comprehensively depicts all aspects of the negative impact of psychostimulant use on the nervous system.
Bramness JG, Rognli EB. Psychosis induced by amphetamines. Curr Opin Psychiatry. 2016;29(4):236–41.
Lecomte T, Dumais A, Dugré JR, Potvin S. The prevalence of substance-induced psychotic disorder in methamphetamine misusers: a meta-analysis. Psychiatry Res. 2018;268:189–92. A meta-analysis revealed that 36.5% of those who misuse methamphetamines develop a psychotic disorder.
Huang CL, Tsai IJ, Lee CW. Risk of psychosis in illicit amphetamine users: a 10 year retrospective cohort study. Evidence-based Mental Health. 2022;25(4):163–8.
Shalaby AS, Bahanan AO, Alshehri MH, Elag KA. Sleep deprivation & amphetamine induced psychosis. Psychopharmacol Bull. 2022;52(3):31–40.
Roncero C, Daigre C, Grau-López L, Barral C, Pérez-Pazos J, et al. An international perspective and review of cocaine-induced psychosis: a call to action. Subst Abus. 2014;35(3):321–7.
Roncero C, Daigre C, Grau-López L, Rodríguez-Cintas L, Barral C, Pérez-Pazos J, et al. Cocaine-induced psychosis and impulsivity in cocaine-dependent patients. J Addict Dis. 2013;32(3):263–73.
Zerdazi EH, Curis E, Karsinti E, Icick R, Fortias M, Batel P, et al. Occurrence and severity of cocaine-induced hallucinations: two distinct phenotypes with shared clinical factors but specific genetic risk factors. Drug Alcohol Depend. 2022;232:109270. https://doi.org/10.1016/j.drugalcdep.2022.109270.
Moran LV, Ongur D, Hsu J, Castro VM, Perlis RH, Schneeweiss S. Psychosis with methylphenidate or amphetamine in patients with ADHD. N Engl J Med. 2019;380(12):1128–38. A study that showed the association between new-onset psychosis and the use of prescribed psychostimulants for the treatment of ADHD.
Henning A, Kurtom M, Espiridion ED. A case study of acute stimulant-induced psychosis. Cureus. 2019;11(2):e4126. https://doi.org/10.7759/cureus.4126.
Srisurapanont M, Likhitsathian S, Suttajit S, Maneeton N, Maneeton B, Oon-Arom A, et al. Efficacy and dropout rates of antipsychotic medications for methamphetamine psychosis: a systematic review and network meta-analysis. Drug Alcohol Depend. 2021;219:108467. https://doi.org/10.1016/j.drugalcdep.2020.108467.
Hajebi A, Amini H, Kashani L, Sharifi V. Twelve-month course and outcome of methamphetamine-induced psychosis compared with first episode primary psychotic disorders. Early Interv Psychiatry. 2018;12(5):928–34.
Mitchell DC, Knight CA, Hockenberry J, Teplansky R, Hartman TJ. Beverage caffeine intakes in the U.S. Food Chem Toxicol. 2014;63:136–42.
World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Mental and behavioural disorders due to use of other stimulants, including caffeine, 2019. https://icd.who.int/browse10/2019/en#/F15. Accessed 15 Apr 2023.
World Health Organization. Eleventh Revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-11). Disorders due to use of caffeine, 2023. https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/31898480. Accessed 15 Apr 2023.
Hearn JK, Reiff T, McBride AB, Kelly MB. Caffeine-induced psychosis and a review of statutory approaches to involuntary intoxication. J Am Acad Psychiatry Law. 2020;48(3):376–83.
Hernandez-Huerta D, Martin-Larregola M, Gomez-Arnau J, Correas-Lauffer J, Dolengevich-Segal H. Psychopathology related to energy drinks: a psychosis case report. Case Rep Psychiatry. 2017;2017:5094608.
Wang HR, Woo YS, Bahk WM. Caffeine-induced psychiatric manifestations: a review. Int Clin Psychopharmacol. 2015;30(4):179–82.
Ágoston C, Bernáth L, Rogers PJ, Demetrovics Z. Stress, caffeine and psychosis-like experiences-a double-blind, placebo-controlled experiment. Hum Psychopharmacol. 2022;37(3):e2828. https://doi.org/10.1002/hup.2828.
Lystrup RM, Leggit JC. Caffeine toxicity due to supplement use in caffeine--naïve individual: a cautionary tale. Mil Med. 2015;180(8):e936–40. https://doi.org/10.7205/MILMED-D-15-00045.
Arrojo-Romero M, Armas Barbazán C, López-Moriñigo JD, Ramos-Ríos R, Gurpegui M, et al. Caffeine consumption in a long-term psychiatric hospital: tobacco smoking may explain in large part the apparent association between schizophrenia and caffeine use. Schizophr Res. 2015;164(1–3):234–41.
Krankl JT, Gitlin M. Caffeine-induced mania in a patient with caffeine use disorder: a case report. Am J Addict. 2015;24(4):289–91.
Hedges DW, Woon FL, Hoopes SP. Caffeine-induced psychosis. CNS Spectr. 2009;14(3):127–9.
Fluyau D, Revadigar N. Biochemical benefits, diagnosis, and clinical risks evaluation of Kratom. Front Psychiatry. 2017;8:62.
Tavakoli HR, Buchholz AC, Kabir IK, Deb A, Gayk JN. Kratom: a new product in an expanding substance abuse market. Fed Pract. 2016;33(11):32–6.
Swogger MT, Walsh Z. Kratom use and mental health: a systematic review. Drug Alcohol Depend. 2018;183:134–40.
Leong Bin Abdullah MFI, Singh D, Swogger MT, Rahim AA, Vicknasingam B. The prevalence of psychotic symptoms in kratom (Mitragyna speciosa Korth.) users in Malaysia. Asian J Psychiatr. 2019;43:197–201.
Weiss ST, Douglas HE. Treatment of Kratom withdrawal and dependence with buprenorphine/naloxone: a case series and systematic literature review. J Addict Med. 2021;15(2):167–72.
Vijeepallam K, Pandy V, Kunasegaran T, Murugan DD, Naidu M. Mitragyna speciosa leaf extract exhibits antipsychotic-like effect with the potential to alleviate positive and negative symptoms of psychosis in mice. Front Pharmacol. 2016;7:464.
Johnson LE, Balyan L, Magdalany A, Saeed F, Salinas R, Wallace S, et al. The potential for Kratom as an antidepressant and antipsychotic. Yale J Biol Med. 2020;93(2):283–9.
Davis AK, Arterberry BJ, Xin Y, Agin-Liebes G, Schwarting C, Williams MT. Race, ethnic, and sex differences in prevalence of and trends in hallucinogen consumption among lifetime users in the United States between 2015 and 2019. Front Epidemiol. 2022;2:876706.
Shalit N, Rehm J, Lev-Ran S. Epidemiology of hallucinogen use in the U.S. results from the national epidemiologic survey on alcohol and related conditions III. Addict Behav. 2019;89:35–43.
Liechti ME. Modern clinical research on LSD. Neuropsychopharmacology. 2017;42(11):2114–27. https://doi.org/10.1038/npp.2017.86.
El-Khoury J, Sahakian N. The association of Salvia divinorum and psychotic disorders: a review of the literature and case series. J Psychoactive Drugs. 2015;47(4):286–92.
De Gregorio D, Comai S, Posa L, Gobbi G. D-lysergic acid diethylamide (LSD) as a model of psychosis: mechanism of action and pharmacology. Int J Mol Sci. 2016;17(11):1953.
Kelly JR, Gillan CM, Prenderville J, Kelly C, Harkin A, Clarke G, et al. Psychedelic therapy's transdiagnostic effects: a research domain criteria (RDoC) perspective. Front Psychiatry. 2021;12:800072.
Krebs TS, Johansen PØ. Psychedelics and mental health: a population study. PLoS One. 2013;8(8):e63972. https://doi.org/10.1371/journal.pone.0063972.
Bender D, Hellerstein DJ. Assessing the risk-benefit profile of classical psychedelics: a clinical review of second-wave psychedelic research. Psychopharmacology. 2022;239(6):1907–32.
Nutt D, Carhart-Harris R. The current status of psychedelics in psychiatry. JAMA Psychiatry. 2021;78(2):121–2.
Beck K, Hindley G, Borgan F, Ginestet C, McCutcheon R, Brugger S, et al. Association of ketamine with psychiatric symptoms and implications for its therapeutic use and for understanding schizophrenia: a systematic review and meta-analysis. JAMA Netw Open. 2020;3(5):e204693. https://doi.org/10.1001/jamanetworkopen.2020.4693.
Saiz-Sapena N. Ketamine revisited - new insights into NMDA inhibitors. IntechOpen. 2022. https://doi.org/10.5772/intechopen.95733. Accessed 1 Mar 2023.
Tsai YY, Yang HJ. Ketamine increases positive symptoms more than negative and cognitive ones: a systematic review and meta-analysis. J Subst Use. 2021. https://doi.org/10.1080/14659891.2020.1766127.
Wolf CJH, Beurmanjer H, Dijkstra BAG, Geerlings AC, Spoelder M, Homberg JR, et al. Characterization of the GHB withdrawal syndrome. J Clin Med. 2021;10:2333.
Arunogiri S, Moayeri F, Crossin R, Killian JJ, Smith K, Scott D, et al. Trends in gamma-hydroxybutyrate-related harms based on ambulance attendances from 2012 to 2018 in Victoria, Australia Addiction. 2020;115:473–9.
Sarkanen T, Niemelä V, Landtblom AM, Partinen M. Psychosis in patients with narcolepsy as an adverse effect of sodium. Front Neurol. 2014;5(136):1–5.
Doyno CR, White CM. Sedative-hypnotic agents that impact gammaaminobutyric acid receptors: focus on flunitrazepam, gammahydroxybutyric acid, phenibut, and selank. J Clin Pharmacol. 2021;61:S114–28. https://doi.org/10.1002/jcph.1922.
Buckley PJ, Wolf CT. Psychosis in a 22-year-old woman with narcolepsy after restarting sodium oxybate. Psychosomatics. 2018;59(3):298–301.
Chien J, Ostermann G, Turkel SB. Sodium oxybate-induced psychosis and suicide attempt in an 18-year-old girl. J Child Adolesc Psychopharmacol. 2013;23(4):300–1.
Claussen MC, Hassanpour K, Jenewein J, Boettger S. Catatonic stupor secondary to gamma-hydroxy-acid (GHB) dependence and withdrawal syndrome. Psychiatr Danub. 2014;26(4):358–9.
Cagnin A, Pompanin S, Manfioli V, Briani C, Zambon A, Saladini M, et al. γ- Hydroxybutyric acid-induced psychosis and seizures. Epilepsy Behav. 2011;21(2):203–5.
Langford J, Gross WL. Psychosis in the context of sodium oxybate therapy. J Clin Sleep Med. 2011;7(6):665–6.
Kamal RM, van Noorden MS, Wannet W, Beurmanjer H, Dijkstra BA, Schellekens A. Pharmacological treatment in γ-Hydroxybutyrate (GHB) and γ-Butyrolactone (GBL) dependence: detoxification and relapse prevention. CNS Drugs. 2017;31(1):51–64.
Diestelmann M, Zangl A, Herrle I, Koch E, Graw M, Paul LD. MDPV in forensic routine cases: psychotic and aggressive behavior in relation to plasma concentrations. Forensic Sci Int. 2018;283:72–84.
Stevenson R, Tuddenham L. Novel psychoactive substance intoxication resulting in attempted murder. J Forensic Legal Med. 2014;25:60–1.
Weinstein AM, Rosca P, Fattore L, London ED. Synthetic cathinone and cannabinoid designer drugs pose a major risk for public health. Front Psychiatry. 2017;8:156. https://doi.org/10.3389/fpsyt.2017.00156.
Bretteville-Jensen AL, Tuv SS, Bilgrei OR, Fjeld B, Bachs L. Synthetic cannabinoids and cathinones: prevalence and markets. Forensic Sci Rev. 2013;25(1–2):7–26.
Chang HM, Huang MH, Pan CH, Chen LY. Psychiatric profiles and clinical manifestations of cathinone users: case series of analytically confirmed cathinone use in Taiwan. J Addict Addictv Disord. 2019;6:23.
Oliver CF, Palamar JJ, Salomone A, Simmons SJ, Philogene-Khalid HL, Stokes-McCloskey N, Rawls SM. Synthetic cathinone adulteration of illegal drugs. Psychopharmacology. 2019;236:869–79.
Mas-Morey P, Visser MH, Winkelmolen L, Touw DJ. Clinical toxicology and management of intoxications with synthetic cathinones (“balt salts”). J Pharm Pract. 2013;26(4):353–7.
SAMHSA. 2018 National Survey on drug use and health: methodological summary and definitions. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; 2019. https://www.datafiles.samhsa.gov/. Accessed 1 Sept 2023.
Vasilov A, Nandu B, Berman J. Treatment modules and therapeutic approaches for inhalant abuse: a case report. Psychiatr Ann. 2013;43(9):419–23.
Narayanaswamy JC, Viswanath B, Ravi M, Muralidharan K. Inhalant dependence: data from a tertiary care center in South India. Indian. J Psychol Med. 2012;34(3):232–6.
Mustonen A, Niemelä S, McGrath JJ, Murray GK, Nordström T, Mäki P, et al. Adolescent inhalant use and psychosis risk - a prospective longitudinal study. Schizophr Res. 2018;201:360–6.
Sarkar S, Bhatia G, Dhawan A. Clinical practice guidelines for assessment and management of patients with substance intoxication presenting to the emergency department. Indian J Psychiatry. 2023;65(2):196–211.
Wada K, Nakayama K, Koishikawa H, Katayama M, Hirai S, Yabana T, et al. Symptomatological structure of volatile solvent-induced psychosis: is "solvent psychosis" a discernible syndrome? Japanese Journal of Alcohol Studies and Drug Dependence. 2005;40(5):471–84.
Stein Y, Finkelstein Y, Levy-Nativ O, Bonne O, Aschner M, Richter ED. Exposure and susceptibility: schizophrenia in a young man following prolonged high exposures to organic solvents. Neurotoxicology. 2010;31(5):603–7.
Funding
None.
Author information
Authors and Affiliations
Contributions
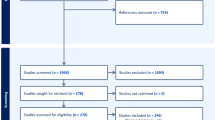
L.T. was responsible for conceiving, designing, and planning the paper. The database literature search was done by L.T., M.P., and Z.K.P. L.T. and M.P. wrote the first draft of the article. L.T., M.P., and Z.K.P. critically revised the article for important intellectual content. L.T., M.P., and Z.K.P. approved the final version and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethical Approval
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tomašić, L., Peček, M. & Petrović, Z.K. Substance-Induced Psychosis: a Narrative Review. Curr Addict Rep 11, 55–67 (2024). https://doi.org/10.1007/s40429-023-00528-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40429-023-00528-w