Abstract
Purposeof Review
The prevalence of problematic substance use is disproportionately higher among sexual and gender minority (SGM) adults compared to adults in the general population. mHealth as a treatment modality could reduce barriers to accessing substance use treatments among SGM populations. Through a qualitative literature search, the current narrative review aimed to understand the lived experiences of SGM individuals who use substances and to synthesize recommendations made in the literature to inform future mHealth interventions.
Recent Findings
Positive and negative reinforcement motives were prominent reasons for substance use, which included SGM identity expression and conformity motives. Individual- and system-level treatment barriers included a lack of safe and nonjudgmental environment, shame and stigma, and limited knowledge about treatment options. Barriers were directly linked to the reported substance use treatment needs in this population.
Summary
On-demand app features, real-time intervention and assessment, and anonymity should be considered in future mHealth trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sexual and gender minority (SGM) individuals are those who identify as, but not limited to, lesbian (L), gay (G), bisexual (B), queer, and/or asexual (i.e., sexual minority), transgender (T), and/or nonbinary (i.e., gender minority) [1, 2]. The most recent Gallup survey in 2022 reported that 7.2% of the adults in the United States (US) self-identified as lesbian, gay, bisexual, transgender (LGBT), or something else other than heterosexual [3]. The prevalence of substance use is disproportionately higher among SGM adults compared to general population. For example, in the National Survey on Drug Use and Health 2020, the prevalence of having a substance use disorder was twice as high for LGB adults versus the general population (34.2% vs 15.4%, respectively) [4]. Further, substance use (i.e., not just those with substance use disorders) is associated with several other physical and behavioral health concerns among SGM individuals, such as unprotected sex [5, 6], nonadherence to HIV medication [7], and partner abuse [8]. Therefore, there is a critical need to develop interventions to reduce problematic substance use among this vulnerable population.
Previous studies have found promising results when using behavioral interventions for the treatment of problematic substance use in the SGM population [9••]. However, the majority of extant studies have focused on specific substances such as alcohol, tobacco, or methamphetamine, and most study samples have consisted of sexual minority men [9••]. Further, multiple factors may hinder enrollment in substance use treatment for SGM individuals, such as a lack of substance use programs tailored to the needs of the SGM population [10]. SGM individuals anticipate discrimination and rejection in treatment [11]. This finding is aligned with the Minority Stress Model that posits that behavioral health disparities in SGM populations are explained by the experience of repeated prejudicial events, expectations of discrimination and rejection, concealment of SGM status, and internalized stigma [12]. Indeed, a previous study reported that SGM individuals suffer discrimination while undergoing substance use treatment, which in turn negatively impacted recovery [13]. Moreover, the stigma associated with both SGM identity and substance use may explain why confidentiality is a major concern for this population [14, 15••]. Given these multiple barriers, satisfaction and retention in traditional substance use programs is lower among SGM individuals as compared to non-SGM individuals [16]. In this context, interventions provided through mobile devices (e.g., mHealth) may be suitable to address the needs of this vulnerable population to increase access. Indeed, a recent review on virtual and web-based digital health interventions targeting mental health issues or tobacco use demonstrated a preference for digital treatment programs among SGM individuals [15••]. Comparable treatment adherence rates were reported between SGM and non-SGM individuals, and significant improvement in the indices of emotional difficulties (e.g., depression) and tobacco use among SGM individuals were also found [15••], further supporting the potential for mHealth modality.
There are only a few mHealth trials that have been conducted to address problematic substance use among SGM individuals. A three-arm randomized control trial that examined the efficacy of a text-based methamphetamine intervention found a reduction in the frequency of having unprotected sex and having sex under the influence of methamphetamine among those randomized to active treatment conditions (from baseline to 9-months post randomization) [17]. In a small pilot mHealth study for alcohol use among 8 men who have sex with men (MSM), sending text messages to increase safe sex practices and reduce alcohol use led to reduced heavy drinking frequency and an increase in self-efficacy related to safe sex [18]. However, mHealth substance use intervention trials among other SGM subpopulations who use various types of substance are extremely limited. Technology could be leveraged to address the diversity of SGM subpopulations enrolling in treatment, improve retention rates, and maximize treatment effectiveness. Although its efficacy and acceptability have been supported in the general population [19••], mHealth substance use interventions among SGM individuals remain scant [15••].
Understanding the needs of SGM populations regarding substance use treatment could inform the development of future treatments, including interventions that leverage mHealth. This narrative review aims to better understand the lived experiences of SGM individuals who use substances and to identify potential targets that could be addressed in an mHealth intervention for substance use tailored to this population. To the best of our knowledge, there is no known mHealth literature that critically assesses and synthesizes perspectives, processes, and contextual factors of substance use and treatment needs among SGM individuals that can be effectively captured via a qualitative approach [20]. Thus, we reviewed the literature of qualitative studies published in the last few years to summarize extant qualitative findings on the SGM adults’ unique needs for substance use treatment and recommendations made in the literature to identify areas of improvement. We also discuss considerations for future mHealth interventions targeted to this group. The goal of this narrative review is to answer the following: (1) What are the contextual factors associated with problematic substance use among SGM adults with lived experiences? (2) What are the unique needs of SGM adults who engage in problematic substance use? Problematic substance use was broadly defined as the use of any illicit substances and/or use of other substance for different reasons other than as prescribed or that led to adverse intrapersonal or interpersonal consequences.
Method
Search strategy
A medical librarian at the H. Lee Moffitt Cancer Center & Research Institute developed a search strategy to capture the following key concepts: Sexual and gender minorities, substance use, and qualitative research. The bibliographic search was conducted on August 18, 2022 in Ovid MEDLINE® ALL (i.e., 1946 to August 17, 2022) to capture any scientific papers, as we were unsure how many qualitative articles there would be in this domain. Full search terms using Medical Subject Headings (MeSH) and keywords are presented in Supplementary Material 1.
Eligibility criteria and selection process
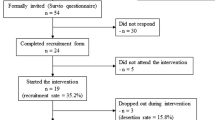
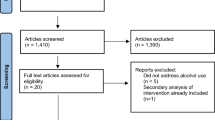
The inclusion criteria were: (1) SGM adults (≥ 18 years old) as the target study population, (2) using any modality of qualitative research methods (e.g., qualitative in-depth interviews/questions or focus groups), and (3) the studies’ primary outcome was substance use behavior and/or experiences with substance use treatment. Studies with no original data collection (e.g., commentaries, protocols) and those in a language other than English were excluded. Following the identification of the articles, titles and abstracts were screened for inclusion by the first author (MJY). Selected articles that were published within the past 5 years were subjected to full-text review to capture most up-to-date qualitative findings in the literature. We also reviewed the articles published between 2012 and 2016 (n = 9 that met the inclusion criteria) to determine if any different/new themes would emerge. After a thorough review, no different/new themes were identified from the articles published between 2012 and 2016. Additionally, we included two articles on smoking that were not retrieved in our initial search but we became aware of through hand search during the review process. Thus, a total of 25 articles published between 2017 and 2022 were included in our review. During the review of the 25 articles, we focused on content that was exclusively relevant to problematic substance use and/or substance use treatment reported by SGM adults and did not include information irrelevant to the aim of the current review or those reported by providers. The PRISMA flow diagram presents the overview of the selection process (Fig. 1).
Results
Study Characteristics
Table 1 contains the study characteristics of the 25 articles included in this narrative review. No qualitative studies were found on mHealth for substance use among SGM adults. Regarding qualitative research methods, 17 studies (68%) conducted semi-structured interviews, 6 studies (24%) conducted focus groups, 1 study (4%) conducted a problem-centered interview, and 1 study (4%) asked participants open-ended qualitative questions as part of a survey. In terms of gender identity,Footnote 1 16 studies (64%) exclusively included individuals who identified as male, 6 studies (24%) included those who identified as female, and 8 studies (32%) recruited transgender individuals in their sample (3 studies with transgender men, 6 studies with transgender women, and 2 studies did not specify). Regarding sexual orientation, 15 studies (60%) reported sexual orientation as part of their sample characteristics whereas 10 studies (40%) did not report information on sexual orientation (although 4 included individuals with diverse sexual orientation per their eligibility criteria). It is notable that the study populations in 9 of those 10 studies were solely composed of MSM. Regarding types of substance use, 9 studies (36%) focused on a single substance (4 studies on alcohol; 2 studies on cigarette smoking; 2 studies on methamphetamine; 1 study on Gamma-hydroxybutyrate [GHB]), 12 studies (48%) addressed polysubstance use, and 4 studies (16%) did not specify the type of substance. In addition, 9 studies (36%) focused on chemsex (substance use as part of sexual activity) and 8 studies (32%) focused on chemsex among gay, bisexual, and/or other men who have sex with men (GBMSM). The majority of studies were conducted in the United States (n = 11; 44%) and the United Kingdom (n = 4; 16%). The age range was 18 to 71, but 2 studies did not report the age of their samples and 3 studies did not report the age range. Below, we summarize observed themes from the literature review and also note unique themes relevant to GBMSM and/or chemsex given their significant representations in the reviewed studies.
Lived Experiences of Problematic Substance Use
Four categories regarding the lived experiences of problematic substance use were identified: (1) Reasons/Motives for using substances, (2) Awareness of the negative consequences of substance use, (3) Barriers to substance use treatment, and (4) Needs for future substance use treatment (Table 2).
Reasons/Motives for using substances
Positive and negative reinforcement were two of the main motives identified within the reviewed articles for substance use. In terms of positive reinforcement, participants from 15 studies (60%) reported social facilitation as a main motive for substance use [21, 22••, 23••, 24,25,26,27,28,29,30,31,32,33,34]. Specifically, SGM individuals noted that substance use is a typical social activity in the SGM communities [23••, 24, 27,28,29, 31, 32, 34] and that it helps with enhancing belongingness and participation in SGM social circles [22••, 23••, 25, 27, 28, 30, 32, 33]. In particular, GBMSM or individuals who engage in chemsex reported that substance use helps with finding sexual partners [27, 30] and maintaining relationships with partners [21, 22••, 26]. One study reported that the COVID-19 pandemic increased their alcohol and marijuana use as a social facilitator under shelter-in-place orders [35]. Enhancement motives were reported in 8 studies (32%) such that substance use helped enhance positive affect and sensations (e.g., relaxation, peace; [21, 23••]), perceived partner’s attractiveness [33], sexual arousal [33], sexual experiences (e.g., sexual pleasure; [21, 22••, 25, 27,28,29, 33]), and sexual performance [29, 33]. These enhancement motives were evident among GBMSM, in particular, individuals who engage in chemsex. Participants from 8 studies (32%) stated that substance use helped them express their SGM identity [31, 36] by increasing the perceived connection to their own SGM identity [21], self-esteem [25], and confidence [21, 30, 32, 34].
Negative reinforcement was another prominent motive. SGM individuals from 11 studies (44%) reported that substance use helped them cope with general stress [36, 37] and SGM-related stress such as negative affect (e.g., shame, inadequacy, emotional pain [22••, 23••, 25, 26, 33, 36,37,38]), internalized/societal stigma [23••, 28, 33, 38], identity concealment [36, 38], fear of identity disclosure [37, 38]/rejection [33], lack of social support (e.g., rejection, [26, 28, 38]), and intersection of stress from SGM identity and social rejection [36,37,38]. Further, GBMSM participants reported that substance use helped manage stress from mental health concerns [26] and HIV status [24, 33]. One study reported that SGM individuals consumed alcohol and used marijuana to cope with stress and boredom during the COVID-19 pandemic [35]. Conformity motives were also reported in 6 studies (24%) [25, 31, 37,38,39,40]. In particular, SGM individuals reported using substances to conform with peer pressure, such as expectations on substance use in social settings [25, 31, 40] or to “fit in” [37, 38]. Among GBMSM, peers’ expectation on sexual performance was reported as one of the conformity motives [39].
Other contextual factors that influence using substances also emerged. Two studies (8%) reported that SGM individuals, who engage in chemsex, used substances because of their perceived confidence in the ability to use substances safely. For example, they felt they were knowledgeable about implementing safety and harm reduction measures, such as preplanning to reduce any complications after substance use (e.g., schedule chemsex to limit interferences with work, logistics of substance use; [40]), using hygienic measures (e.g., use clean needles; [40]), knowing what to do when someone is in “GHB sleep” [21], being careful with dosing and timing [21], and using substances only when with reliable people [21, 40]. Two other studies (8%) among GBMSM reported contextual factors that promote drug use such as different types of substances being preferred in different generations (e.g., those older than 35 years use crack/heroin [26]) and social circumstances regarding route of substance use administration (e.g., intravenous use of heroin/methamphetamine not being acceptable at a nightclub or bar but allowable to use in private places, [27]). Participants in one study noted cue-provoked urge to use substances in their environment (e.g., usual context of smoking, [36]). One study reported how the COVID-19 pandemic could have contributed to increased use, as individuals had more time to use/explore alcohol and marijuana after losing daily routines because of a stay home order [35]. Lastly, one study among GBMSM reported that substance use behaviors (e.g., decrease in the use frequency) change over time given the shifts in their life priorities and social circle [27].
Awareness of the negative consequences of substance use
SGM individuals reported being aware of possible negative consequences following substance use, as indicated by participants from 11 studies (44%) [21, 22••, 24, 25, 29, 30, 32, 34, 35, 39, 40]. For example, individuals who engage in chemsex reported that safety practices were put in place when using substances to avoid the risk of overdose, in particular, when using more than one drug concurrently [21]. Among GBMSM who engage in chemsex, scheduling drug use accounting for a time to recover from lingering negative effects to minimize the interference with other responsibilities was also part of the safety practices [40]. GBMSM and/or individuals who engage in chemsex acknowledged the various costs associated with substance use, such as missing out on enjoyable activities [22••] that they used to enjoy [30], having unstable interpersonal relationships resulting in distress (e.g., feeling used, [22••, 24]), engaging in polysubstance use [39], sexual risk behaviors (e.g., HIV transmission, condomless sex [24, 25, 29, 32]), and other unintended negative consequences (e.g., sexual violence, black out, [21, 32]). Interference with day-to-day activities was noted as a marker of problematic drinking [34]. Two studies among GBMSM (8%) also noted a lack of knowledge on how to minimize negative consequences [39, 40].
Barriers to substance use treatment
Many studies assessed and/or identified perceived barriers to substance use treatment. Eight studies (32%) identified system-level barriers such as low accessibility to adequate treatment for SGM individuals due to too high burden in navigating substance use referrals [29, 37, 41], safety concerns regarding the location of the clinics [41], high treatment cost [37], and difficulty finding providers trained in and services that meet the need of SGM individuals [26, 29, 40, 42]. In particular, among GBMSM who engage in chemsex, lack of a safe and nonjudgmental environment to openly discuss their substance use and/or chemsex [40] was also mentioned as a system-level barrier, given limited laws and policies to support the rehabilitation of these individuals [23••, 28]. At the individual-level, seven studies (28%) noted shame and stigma associated with drug use [28] and SGM status [41] such as fear of disclosing their sexual practices [40, 42] in particular among GBMSM who engage in chemsex, low self-efficacy for abstinence [37], and pharmacotherapy for substance use perceived as a replacement of one substance for another [34, 43]. Two studies (8%) noted limited knowledge about available treatment options with a harm reduction approach [43] and pharmacological treatment [34, 43], and concerns about the pharmacotherapy (e.g., side effects, [34]). Other barriers identified by a few studies included the social norms surrounding the use of certain substances [23••, 35, 37], fear of losing perceived gains from substance use (e.g., self-confidence) [30], and beliefs that one should be motivated to be treated [34].
Needs for future substance use treatment
Unmet needs in current substance use treatment for SGM were assessed in some studies. One prominent theme was provision of psychoeducation on harm reduction, short/long-term negative consequences of substance use, and coping strategies, which emerged in 6 studies (24%) [28, 34, 36, 37, 40, 43]. GBMSM were interested in learning how to use drugs safely as an alternative to complete abstinence [34, 43]. Participants suggested providing psychoeducation on various options of substance use treatment (e.g., harm reduction, pharmacotherapy) [37, 43] and potential drug interactions for transgender individuals receiving hormone therapy [43] as well as reliable harm reduction guidelines (e.g., dosing, safe chemsex, what to do in emergency, [40]). Providing psychoeducation to teach coping skills [36, 37] and to promote awareness of the negative consequences of substance use was also recommended (e.g., cost or changes in health associated with continuous substance use [36, 37]) by using places where SGM individuals socialize (e.g., social media, bars, [28]). Four studies (16%) [28, 37, 40, 42] noted that key needs in substance use treatment were enhancing treatment accessibility. For example, participants suggested having providers and clinic staff with a nonjudgmental attitude and extensive knowledge in SGM health, and providing a safe environment, given shame and stigma that challenge getting appropriate care (e.g., sexual health while using drugs, [28, 36, 37, 40]). Societal support to promote a change in the norm regarding substance use and for safe drug use and harm reduction within SGM communities (e.g., peer support) arose as another key component of substance use treatment among 5 studies (20%) [34, 36, 37, 44, 45]. For example, GBMSM who completed treatment reported having peers to share long-term perspectives on various harms associated with substance use (e.g., HIV infection) and making connections to peers who support their behavior change were helpful [45].
Recommendations for Substance Use Treatment for SGM Individuals made in the Reviewed Studies
Here, we summarize the recommendations made in the reviewed studies over the past 5 years, for substance use treatment for SGM individuals, which fall into two categories: (1) Eliminating treatment barriers and (2) Treatment approach and components. These recommendations combined with the themes above were synthesized to make recommendations for future mHealth trials in the Discussion.
Eliminating treatment barriers
Several studies provided recommendations to eliminate potential barriers to access substance use treatment: (1) Creating a safe and nonjudgmental environment to destigmatize substance use, in particular, for transgender individuals [43]. Specific suggestions included having SGM-related images, SGM-identified staff, SGM-inclusive procedures such as including questions on sexual orientation, gender identity, pronouns, and using SGM-friendly language (e.g., “relationship status vs marital status”) [38]. Having a nonjudgmental attitude was specifically highlighted for chemsex (e.g., acknowledging complex contextual factors leading to substance use). Studies also recommended validating the role that minority stress plays in substance use and addressing sexual wellness so that SGM individuals can openly discuss their substance use in the context of sexual practices [22••, 40]. Promoting anonymity and confidentiality was recommended as a key component to alleviate treatment barriers and create a safe welcoming environment [38, 40]. (2) Studies also recommended improving the referral network to substance use treatment [29, 41], providing brief interventions at the patient encounter (e.g., motivational interviewing, [32, 37]) and having a peer navigator [41] to overcome barriers related to a complicated health care system. (3) Providing and developing peer/social support as part of the substance use treatment were also recommended to facilitate behavior change [24,25,26, 45]. Other recommendations included holding community events without promoting substance use [27] and sending text messages or having advertisements on social media to promote health behaviors when mass events (e.g., music festivals) with high substance use take place (e.g., safety measures for chemsex [28]).
Treatment approach and components
Common themes arose across studies regarding treatment approach. (1) Given the perceived gains from engaging in substance use [22••], a harm reduction approach to promote safe use [21, 28, 37, 45] was recommended as opposed to complete abstinence [27, 29, 43] with the aim of preventing or mitigating negative consequences such as overdose, HIV, or sexually transmitted infections [21, 28, 45]. (2) Several studies recommended including educational modules as part of substance use treatment programs or relevant services that address the negative consequences of substance use (e.g., overdose, violence, [21], medical emergency, [39]), safe sex (e.g., sexual health, [27]), and pharmacotherapy options [37, 43]. Additionally, this information should come from reliable sources and be easily accessible [40], in particular, in places and times in which heavy substance use is expected [28, 42]. (3) Several studies recommended that the complexity of factors (e.g., contextual factors, unique pathways) leading to substance use among SGM individuals should be acknowledged in treatment [34]. For example, perceived gains from engaging in substance use [22••, 33], trauma history [23••], negative affect [35], minority stress [24, 35, 37], intersectionality of multiple identities [24, 31], pain [26], and sexual behavior [24] should be taken into consideration in substance use treatment. In particular, assessing sexual activity and discussing sexual concerns are crucial for SGM individuals who engage in chemsex [22••]. (4) Some studies also recommended reinforcing protective and resilient factors (e.g., optimism, supportive relationships, [24]) to mitigate minority stress [25] and affirm SGM identity [38]. (4) Teaching coping skills to manage minority stress and seeking appropriate social support was also recommended [22••, 36, 37].
Discussion
mHealth for substance use among SGM individuals is still in its infancy. To inform future mHealth interventions targeted to this population, the current manuscript reviewed the literature on the lived experience of SGM adults regarding problematic substance use as well as recommendations made for substance use treatment based on qualitative studies published between January 2017 and August 2022. Of note, our literature search did not identify any qualitative mHealth studies among SGM individuals regarding substance use. Our review did not include studies among SGM adolescents.
Based on this review of the literature, we believe that serious consideration should be given to the potential of mHealth interventions for the SGM population. Given concerns about confidentiality and minority stress, mHealth has the ability to expand reach and uniquely address such needs. Indeed, the vast HIV literature has reported that SGM individuals perceive mHealth interventions to be useful in addressing barriers to appropriate health care services and in obtaining basic health education [46] and a preference has been reported for online/smartphone apps over in-person interventions for HIV prevention [47]. Evidence shows that mHealth social media and mobile networking apps are more effective in reaching and enrolling diverse SGM individuals for broad clinical research [48] including those who use substances, as compared to in-person approaches [49].
Early mHealth substance use trials in this population have implemented some of the recommendations made in the literature (e.g., peer support, HIV prevention messages) by using text messages [17, 18]. To consider ways to address this population’s needs by leveraging technology, we list several considerations and recommendations for future mHealth research (Table 2). First, education on treatment options and safe substance use can be effectively delivered in various ways, on-demand or in real-time. For example, using a smartphone app, safety measures, treatment options, and resources for relevant treatment could be provided whenever needed. In particular, a direct link to a phone number or to relevant resources, as provided on the app or via text messages, could increase substance use treatment reach, since it would take only one click to access appropriate services (e.g., safe sex, needle use, peer support, [50]). Second, some treatment barriers could be easily addressed given their immediate availability. Information on safety measures or support could be provided in advance, either via texts or messages within an app, before individuals are at the places and times when heavy substance use is expected. Tracking technology such as ecological momentary assessments (EMA) or GPS might serve such purpose, although its acceptability should be assessed through future qualitative studies. A welcoming environment by using SGM-affirming images and language as well as a space for an anonymous support group could also be provided on the app.
Third, just-in-time adaptive interventions (JITAIs) could be effectively applied for substance use treatment among this population. Micro-randomized trial designs could be applied to examine the unique effect of general (e.g., craving) and SGM-specific (e.g., minority stress [12], salience of SGM identity, [51]) interventions on proximal outcomes related to substance use when SGM individuals report heightened craving or SGM-specific cognitive-affective processes. Also, on-demand support that branches to specific coping strategies based on the participants’ momentary needs could be available. For example, when experiencing high craving, an individual can initiate the on-demand process by indicating high craving, which could subsequently trigger assessment of their momentary need (e.g., reduce craving, reminder of their treatment goal) and then relevant coping strategies (e.g., emotion regulation [52]). Lastly, given confidentiality and anonymity in treatment are concerns among SGM individuals, additional protection should be implemented. For example, the app should be password locked and the language used in notifications should be carefully written. Indeed, within the context of existing HIV literature on mHealth, SGM individuals suggested clarifying privacy and confidentiality upfront including visual aspects of the app (e.g., icon of the app) and password protection, which may affect willingness to engage in the intervention [46].
Limitations of the current review include the majority of the studies being focused on men and chemsex, as well as not including quantitative studies, which was outside the scope of this narrative review. Although the current review aimed to identify unique needs of SGM adults by reviewing the qualitative literature on this population, there are likely some overlapping needs identified here that are broadly applicable to other populations. As such, future studies may include a comparison group of non-SGM adults to disentangle the SGM-specific needs from more general needs in substance use treatment, as well as SGM adolescents (e.g., [53, 54]). It is notable that a few studies had a small sample size (N < 10), however the themes observed in these studies were consistent with the other studies reviewed. We also want to highlight the limitations in the extant qualitative literature that we reviewed. Overall, this area of research is limited to certain types of drugs and sexual behaviors, and certain subtypes of SGM individuals. For example, most papers were focused on HIV prevention, and sexual minority women and gender minority individuals were not well represented. Some papers did not report sexual orientation or distinguish sexual orientation from gender identity. Idiosyncrasies among SGM subpopulations has been recognized given, for example, bisexual individuals are more prone to experience minority stress and emotional difficulties than lesbian/gay individuals [55, 56], highlighting the importance of correctly identifying the population. Given the large representation of GBMSM in this review, caution is needed when considering the current findings for future treatment development.
Conclusions
The current review identified the lived experiences of problematic substance use among SGM adults and their needs in substance use treatment. Based on the recommendations made in the literature, we presented considerations in study methodologies for future mHealth substance use treatments. If mHealth-based substance use treatment is found effective, its potential in scalability and public health benefit would be immense.
Notes
Note that the studies counted for each category are not mutually exclusive. For example, some studies recruited both those identifying as female and transgender.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
National institutes of health sexual and gender minority research coordinating committee. NIH FY 2016–2020 strategic plan to advance research on the health and well-being of sexual and gender minorities. 2015. https://www.edi.nih.gov/sites/default/files/EDI_Public_files/sgm-strategic-plan.pdf. Accessed 23 Mar 2023.
National academies of sciences, engineering, and medicine. Measuring sex, gender identity, and sexual orientation. Washington, DC: The National Academies Press; 2022. https://doi.org/10.17226/26424.
Jones JM. U.S. LGBT identification steady at 7.2%. Gallup. 2023. https://news.gallup.com/poll/470708/lgbt-identification-steady.aspx. Accessed 22 Feb 2023.
Substance Abuse and Mental Health Services Administration. 2020 National survey on drug use and health: Lesbian, Gay, and Bisexual (LGB) Adults. In: 2020 National Survey of Drug Use and Health (NSDUH) Releases. 2022. https://www.samhsa.gov/data/sites/default/files/reports/slides-2020-nsduh/2020NSDUHLGBSlides072522.pdf. Accessed 8 Feb 2023.
Vosburgh H, Mansergh G, Sullivan PS, Purcell DW. A review of the literature on event-level substance use and sexual risk behavior among men who have sex with men. AIDS Behav. 2012;16(6):1394–410.
Vagenas P, Lama JR, Ludford KT, Gonzales P, Sanchez J, Altice FL. A systematic review of alcohol use and sexual risk-taking in Latin America. Rev Panam Salud Publica. 2013;34(4):267–74.
Moore DJ, Blackstone K, Woods SP, Ellis RJ, Atkinson JH, Heaton RK, et al. Methamphetamine use and neuropsychiatric factors are associated with antiretroviral non-adherence. AIDS Care. 2012;24(12):1504–13.
Houston E, McKirnan DJ. Intimate partner abuse among gay and bisexual men: Risk correlates and health outcomes. J Urban Health. 2007;84(5):681–90.
•• Kidd JD, Paschen-Wolff MM, Mericle AA, Caceres BA, Drabble LA, Hughes TL. A scoping review of alcohol, tobacco, and other drug use treatment interventions for sexual and gender minority populations. J Subst Abus Treat. 2022;133:108539. A scoping review on the non-mHealth substance use treatment for SGM individuals. The paper presents the types of samples, study design, outcome measures, and their impact in changing substance use behaviors.
Mericle AA, de Guzman R, Hemberg J, Yette E, Drabble L, Trocki K. Delivering LGBT-sensitive substance use treatment to sexual minority women. J Gay Lesbian Soc Serv. 2018;30(4):393–408. https://doi.org/10.1080/10538720.2018.1512435.
Dearing RL, Hequembourg AL. Culturally (in) competent? Dismantling health care barriers for sexual minority women. Soc Work Health Care. 2014;53(8):739–61.
Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2013;129(5):674.
Lombardi E. Substance use treatment experiences of transgender/transsexual men and women. J LGBT Health Res. 2007;3(2):37–47.
Mayer KH, Bradford JB, Makadon HJ, Stall R, Goldhammer H, Landers S. Sexual and gender minority health: what we know and what needs to be done. Am J Public Health. 2008;98(6):989–95.
•• Whaibeh E, Vogt EL, Mahmoud H. Addressing the behavioral health needs of sexual and gender minorities during the COVID-19 Pandemic: a Review of the expanding role of digital health technologies. Curr Psychiatry Rep. 2022:24:387–97. A review on the role of digital health modality for overall behavioral health interventions among SGM individuals. This review identifies advantages and crucial gaps in the extant digital health interventions at both patient and provider levels.
Senreich E. A comparison of perceptions, reported abstinence, and completion rates of gay, lesbian, bisexual, and heterosexual clients in substance abuse treatment. J Gay Lesbian Mental Health. 2009;13(3):145–69.
Reback CJ, Fletcher JB, Swendeman DA, Metzner M. Theory-based text-messaging to reduce methamphetamine use and HIV sexual risk behaviors among men who have sex with men: automated unidirectional delivery outperforms bidirectional peer interactive delivery. AIDS Behav. 2019;23(1):37–47.
Chavez K, Palfai TP. Feasibility of a mobile messaging-enhanced brief intervention for high risk heavy drinking MSM: A pre-pilot study. Alcohol Treat Q. 2020;38(1):87–105.
•• Carreiro S, Newcomb M, Leach R, Ostrowski S, Boudreaux ED, Amante D. Current reporting of usability and impact of mHealth interventions for substance use disorder: A systematic review. Drug Alcohol Depend. 2020;215:108201. A systematic review on the challenges in mHealth modality, types of outcomes, acceptability, and usability for substance use treatments. A recommended read to understand the recent mHealth methodology, intervention approach, and outcomes among non SGM individuals.
Maxwell JA. Why qualitative methods are necessary for generalization. Qualitative Psychology. 2021;8(1):111.
Freestone J, Prestage G, Bourne A, Ezard N, Race K, Nedanoski A, et al. Controlling for pleasure and risk: The experiences of sexuality and gender diverse people who use GHB. Int J Drug Policy. 2022;105:103747. https://doi.org/10.1016/j.drugpo.2022.103747.
•• Stanton AM, Wirtz MR, Perlson JE, Batchelder AW. “It’s how we get to know each other”: Substance use, connectedness, and sexual activity among men who have sex with men who are living with HIV. BMC Public Health. 2022;22(1):425. https://doi.org/10.1186/s12889-022-12778-w. A qualitative study that examined the perceived role of substance use to feel connected and belonged to the community. A recommended read as the study highlights that the function of drug use should be acknowledged in substance use treatment for MSM rather than focusing on its adverse impact (or total abstinence).
•• Tan RKJ, Phua K, Tan A, Gan DCJ, Ho LPP, Ong EJ, et al. Exploring the role of trauma in underpinning sexualised drug use ('chemsex’) among gay, bisexual and other men who have sex with men in Singapore. Int J Drug Policy. 2021;97:103333. https://doi.org/10.1016/j.drugpo.2021.103333. An exemplary qualitative study that raises an important issue in the terms used to describe drug use during sex acknowledging stigma attached to chemsex.
Maiorana A, Kegeles SM, Brown S, Williams R, Arnold EA. Substance use, intimate partner violence, history of incarceration and vulnerability to HIV among young Black men who have sex with men in a Southern US city. Cult Health Sex. 2021;23(1):37–51. https://doi.org/10.1080/13691058.2019.1688395.
Ogunbajo A, Iwuagwu S, Williams R, Biello KB, Kahler CW, Sandfort TGM, et al. Experiences of minority stress among gay, bisexual, and other men who have sex with men (GBMSM) in Nigeria, Africa: The intersection of mental health, substance use, and HIV sexual risk behavior. Glob Public Health. 2021;16(11):1696–710. https://doi.org/10.1080/17441692.2020.1834598.
Dangerfield Ii DT, Heidari O, Cooper J, Allen S, Lucas GM. Motivations for opioid and stimulant use among drug using black sexual minority men: A life course perspective. Drug Alcohol Depend. 2020;215:108224. https://doi.org/10.1016/j.drugalcdep.2020.108224.
Hawkins B, Armstrong HL, Kesselring S, Rich AJ, Cui Z, Sereda P, et al. Substance Use as a Mechanism for Social Inclusion among Gay, Bisexual, and Other Men Who Have Sex with Men in Vancouver. Canada Subst Use Misuse. 2019;54(12):1945–55. https://doi.org/10.1080/10826084.2019.1621901.
Tan RKJ, Wong CM, Chen MI, Chan YY, Bin Ibrahim MA, Lim OZ, et al. Chemsex among gay, bisexual, and other men who have sex with men in Singapore and the challenges ahead: A qualitative study. Int J Drug Policy. 2018;61:31–7. https://doi.org/10.1016/j.drugpo.2018.10.002.
Graf N, Dichtl A, Deimel D, Sander D, Stover H. Chemsex among men who have sex with men in Germany: motives, consequences and the response of the support system. Sex Health. 2018;15(2):151–6. https://doi.org/10.1071/SH17142.
Smith V, Tasker F. Gay men’s chemsex survival stories. Sex Health. 2018;15(2):116–22. https://doi.org/10.1071/SH17122.
Emslie C, Lennox J, Ireland L. The role of alcohol in identity construction among LGBT people: a qualitative study. Sociol Health Illn. 2017;39(8):1465–79. https://doi.org/10.1111/1467-9566.12605.
Vagenas P, Brown SE, Clark JL, Konda KA, Lama JR, Sanchez J, et al. A Qualitative Assessment of Alcohol Consumption and Sexual Risk Behaviors Among Men Who Have Sex With Men and Transgender Women in Peru. Subst Use Misuse. 2017;52(7):831–9. https://doi.org/10.1080/10826084.2016.1264968.
Weatherburn P, Hickson F, Reid D, Torres-Rueda S, Bourne A. Motivations and values associated with combining sex and illicit drugs ('chemsex’) among gay men in South London: findings from a qualitative study. Sex Transm Infect. 2017;93(3):203–6. https://doi.org/10.1136/sextrans-2016-052695.
Brown SE, Vagenas P, Konda KA, Clark JL, Lama JR, Gonzales P, et al. Men Who Have Sex With Men in Peru: Acceptability of Medication-Assisted Therapy for Treating Alcohol Use Disorders. Am j. 2017;11(4):1269–78. https://doi.org/10.1177/1557988315576775.
Bochicchio LA, Drabble LA, Riggle EDB, Munroe C, Wootton AR, Hughes TL. Understanding Alcohol and Marijuana Use among Sexual Minority Women during the COVID-19 Pandemic: A Descriptive Phenomenological Study. J Homosex. 2021;68(4):631–46. https://doi.org/10.1080/00918369.2020.1868187.
Tan AS, Gazarian PK, Darwish S, Hanby E, Farnham BC, Koroma-Coker FA, et al. Smoking protective and risk factors among transgender and gender-expansive individuals (project SPRING): Qualitative study using digital photovoice. JMIR Public Health Surveill. 2021;7(10): e27417.
Matthews AK, Cesario J, Ruiz R, Ross N, King A. A qualitative study of the barriers to and facilitators of smoking cessation among lesbian, gay, bisexual, and transgender smokers who are interested in quitting. Lgbt Health. 2017;4(1):24–33.
Felner JK, Wisdom JP, Williams T, Katuska L, Haley SJ, Jun HJ, et al. Stress, Coping, and Context: Examining Substance Use Among LGBTQ Young Adults With Probable Substance Use Disorders. Psychiatr Serv. 2020;71(2):112–20. https://doi.org/10.1176/appi.ps.201900029.
Masterson JM, Zhao H, Choi E, Kim HH, Anger JT. Characteristics and Long Term Follow up of Men Who Suffer Ischemic Priapism Secondary to Recreational Use of Intracavernosal Injectable Medications. Urology. 2021;156:163–8. https://doi.org/10.1016/j.urology.2021.06.036.
Herrijgers C, Poels K, Vandebosch H, Platteau T, van Lankveld J, Florence E. Harm Reduction Practices and Needs in a Belgian Chemsex Context: Findings from a Qualitative Study. Int J Environ Res Public Health. 2020;17(23):04. https://doi.org/10.3390/ijerph17239081.
Baguso GN, Aguilar K, Sicro S, Manacop M, Quintana J, Wilson EC. “Lost trust in the system”: system barriers to publicly available mental health and substance use services for transgender women in San Francisco. BMC Health Serv Res. 2022;22(1):930. https://doi.org/10.1186/s12913-022-08315-5.
Tomkins A, Vivancos R, Ward C, Kliner M. How can those engaging in chemsex best be supported? An online survey to gain intelligence in Greater Manchester. Int J STD AIDS. 2018;29(2):128–34. https://doi.org/10.1177/0956462417719643.
Hsiang E, Jennings D, Matheson T, Hern J, Euren J, Santos GM. Acceptability of pharmacotherapy for hazardous alcohol use among men who have sex with men: Findings from a qualitative study. Addict Behav Rep. 2018;8:122–7. https://doi.org/10.1016/j.abrep.2018.09.004.
Burgess K, Parkhill G, Wiggins J, Ruth S, Stoove M. Re-Wired: treatment and peer support for men who have sex with men who use methamphetamine. Sex Health. 2018;15(2):157–9. https://doi.org/10.1071/SH17148.
Buttram ME, Kurtz SP. A Qualitative Study of African American/Black MSM’s Experiences of Participating in a Substance Use and Sexual Risk Reduction Intervention. Am j. 2017;11(4):1155–61. https://doi.org/10.1177/1557988315584157.
Jones J, Edwards OW, Merrill L, Sullivan PS, Stephenson R. Interest in HIV prevention mobile phone apps: focus group study with sexual and gender minority persons living in the rural Southern United States. JMIR Formative Research. 2022;6(6): e38075.
Holloway IW, Rice E, Gibbs J, Winetrobe H, Dunlap S, Rhoades H. Acceptability of smartphone application-based HIV prevention among young men who have sex with men. AIDS Behav. 2014;18(2):285–96.
Lunn MR, Capriotti MR, Flentje A, Bibbins-Domingo K, Pletcher MJ, Triano AJ, et al. Using mobile technology to engage sexual and gender minorities in clinical research. PLoS ONE. 2019;14(5):e0216282.
Parker JN, Hunter AS, Bauermeister JA, Bonar EE, Carrico A, Stephenson R. Comparing Social Media and In-Person Recruitment: Lessons Learned From Recruiting Substance-Using, Sexual and Gender Minority Adolescents and Young Adults for a Randomized Control Trial. JMIR Public Health Surveill. 2021;7(12):e31657.
Gustafson DH, McTavish FM, Chih M-Y, Atwood AK, Johnson RA, Boyle MG, et al. A smartphone application to support recovery from alcoholism: a randomized clinical trial. JAMA Psychiat. 2014;71(5):566–72. https://doi.org/10.1001/jamapsychiatry.2013.4642.
Suen LW, Lunn MR, Katuzny K, Finn S, Duncan L, Sevelius J, et al. What sexual and gender minority people want researchers to know about sexual orientation and gender identity questions: a qualitative study. Arch Sex Behav. 2020;49(7):2301–18.
Durham DBT, Inc. DBT Diary Card & Skills Coach. 2014. https://apps.apple.com/us/app/dbt-diary-card-skills-coach/id479013889.
Bruce Baskerville N, Wong K, Shuh A, Abramowicz A, Dash D, Esmail A, et al. A qualitative study of tobacco interventions for LGBTQ+ youth and young adults: overarching themes and key learnings. BMC Public Health. 2018;18:1–14.
Baskerville NB, Shuh A, Wong-Francq K, Dash D, Abramowicz A. LGBTQ youth and young adult perspectives on a culturally tailored group smoking cessation program. Nicotine Tob Res. 2017;19(8):960–7.
Balsam KF, Mohr JJ. Adaptation to sexual orientation stigma: a comparison of bisexual and lesbian/gay adults. J Couns Psychol. 2007;54(3):306.
Chan RC, Operario D, Mak WW. Bisexual individuals are at greater risk of poor mental health than lesbians and gay men: The mediating role of sexual identity stress at multiple levels. J Affect Disord. 2020;260:292–301.
Acknowledgements
The authors would like to thank Mary Katherine Haver, MLIS, AHIP-D, Medical Librarian, Biomedical Library, H. Lee Moffitt Cancer Center & Research Institute, for assistance with the literature search.
Funding
This work has been supported by the Cancer Center Support Grant (P30CA076292) at the H. Lee Moffitt Cancer Center & Research Institute, a comprehensive cancer center designated by the National Cancer Institute, and National Cancer Institute (K99CA271040, PI: Yang).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Informed Consent
Not applicable.
Conflicts of Interest
Matthew B. Schabath, Ph.D. is a consultant for Bristol Myers Squibb.
Human and Animal Rights
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yang, MJ., Martínez, Ú., Simmons, V.N. et al. Considerations and recommendations for mHealth interventions for substance use among Sexual and Gender Minority (SGM) individuals: A narrative review of the past 5 years. Curr Addict Rep 10, 353–365 (2023). https://doi.org/10.1007/s40429-023-00497-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40429-023-00497-0