Abstract
Purpose of Review
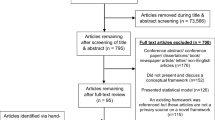
Smoking remains a leading preventable cause of premature death in the world; thus, developing effective and scalable smoking cessation interventions is crucial. This review uses the Obesity-Related Behavioral Intervention Trials (ORBIT) model for early phase development of behavioral interventions to conceptually organize the state of research of mobile applications (apps) for smoking cessation, briefly highlight their technical and theory-based components, and describe available data on efficacy and effectiveness.
Recent Findings
Our review suggests that there is a need for more programmatic efforts in the development of mobile applications for smoking cessation, though it is promising that more studies are reporting early phase research such as user-centered design. We identified and described the app features used to implement smoking cessation interventions, and found that the majority of the apps studied used a limited number of mechanisms of intervention delivery, though more effort is needed to link specific app features with clinical outcomes. Similar to earlier reviews, we found that few apps have yet been tested in large well-controlled clinical trials, although progress is being made in reporting transparency with protocol papers and clinical trial registration.
Summary
ORBIT is an effective model to summarize and guide research on smartphone apps for smoking cessation. Continued improvements in early phase research and app design should accelerate the progress of research in mobile apps for smoking cessation.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
WHO Global Report: mortality attributable to tobacco. Geneva, Switzerland: World Health Organization; 2012. Available from: https://www.who.int/tobacco/publications/surveillance/en/
Goodchild M, Nargis N, d’Espaignet ET. Global economic cost of smoking-attributable diseases. Tob Control. 2018;27(1):58–64.
National Center for Chronic Disease Prevention and Health Promotion (U.S.) Office on Smoking and Health. The health consequences of smoking—50 years of progress: a report of the Surgeon General. Atlanta GA: Centers for Disease Control and Prevention; 2014. Available from: http://www.ncbi.nlm.nih.gov/books/NBK179276/
Centers for Disease Control and Prevention. Current cigarette smoking among adults—United States, 2016. Morbidity and Mortality Weekly Report 2018;67(2):53–9 [Accessed 2018 Nov 15].
Bhattacharya A, Vilardaga R, Kientz JA, Munson SA. Lessons from practice: designing tools to facilitate individualized support for quitting smoking. ACM Trans Comput Hum Interact. 2017;2017:3057–70.
Vilardaga R, Bricker J, McDonell M. The promise of mobile technologies and single case designs for the study of individuals in their natural environment. J Contextual Behav Sci. 2014;3(2):148–53.
Shiffman S, Stone AA, Hufford M. Ecological momentary assessment. Annu Rev Clin Psychol. 2008;4:1–32.
Zeng EY, Vilardaga R, Heffner JL, Mull KE, Bricker JB. Predictors of utilization of a novel smoking cessation smartphone app. Telemed J E Health. 2015;21(12):998–1004.
Whittaker R, McRobbie H, Bullen C, Rodgers A, Gu Y. Mobile phone-based interventions for smoking cessation. Cochrane Database Syst Rev. 2016;4:CD006611.
BinDhim NF, McGeechan K, Trevena L. Who uses smoking cessation apps? A feasibility study across three countries via smartphones. J Med Internet Res mHealth uHealth 2014;2(1).
Haskins BL, Lesperance D, Gibbons P, Boudreaux ED. A systematic review of smartphone applications for smoking cessation. Transl Behav Med. 2017;7(2):292–9.
Heffner JL, Vilardaga R, Mercer LD, Kientz JA, Bricker JB. Feature-level analysis of a novel smartphone application for smoking cessation. Am J Drug Alcohol Abuse. 2015;41(1):68–73.
Bert F, Giacometti M, Gualano MR, Siliquini R. Smartphones and health promotion: a review of the evidence. J Med Syst. 2013;38(1):9995.
Ghorai K, Akter S, Khatun F, Ray P, Ghorai K, Akter S, et al. mHealth for smoking cessation programs: a systematic review. J Pers Med. 2014;4(3):412–23.
Karkar R, Zia J, Vilardaga R, Mishra SR, Fogarty J, Munson SA, et al. A framework for self-experimentation in personalized health. J Am Med Inform Assoc. 2015;23(3):440–8.
McClure JB, Hartzler AL, Catz SL. Design considerations for smoking cessation apps: feedback from nicotine dependence treatment providers and smokers. J Med Internet Res mHealth uHealth. 2016;4(1):e17. Published 2016 Feb 12.
Bricker JB, Copeland W, Mull KE, Zeng EY, Watson NL, Akioka KJ, et al. Single-arm trial of the second version of an acceptance & commitment therapy smartphone application for smoking cessation. Drug Alcohol Depend. 2017;170:37–42.
Abroms LC, Lee Westmaas J, Bontemps-Jones J, Ramani R, Mellerson J. A content analysis of popular smartphone apps for smoking cessation. Am J Prev Med. 2013;45(6):732–6.
• West R, Hajek P, Stead L, Stapleton J. Outcome criteria in smoking cessation trials: proposal for a common standard. Addict. 2005;100(3):299–303 Useful recommendations for reporting outcomes for smoking cessation.
•• Czajkowski SM, Powell LH, Adler N, et al. From ideas to efficacy: the ORBIT model for developing behavioral treatments for chronic diseases. Health Psychol. 2015;34(10):971–82 Model used to define and guide phases of research on smoking cessation apps.
Landers RN. Developing a theory of gamified learning: linking serious games and gamification of learning. Simul Gaming. 2014;45(6):752–68.
Baskerville NB, Struik LL, Dash D. Crush the crave: development and formative evaluation of a smartphone app for smoking cessation. J Med Internet Res mHealth uHealth. 2018;6(3):e52.
DeLaughter KL, Sadasivam RS, Kamberi A, English TM, Seward GL, Chan SW, et al. Crave-Out: a distraction/motivation mobile game to assist in smoking cessation. J Med Internet Res Serious Games. 2016;4(1):e3.
Gordon JS, Armin JS, Cunningham JK, Muramoto ML, Christiansen SM, Jacobs TA. Lessons learned in the development and evaluation of RxCoach™, an mHealth app to increase tobacco cessation medication adherence. Patient Educ Couns. 2017;100(4):720–7.
Armin J, Johnson T, Hingle M, Jr PG, Gordon JS. Development of a multi-behavioral mhealth app for women smokers. J Health Commun. 2017;22(2):153–62.
Tombor I, Shahab L, Brown J, Crane D, Michie S, West R. Development of SmokeFree Baby: a smoking cessation smartphone app for pregnant smokers. Transl Behav Med. 2016;6(4):533–45.
Ploderer B, Smith W, Pearce J, Borland R. A mobile app offering distractions and tips to cope with cigarette craving: a qualitative study. J Med Internet Res mHealth uHealth. 2014;2(2):e23.
Raiff BR, Fortugno N, Scherlis DR, Rapoza D. A mobile game to support smoking cessation: prototype assessment. J Med Internet Res Serious Games. 2018;6(2):e11.
Dotson JAW, Pineda R, Cylkowski H, Amiri S. Development and evaluation of an iPad application to promote knowledge of tobacco use and cessation by pregnant women. Nurs Womens Health. 2017;21(3):174–85.
van Agteren JEM, Lawn S, Bonevski B, Smith BJ. Kick.it: the development of an evidence-based smoking cessation smartphone app. Transl Behav Med. 2018;8(2):243–67.
• Vilardaga R, Rizo J, Zeng E, Kientz JA, Ries R, Otis C, et al. User-centered design of Learn to Quit, a smoking cessation smartphone app for people with serious mental illness. J Med Internet Res Serious Games. 2018;6(1):e2 Example of phase Ia study (ORBIT model) to define the design characteristics of a smoking cessation app using user-centered design methodology.
Schick RS, Kelsey TW, Marston J, Samson K, Humphris GW. MapMySmoke: feasibility of a new quit cigarette smoking mobile phone application using integrated geo-positioning technology, and motivational messaging within a primary care setting. Pilot Feasibility Stud. 2017;4(1):19.
Cerrada CJ, Dzubur E, Blackman KCA, Mays V, Shoptaw S, Huh J. Development of a just-in-time adaptive intervention for smoking cessation among Korean American emerging adults. Int J Behav Med. 2017;24(5):665–72.
Naughton F, Hopewell S, Lathia N, Schalbroeck R, Brown C, Mascolo C, et al. A context-sensing mobile phone app (Q sense) for smoking cessation: a mixed-methods study. J Med Internet Res mHealth uHealth. 2016;4(3):e106.
Tudor-Sfetea C, Rabee R, Najim M, Amin N, Chadha M, Jain M, et al. Evaluation of two mobile health apps in the context of smoking cessation: qualitative study of cognitive behavioral therapy (CBT) versus non-CBT-based digital solutions. J Med Internet Res mHealth uHealth. 2018;6(4):e98.
Bindoff I, de Salas K, Peterson G, Ling T, Lewis I, Wells L, et al. Quittr: the design of a video game to support smoking cessation. J Med Internet Res Serious Games. 2016;4(2):e19.
Hoeppner BB, Hoeppner SS, Kelly L, Schick M, Kelly JF. Smiling instead of smoking: development of a positive psychology smoking cessation smartphone app for non-daily smokers. Int J Behav Med. 2017;24(5):683–93.
Fulton E, Brown K, Kwah K, Wild S, Fulton EA, Brown KE, et al. StopApp: using the behaviour change wheel to develop an app to increase uptake and attendance at NHS stop smoking services. Healthcare. 2016;4(2):31.
Ubhi HK, Michie S, Kotz D, Wong WC, West R. A mobile app to aid smoking cessation: preliminary evaluation of SmokeFree28. J Med Internet Res. 2015;17(1):e17.
• Brinker TJ, Holzapfel J, Baudson TG, Sies K, Jakob L, Baumert HM, et al. Photoaging smartphone app promoting poster campaign to reduce smoking prevalence in secondary schools: the Smokerface randomized trial: design and baseline characteristics. BMJ Open. 2016;6(11):e014288 Interesting approach to cost-effective dissemination of an anti-smoking app for adolescents via a poster campaign.
Iacoviello BM, Steinerman JR, Klein DB, Silver TL, Berger AG, Luo SX, et al. Clickotine, a personalized smartphone app for smoking cessation: initial evaluation. J Med Internet Res mHealth uHealth. 2017;5(4):e56.
Finkelstein J, Cha EM. Using a mobile app to promote smoking cessation in hospitalized patients. J Med Internet Res mHealth uHealth. 2016;4(2):e59.
Bruno M, Wright M, Baker CL, Emir B, Carda E, Clausen M, et al. Mobile app usage patterns of patients prescribed a smoking cessation medicine: prospective observational study. J Med Internet Res mHealth uHealth. 2018;6(4):e97.
Shuter J, Kim RS, An LC, Abroms LC. Feasibility of a smartphone-based tobacco treatment for HIV-infected smokers. Nicotine Tob Res. 2018. https://doi.org/10.1093/ntr/nty208.
Buller DB, Borland R, Bettinghaus EP, Shane JH, Zimmerman DE. Randomized trial of a smartphone mobile application compared to text messaging to support smoking cessation. Telemed J E Health. 2014;20(3):206–14.
Bricker JB, Mull KE, Kientz JA, Vilardaga R, Mercer LD, Akioka KJ, et al. Randomized, controlled pilot trial of a smartphone app for smoking cessation using acceptance and commitment therapy. Drug Alcohol Depend. 2014;143:87–94.
Businelle MS, Ma P, Kendzor DE, Frank SG, Vidrine DJ, Wetter DW. An ecological momentary intervention for smoking cessation: evaluation of feasibility and effectiveness. J Med Internet Res. 2016;18(12):e321.
• Dar R. Effect of real-time monitoring and notification of smoking episodes on smoking reduction: a pilot study of a novel smoking cessation app. Nicotine Tob Res. 2017;20(12):1515–8 Promising new approach utilizing mobile wearable technology (smartbands) to monitor and intervene with smoking.
Brinker TJ, Brieske CM, Esser S, Klode J, Mons U, Batra A, et al. A face-aging app for smoking cessation in a waiting room setting: pilot study in an HIV outpatient clinic. J Med Internet Res. 2018;20(8):e10976.
Hicks TABS, Thomas SP, Wilson SM, Calhoun PS, Kuhn ER, Beckham JC. A preliminary investigation of a relapse prevention mobile application to maintain smoking abstinence among individuals with posttraumatic stress disorder. J Dual Diagn. 2017;13(1):15–20.
Pifarré M, Carrera A, Vilaplana J, Cuadrado J, Solsona S, Abella F, et al. TControl: a mobile app to follow up tobacco-quitting patients. Comput Methods Prog Biomed. 2017;142:81–9.
• Garrison KA, Pal P, O'Malley SS, Pittman BP, Gueorguieva R, Rojiani R, et al. Craving to quit: a randomized controlled trial of smartphone app-based mindfulness training for smoking cessation. Nicotine Tob Res. 2018. https://doi.org/10.1093/ntr/nty126 One author’s full-scale randomized controlled trial of smartphone app-based mindfulness training for smoking cessation.
Cambon L, Bergman P, Faou AL, Vincent I, Maitre BL, Pasquereau A, et al. Study protocol for a pragmatic randomized controlled trial evaluating efficacy of a smoking cessation e-‘Tabac info service’: ee-TIS trial. BMJ Open. 2017;7(2):e013604.
BinDhim NF, McGeechan K, Trevena L. Smartphone smoking cessation application (SSC App) trial: a multicountry double-blind automated randomized controlled trial of a smoking cessation decision-aid ‘app’. BMJ Open. 2018;8(1):e017105.
• Tobacco Use and Dependence Guideline Panel. Treating tobacco use and dependence: 2008 update. Rockville MD: U.S. Department of Health and Human Services; 2008 May. Available from: https://www.ncbi.nlm.nih.gov/books/NBK63952/. Evidence-based guidelines for treating tobacco use and dependence.
Fulton E, Kwah K, Wild S, Brown K, Fulton EA, Kwah KL, et al. Lost in translation: transforming behaviour change techniques into engaging digital content and design for the StopApp. Healthcare. 2018;6(3):75.
Skinner AL, Stone CJ, Doughty H, Munafò MR. StopWatch: the preliminary evaluation of a smartwatch-based system for passive detection of cigarette smoking. Nicotine Tob Res. 2018;21:257–61.
Crane D, Ubhi HK, Brown J, West R. Relative effectiveness of a full versus reduced version of the ‘Smoke Free’ mobile application for smoking cessation: a randomized controlled trial. F1000Research. 2018;7:1524.
Lin Y, Tudor-Sfetea C, Siddiqui S, Sherwani Y, Ahmed M, Eisingerich AB. Effective behavioral changes through a digital mHealth app: exploring the impact of hedonic well-being, psychological empowerment and inspiration. J Med Internet Res mHealth uHealth. 2018;6(6):e10024.
• Garrison KA, Pal P, Rojiani R, Dallery J, O’Malley SS, Brewer JA. A randomized controlled trial of smartphone-based mindfulness training for smoking cessation: a study protocol. BMC Psychiatry. 2015;15(1):83 Example “protocol paper” recommended to reduce reporting bias and increase transparency in reporting clinical trials of smartphone apps for smoking cessation.
Giacobbi P Jr, Hingle M, Johnson T, Cunningham JK, Armin J, Gordon JS. See me smoke-free: protocol for a research study to develop and test the feasibility of an mHealth app for women to address smoking, diet, and physical activity. JMIR Res Protoc. 2016;5(1):e12.
Gordon JS, Armin J, Hingle MD, Giacobbi P, Cunningham JK, Johnson T, et al. Development and evaluation of the see me smoke-free multi-behavioral mHealth app for women smokers. Transl Behav Med. 2017;7(2):172–84.
Tombor I, Beard E, Brown J, Shahab L, Michie S, West R. Randomized factorial experiment of components of the SmokeFree Baby smartphone application to aid smoking cessation in pregnancy. Transl Behav Med. 2018. https://doi.org/10.1093/tbm/iby073.
Brinker TJ, Seeger W, Buslaff F. Photoaging mobile apps in school-based tobacco prevention: the mirroring approach. J Med Internet Res. 2016;18(6):e183.
Pew Research Center, February, 2016, Smartphone ownership and internet usage continues to climb in emerging economies. http://www.pewglobal.org/2016/02/22/smartphone-ownership-and-internet-usage-continues-to-climb-in-emerging-economies/ [Accessed 15 Nov 2018].
Center for Behavioral Health Statistics and Quality. (2017). 2016 National Survey on drug use and health: detailed tables. Substance Abuse and Mental Health Services Administration, Rockville, MD.
Baskerville NB, Struik LL, Hammond D, Guindon GE, Norman CD, Whittaker R, et al. Effect of a mobile phone intervention on quitting smoking in a young adult population of smokers: randomized controlled trial study protocol. JMIR Res Protoc. 2015;4(1):e10.
Baskerville NB, Struik LL, Guindon GE, Norman CD, Whittaker R, Burns C, et al. Effect of a mobile phone intervention on quitting smoking in a young adult population of smokers: randomized controlled trial. J Med Internet Res mHealth uHealth. 2018;6(10):e10893.
Struik LL, Bottorff JL, Baskerville NB, Oliffe JL. The Crush the Crave quit smoking app and young adult smokers: qualitative case study of affordances. J Med Internet Res mHealth uHealth. 2018;6(6):e134.
Vilardaga R, Rizo J, Kientz JA, McDonell MG, Ries RK, Sobel K. User experience evaluation of a smoking cessation app in people with serious mental illness. Nicotine Tob Res. 2016;18(5):1032–8.
• Vilardaga R, Rizo J, Zeng E, et al. User-centered design of Learn to Quit, a smoking cessation smartphone app for people with serious mental illness. J Med Internet Res Serious Games. 2018;6(1):e2. Example of phase Ib study (ORBIT model) to refine the design characteristics of a smoking cessation app using cost-effective single case design methodology.
Lawn S, van Agteren J, Zabeen S, Bertossa S, Barton C, Stewart J, et al. Adapting, pilot testing and evaluating the Kick.it app to support smoking cessation for smokers with severe mental illness: a study protocol. Int J Environ Res Public Health. 2018;15(2):254.
Herbst E, Pennington D, Kuhn E, McCaslin SE, Delucchi K, Batki SL, et al. Mobile technology for treatment augmentation in veteran smokers with posttraumatic stress disorder. Am J Prev Med. 2018;54(1):124–8.
Rigotti NA, Munafo MR, Stead LF. Smoking cessation interventions for hospitalized smokers: a systematic review. Arch Intern Med. 2008;168(18):1950–60.
Mdodo R, Frazier EL, Dube SR, Mattson CL, Sutton MY, Brooks JT, et al. Cigarette smoking prevalence among adults with HIV compared with the general adult population in the United States: cross-sectional surveys. Ann Intern Med. 2015;162(5):335–44.
Hiscock R, Bauld L, Amos A, Fidler JA, Munafò M. Socioeconomic status and smoking: a review. Ann N Y Acad Sci. 2012;1248(1):107–23.
Hébert ET, Stevens EM, Frank SG, Kendzor DE, Wetter DW, Zvolensky MJ, et al. An ecological momentary intervention for smoking cessation: the associations of just-in-time, tailored messages with lapse risk factors. Addict Behav. 2018;78:30–5.
Collins LM, Murphy SA, Strecher V. The multiphase optimization strategy (MOST) and the sequential multiple assignment randomized trial (SMART): new methods for more potent eHealth interventions. Am J Prev Med. 2007;32(5 Suppl):S112–8.
Moher D, Hopewell S, Schulz KF, Montori V, Gøtzsche PC, Devereaux PJ, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomized trials. BMJ. 2010;340:c869.
Borrelli B. The assessment, monitoring, and enhancement of treatment fidelity in public health clinical trials. J Public Health Dent. 2011;71(s1):S52–63.
Bowen DJ, Kreuter M, Spring B, Cofta-Woerpel L, Linnan L, Weiner D, et al. How we design feasibility studies. Am J Prev Med. 2009;36(5):452–7.
Kraemer HC, Mintz J, Noda A, Tinklenberg J, Yesavage JA. Caution regarding the use of pilot studies to guide power calculations for study proposals. Arch Gen Psychiatry. 2006;63(5):484–9.
Munafò MR, Nosek BA, Bishop DVM, Button KS, Chambers CD, Percie du Sert N, et al. A manifesto for reproducible science. Nat Hum Behav. 2017;1(1):0021.
Vilardaga R, Hayes SC, Levin ME, Muto T. Creating a strategy for progress: a contextual behavioral science approach. Behav Anal. 2009;32(1):105–33.
Thornton L, Quinn C, Birrell L, Guillaumier A, Shaw B, Forbes E, et al. Free smoking cessation mobile apps available in Australia: a quality review and content analysis. Aust N Z J Public Health. 2017;41(6):625–30.
Kumar S, Nilsen WJ, Abernethy A, Atienza A, Patrick K, Pavel M, et al. Mobile health technology evaluation: the mHealth evidence workshop. Am J Prev Med. 2013;45(2):228–36.
Riley WT, Rivera DE, Atienza AA, Nilsen W, Allison SM, Mermelstein R. Health behavior models in the age of mobile interventions: are our theories up to the task? Transl Behav Med. 2011;1(1):53–71.
Brewer JA, Mallik S, Babuscio TA, Nich C, Johnson HE, Deleone CM, et al. Mindfulness training for smoking cessation: results from a randomized controlled trial. Drug Alcohol Depend. 2011;119(1–2):72–80.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
J.F.M. reports and ownership of a company that provided smoking cessation–related scientific consulting and market research to GSK—Consumer Healthcare.
R.V. reports grants from National Institutes on Drug Abuse, during the conduct of the study.
K.A.G. and E.C.-P. have nothing to disclose.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Tobacco
Rights and permissions
About this article
Cite this article
Vilardaga, R., Casellas-Pujol, E., McClernon, J.F. et al. Mobile Applications for the Treatment of Tobacco Use and Dependence. Curr Addict Rep 6, 86–97 (2019). https://doi.org/10.1007/s40429-019-00248-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40429-019-00248-0