Abstract
Purpose of Review
This paper integrates recent developments in the areas of excessive eating and addictive behavior, reviewing shared and unique features with respect to topography, etiological mechanisms/risk factors, comorbidity, and related adverse consequences/correlates.
Recent Findings
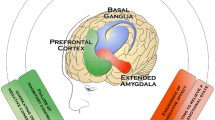
Emerging literature is converging to suggest a high degree of overlap in terms of eating and addictive behavior, including common risk factors and involvement of brain reward pathways. Behavioral phenotypes involving putative addictive elements include binge eating, food addiction, nocturnal eating, grazing, and emotional eating. Emerging evidence supports that dysregulation of brain reward pathways may underlie certain forms of obesity, particularly when driven by compulsive eating behavior or binge eating disorder/food addiction, and the evidence for comparable dysregulation underlying substance use disorders (SUD) and other addictive behavior is quite robust, with a high degree of overlap in brain circuitry driving excessive eating and drug addiction. At least one form of weight loss (bariatric) surgery, Roux-en-Y gastric bypass, is associated with post-surgical SUD onset, and this body of work has greatly expanded our appreciation of the intricate gut-brain connections involved in eating and addictive behavior. Nonetheless, controversy remains regarding the extent to which and in what forms eating behavior may constitute addiction.
Summary
Research productivity in the intersection of eating, obesity, and addiction has increased dramatically over the past decade, particularly within the past 5 years; it is expected that our understanding of these relationships will grow substantially in the coming years, particularly in light of recent advances in our understanding of the nuances of gut-brain communication that may shed light on new mechanisms.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Wilson GT. The addiction model of eating disorders: a critical analysis. Adv Behav Res Ther. 1991;13:27–72.
Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in obesity among adults in the United States, 2005 to 2014. JAMA. 2016;315(21):2284–91.
KuczmarskiRJ FKM, Campbell SMJC. Increasing prevalence of overweight among US adults: the National Health and Nutrition Examination Surveys, 1960 to 1991. JAMA. 1994;272(3):205–11.
Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA. 2012;307(5):491–7.
Sassi F, Devaux M, Cecchini M, Rusticelli E. OECD health working papers no. 45 the obesity epidemic: analysis of past and projected future trends in selected OECD countries. OECD Health Working Papers. Paris; 2009. Report No. 54.
Sturm R, Hattori A. Morbid obesity rates continue to rise rapidly in the United States. Int J Obes. 2013;37(6):889–91.
Hasin DS, Grant BF. The National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) waves 1 and 2: review and summary of findings. Soc Psychiatry Psychiatr Epidemiol. 2015;50(11):1609–40.
Grant BF, Goldstein, RB, Saha, TD, Chou, SP, Jung, J, Zhang, H, et al. Epidemiology of DSM-5 alcohol use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015;72(8):757–66.
Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML, et al. The global obesity pandemic: shaped by global drivers and local environments. Lancet. 2011;378(9793):804–14.
Briefel RR, Johnson CL. Secular trends in dietary intake in the United States. Annu Rev Nutr. 2004;24:401–31.
Davis C. From passive overeating to “food addiction”: a spectrum of compulsion and severity. ISRN Obes. 2013;2013:1–20.
Blomain ES, Dirhan DA, Valentino MA, Kim GW, Waldman SA. Mechanisms of weight regain following weight loss. ISRN Obes. 2013;2013:210524.
Striegel-Moore RH, Rosselli F, Wilson GT, Perrin N, Harvey K, DeBar L. Nocturnal eating: association with binge eating, obesity, and psychological distress. Int J Eat Disord. 2010;43(6):520–6.
Mitchell JE, King WC, Courcoulas A, Dakin G, Elder K, Engel S, et al. Eating behavior and eating disorders in adults before bariatric surgery. Int J Eat Disord. 2015;48(2):215–22.
Chao AM, Shaw JA, Pearl RL, Alamuddin N, Hopkins CM, Bakizada ZM, et al. Prevalence and psychosocial correlates of food addiction in persons with obesity seeking weight reduction. Compr Psychiatry. 2017;73:97–104.
Nolan LJ. Is it time to consider the “food use disorder?”. Appetite. 2017;115:16–8.
De Ridder D, Manning P, Leong SL, Ross S, Sutherland W, Horwath C, et al. The brain, obesity and addiction: an EEG neuroimaging study. Sci Rep. 2016;6(1):34122.
Nolan LJ, Geliebter A. “food addiction” is associated with night eating severity. Appetite. 2016;98:89–94.
Nolan LJ, Geliebter A. Validation of the Night Eating Diagnostic Questionnaire (NEDQ) and its relationship with depression, sleep quality, “food addiction”, and body mass index. Appetite. 2017;111:86–95.
• Gearhardt AN, Corbin WR, Brownell KD. Development of the yale food addiction scale version 2.0. Psychol Addict Behav. 2016;30(1):113–21. This paper presents the new version of the YFAS, which aligns with DSM-5 symptomology.
Stunkard AJ. The night-eating syndrome: a pattern of food intake among certain obese patients. Am J Med. 1955;19(1):78–86.
Stunkard AJ. Eating patterns and obesity. Psychiatr Q. 1959;33(2):284–95.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5). 5th ed. Arlington: American Psychiatric Publishing, 2013.
Kessler RC, Berglund PA, Chiu WT, Deitz AC, Hudson JI, Shahly V, et al. The prevalence and correlates of binge eating disorder in the World Health Organization world mental health surveys. Biol Psychiatry. 2013;73(9):904–14.
Latner JD, Mond JM, Kelly MC, Haynes SN, Hay PJ. The loss of control over eating scale: development and psychometric evaluation. Int J Eat Disord. 2014;47(6):647–59.
Smith DG, Robbins TW. The neurobiological underpinnings of obesity and binge eating: a rationale for adopting the food addiction model. Biol Psychiatry. 2013;73(9):804–10.
Ferrer-Garcia M, Pla-Sanjuanelo J, Dakanalis A, Vilalta-Abella F, Riva G, Fernandez-Aranda F, et al. Eating behavior style predicts craving and anxiety experienced in food-related virtual environments by patients with eating disorders and healthy controls. Appetite. 2017;117:284–93.
Meule A. Back by popular demand: a narrative review on the history of food addiction research. Yale J Biol Med. 2015;88(3):295–302.
Brunault P, Courtois R, Gearhardt AN, Gaillard P, Journiac K, Cathelain S, et al. Validation of the French version of the DSM-5 Yale Food Addiction Scale in a nonclinical sample. Can J Psychiatr. 2017;62(3):199–210.
Pedram P, Wadden D, Amini P, Gulliver W, Randell E, Cahill F, et al. Food addiction: its prevalence and significant association with obesity in the general population. PLoS One. 2013;8(9):e74832.
Markus CR, Rogers PJ, Brouns F, Schepers R. Eating dependence and weight gain; no human evidence for a “sugar-addiction” model of overweight. Appetite. 2017;114:64–72.
Hebebrand J, Albayrak Ö, Adan R, Antel J, Dieguez C, De Jong J, et al. “Eating addiction”, rather than “food addiction”, better captures addictive-like eating behavior. Neurosci Biobehav Rev. 2014;47:295–306.
Ruddock HK, Christiansen P, Halford JCG, Hardman CA. The development and validation of the Addiction-like Eating Behaviour Scale. Int J Obes. 2017;41(11):1710–17.
• Schulte EM, Potenza MN, Gearhardt AN. A commentary on the “eating addiction” versus “food addiction” perspectives on addictive-like food consumption. Appetite. 2017;115:9–15. This paper considers whether food addiction is better understood as a behavioral addiction or as a substance use disorder, where foods with specific macro nutriet profiles represent a potenitally addictive substance for vulnerable individuals.
Schulte EM, Avena NM, Gearhardt AN. Which foods may be addictive? The roles of processing, fat content, and glycemic load. PLoS One. 2015;10(2):1–18.
Gearhardt AN, Corbin WR, Brownell KD. Preliminary validation of the Yale Food Addiction Scale. Appetite. 2009;52(2):430–6.
Schulte EM, Gearhardt AN. Development of the Modified Yale Food Addiction Scale Version 2.0. Eur Eat Disord Rev. 2017;25(4):302–8.
Allison KC, Lundgren JD, O’Reardon JP, Martino NS, Sarwer DB, Wadden TA, et al. The Night Eating Questionnaire (NEQ): psychometric properties of a measure of severity of the night eating syndrome. Eat Behav. 2008;9(1):62–72.
Meule A, Allison KC, Platte P. Emotional eating moderates the relationship of night eating with binge eating and body mass. Eur Eat Disord Rev. 2014;22(2):147–51.
Meule A, Allison KC, Brähler E, de Zwaan M. The association between night eating and body mass depends on age. Eat Behav. 2014;15(4):683–5.
Branstetter SA, Horton WJ, Mercincavage M, Buxton OM. Severity of nicotine addiction and disruptions in sleep mediated by early awakenings. Nicotine Tob Res. 2016;18(12):2252–9.
Baker TB, Piper ME, McCarthy DE, Bolt DM, Smith SS, Kim S-Y, et al. Time to first cigarette in the morning as an index of ability to quit smoking: implications for nicotine dependence. Nicotine Tob Res. 2007;9(Suppl 4):S555–70.
Conceição EM, Mitchell JE, Engel SG, Machado PPP, Lancaster K, Wonderlich SA. What is “grazing”? Reviewing its definition, frequency, clinical characteristics, and impact on bariatric surgery outcomes, and proposing a standardized definition. Surg Obes Relat Dis. 2014;10(5):973–82.
•• Davis C. A commentary on the associations among “food addiction”, binge eating disorder, and obesity: overlapping conditions with idiosyncratic clinical features. Appetite. 2017;115:3–8. A very comprehensive recent paper on the nuances of food addiction, binge eating, and weight.
Burgmer R, Grigutsch K, Zipfel S, Wolf AM, de Zwaan M, Husemann B, et al. The influence of eating behavior and eating pathology on weight loss after gastric restriction operations. Obes Surg. 2005;15(5):684–91.
Saunders R. “Grazing”: a high-risk behavior. Obes Surg. 2004;14(1):98–102.
Leite Faria S, De Oliveira Kelly E, Pereira Faria O, Kiyomi Ito M. Snack-eating patients experience lesser weight loss after roux-en-Y gastric bypass surgery. Obes Surg. 2009;19(9):1293–6.
Root TL, Pisetsky EM, Thornton L, Lichtenstein P, Pedersen NL, Bulik CM. Patterns of co-morbidity of eating disorders and substance use in Swedish females. Psychol Med. 2010;40(1):105–15.
Hudson JI, Hiripi E, Pope HG, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;61(3):348–58.
Munn-Chernoff MA, Grant JD, Bucholz KK, Agrawal A, Lynskey MT, Madden PAF, et al. Bulimic behaviors and early substance use: findings from a cotwin-control study. Alcohol Clin Exp Res. 2015;33(4):395–401.
Fouladi F, Mitchell JE, Crosby RD, Engel SG, Crow S, Hill L, et al. Prevalence of alcohol and other substance use in patients with eating disorders. Eur Eat Disord Rev. 2015;23(6):531–6.
Becker DF, Grilo CM. Comorbidity of mood and substance use disorders in patients with binge-eating disorder: associations with personality disorder and eating disorder pathology. J Psychosom Res. 2015;79(2):159–64.
Saules KK, Tate JC, Pomerleau CS. Weight control smoking in women. In: Tolson KP, Veksler EB, editors. Research Focus on Smoking and Women’s Health Research. Hauppauge: Nova Science Publishers, Inc.; 2008. p. 59–90.
Mies GW, Treur JL, Larsen JK, Halberstadt J, Pasman JA, Vink JM. The prevalence of food addiction in a large sample of adolescents and its association with addictive substances. Appetite. 2017;118:97–105.
Chuang CWI, Sussman S, Stone MD, Pang RD, Chou CP, Leventhal AM, et al. Impulsivity and history of behavioral addictions are associated with drug use in adolescents. Addict Behav. 2017;74(March):41–7.
Hunt TK, Forbush KT. Is “drunkorexia” an eating disorder, substance use disorder, or both? Eat Behav. 2016;22:40–5.
• Lu H, Mannan H, Hay P. Exploring relationships between recurrent binge eating and illicit substance use in a non-clinical sample of women over two years. Behav Sci (Basel). 2017;7(3):E46. This represents a strong contribution to the literature because it is transdiagnostic and longitudinal. The researchers find evidence to support comorbidity and subsitution patterns, where indviduals initiate binge eating following cessation of illicit substance use.
Petry NM, Barry D, Pietrzak RH, Wagner JA. Overweight and obesity are associated with psychiatric disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychosom Med. 2008;70(3):288–97.
Grucza RA, Krueger RF, Racette SB, Norberg, KE, Hipp PR, Beirut, L. The emerging link between alcoholism risk and obesity in the United States. Arch Gen Psychiatry. 2010;67(12):1301–8.
Huang DYC, Lanza HI, Anglin MD. Association between adolescent substance use and obesity in young adulthood: a group-based dual trajectory analysis. Addict Behav. 2013;38(11):2353–660.
Plurphanswat N, Rodu B. The association of smoking and demographic characteristics on body mass index and obesity among adults in the U.S., 1999–2012. BMC Obes. 2014;1(1):18.
Dare S, Mackay DF, Pell JP. Relationship between smoking and obesity: a cross-sectional study of 499,504 middle-aged adults in the UK general population. PLoS One. 2015;10(4):1–12.
Mackay DF, Gray L, Pell JP. Impact of smoking and smoking cessation on overweight and obesity: Scotland-wide, cross-sectional study on 40,036 participants. BMC Public Health. 2013;13:348.
Chatkin R, Mottin CC, Chatkin JM. Smoking among morbidly obese patients. BMC Pulm Med BioMed Central Ltd. 2010;10(1):61.
Cowan J, Devine C. Food, eating, and weight concerns of men in recovery from substance addiction. Appetite. 2008;50(1):33–42.
Han DH, Bolo N, Daniels MA, Lyoo IK, Min KJ, Kim CH, et al. Craving for alcohol and food during treatment for alcohol dependence: modulation by T allele of 1519T>C GABA A α6. Alcohol Clin Exp Res. 2008;32(9):1593–9.
Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders. Arch Gen Psychiatry. 2004;61(8):807–16.
Scott KM, McGee MA, Wells JE, Oakley Browne MA. Obesity and mental disorders in the adult general population. J Psychosom Res. 2008;64(1):97–105.
Simon GE, Von Korff M, Saunders K, Miglioretti DL, Crane PK, van Belle G, et al. Association between obesity and psychiatric disorders in the US adult population. Arch Gen Psychiatry. 2006;63(7):824–30.
Mather AA, Cox BJ, Enns MW, Sareen J. Associations of obesity with psychiatric disorders and suicidal behaviors in a nationally representative sample. J Psychosom Res. 2009;66(4):277–85.
Lee SS, Humphreys KL, Flory K, Liu R, Glass K. Prospective association of childhood attention-deficit/hyperactivity disorder (ADHD) and substance use and abuse/dependence: a meta-analytic review. Clin Psychol Rev. 2011;31(3):328–41.
Davis C. Attention-deficit/hyperactivity disorder: associations with overeating and obesity. Curr Psychiatry Rep. 2010;12(5):389–95.
Pagoto SL, Curtin C, Lemon SC, Bandini LG, Schneider KL, Bodenlos JS, et al. Association between adult attention deficit/hyperactivity disorder and obesity in the US population. Obesity. 2009;17(3):539–44.
Cortese S, Moreira-Maia CR, St Fleur D, Morcillo-Peñalver C, Rohde LA, Faraone SV. Association between ADHD and obesity: a systematic review and meta-analysis. Am J Psychiatry. 2016;173(1):34–43.
Fayyad J, De Graaf R, Kessler R, Alonso J, Angermeyer M, Demyttenaere K, et al. Cross-national prevalence and correlates of adult attention-deficit hyperactivity disorder. Br J Psychiatry. 2007;190(5):402–9.
Gariepy G, Nitka D, Schmitz N. The association between obesity and anxiety disorders in the population: a systematic review and meta-analysis. Int J Obes. 2010;34(3):407–19.
Grilo CM, White MA, Masheb RM. DSM-IV psychiatric disorder comorbidity and its correlates in binge eating disorder. Int J Eat Disord. 2009;42(3):228–34.
Wilens TE, Martleton M, Joshi G, Bateman C, Fried R, Petty CR, et al. Does ADHD predict substance use disorders? A 10-year follow-up study of young adults with ADHD. J Am Acad Child Adolesc Psychiatry. 2011;50(6):1–18.
Groß-Lesch S, Dempfle A, Reichert S, Jans T, Geissler J, Kittel-Schneider S, et al. Sex- and subtype-related differences in the comorbidity of adult ADHDs. J Atten Disord. 2013;20(10): 855–66.
Black DW, Shaw M, McCormick B, Allen J. Pathological gambling: relationship to obesity, self-reported chronic medical conditions, poor lifestyle choices, and impaired quality of life. Compr Psychiatry. 2013;54(2):97–104.
Fernández-Aranda F, Jiménez-Murcia S, Álvarez-Moya EM, Granero R, Vallejo J, Bulik CM. Impulse control disorders in eating disorders: clinical and therapeutic implications. Compr Psychiatry. 2006;47(6):482–8.
Jiménez-Murcia S, Steiger H, Isräel M, Granero R, Prat R, Santamaría JJ, et al. Pathological gambling in eating disorders: prevalence and clinical implications. Compr Psychiatry. 2013;54(7):1053–60.
Lorains FK, Cowlishaw S, Thomas SA. Prevalence of comorbid disorders in problem and pathological gambling: systematic review and meta-analysis of population surveys. Addiction. 2011;106(3):490–8.
•• Ivezaj V, Stoeckel L, Avena N, Benoit SC, Conason A, Davis JF, et al. Obesity and addiction: can a complication of surgery help us understand the connection ? Obes Rev. 2017;18(7):765–75. This article highlights a unique lens for understanding the connection between obesity and SUD by reviewing specific weight-loss surgery outcomes, such as weight regain or new onset SUD. There is a focus on future directions.
Ostlund MP, Backman O, Marsk R, Stockeld D, Lagergren J, Rasmussen F, et al. Increased admission for alcohol dependence after gastric bypass surgery compared with restrictive bariatric surgery. JAMA Surg. 2013;148(4):374–7.
Saules KK, Wiedemann AW, Ivezaj VI, Hopper JA, Foster-Hartsfield J, Schwarz D. Bariatric surgery history among substance abuse treament patients: prevalence and asssociated features. Surg Obes Relat Dis. 2010;6y:615–21.
Wiedemann AA, Saules KK, Ivezaj V. Emergence of new onset substance use disorders among post-weight loss surgery patients. Clin Obes. 2013;3(6):194–201.
Ivezaj V, Saules KK, Schuh LM. New-onset substance use disorder after gastric bypass surgery: rates and associated characteristics. Obes Surg. 2014;24(11):1975–80.
Wee CC, Mukamal KJ, Huskey KW, Davis RB, Colten ME, Bolcic-Jankovic D, et al. High-risk alcohol use after weight loss surgery. Surg Obes Relat Dis. 2014;10(3):508–13.
Polston JE, Pritchett CE, Tomasko JM, Rogers AM, Leggio L, Thanos PK, et al. Roux-en-Y gastric bypass increases intravenous ethanol self-administration in dietary obese rats. PLoS One. 2013;8(12):e83741.
•• Sirohi S, Richardson BD, Lugo JM, Rossi DJ, Davis JF. Impact of Roux-en-Y gastric bypass surgery on appetite, alcohol intake behaviors, and midbrain ghrelin signaling in the rat. Obesity. 2017;25(7):1228–36. Important preclinical work that advances our understanding of gut-brain communication involved in post-RYGB SUD.
Danese A, Tan M. Childhood maltreatment and obesity: systematic review and meta-analysis. Mol Psychiatry. 2014;19(5):544–54.
Hemmingsson E, Johansson K, Reynisdottir S. Effects of childhood abuse on adult obesity: a systematic review and meta-analysis. Obes Rev. 2014;15(11):882–93.
• Edalati H, Krank MD. Childhood maltreatment and development of substance use disorders: a review and a model of cognitive pathways. Trauma Violence Abuse. 2016;17(5):454–67. This article integrates findings related to psychosocial risk (i.e., trauma) and neuropsychological risk (e.g., impaired decision making) for substance use disorder.
Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield C, Perry BD, et al. The enduring effects of abuse and related adverse experiences in childhood. Eur Arch Psychiatry Clin Neurosci. 2006;256(3):174–86.
Puetz VB, McCrory E. Exploring the relationship between childhood maltreatment and addiction: a review of the neurocognitive evidence. Curr Addict Rep. 2015;2(4):318–25.
Brown S, Mitchell TB, Fite PJ, Bortolato M. Impulsivity as a moderator of the associations between child maltreatment types and body mass index. Child Abuse Negl. 2017;67:137–46.
Holderness CC, Brooks-Gunn J, Warren MP. Co-morbidity of eating disorders and substance abuse review of the literature. Int J Eat Disord. 1994;16(1):1–34.
Kaye WH, Lilenfeld LR, Plotnicov K, Merikangas KR, Nagy L, Strober M, et al. Bulimia nervosa and substance dependence: association and family transmission. Alcohol Clin Exp Res. 1996;20(5):878–81.
Lilenfeld LRR, Ringham R, Kalarchian MA, Marcus MD. A family history study of binge-eating disorder. Compr Psychiatry. 2008;49(3):247–54.
Lee YH, Abbott DW, Seim H, Crosby RD, Monson N, Burgard M, et al. Eating disorders and psychiatric disorders in the first-degree relatives of obese probands with binge eating disorder and obese non-binge eating disorder controls. Int J Eat Disord. 1999;26(3):322–32.
Munn-chernoff MA, Duncan AE, Grant JD, Wade TD, Agrawal A, Bucholz KK, et al. A twin study of alcohol dependence, binge eating, and compensatory behaivors. J Stud Alcohol Drugs. 2013;74:664–73.
Slane JD, Alexandra Burt S, Klump KL. Bulimic behaviors and alcohol use: shared genetic influences. Behav Genet. 2012;42(4):603–13.
Steiger H, Thaler L, Gauvin L, Joober R, Labbe A, Israel M, et al. Epistatic interactions involving DRD2, DRD4, and COMT polymorphisms and risk of substance abuse in women with binge-purge eating disturbances. J Psychiatr Res. 2016;77:8–14.
Davis C, Levitan RD, Yilmaz Z, Kaplan AS, Carter JC, Kennedy JL. Binge eating disorder and the dopamine D2 receptor: genotypes and sub-phenotypes. Prog Neuro-Psychopharmacol Biol Psychiatry. 2012;38(2):328–35.
Blum K, Sheridan PJ, Wood RC, Braverman ER, Chen TJH, Cull JG, et al. The D2 dopamine receptor deficiency syndrome. J R Soc Med. 1996;89:396–400.
Daviss C, Loxton NJ, Levitan RD, Kaplan AS, Carter JC, Kennedy JL. “Food addiction” and its association with a dopaminergic multilocus genetic profile. Physiol Behav. 2013;118:63–9.
Soyka M, Preuss UW, Hesselbrock V, Zill P, Koller G, Bondy B. GABA-A2 receptor subunit gene (GABRA2) polymorphisms and risk for alcohol dependence. J Psychiatr Res. 2008;42(3):184–91.
Loh EW, Higuchi S, Matsushita S, Murray R, Chen CK, Ball D. Association analysis of the GABA(A) receptor subunit genes cluster on 5q33-34 and alcohol dependence in a Japanese population. Mol Psychiatry. 2000;5(3):301–7.
•• Munn-Chernoff MA, Baker JH. A primer on the genetics of comorbid eating disorders and substance use disorders. Eur Eat Disord Rev. 2016;24(2):91–100. This article provides a clear and concise summary of the genetic evidence related to comorbidity of eating disorders and SUD. The authors argue that current molecular genetic methodologies have limitations that must be strongly considered.
•• Wiss DA, Criscitelli K, Gold M, Avena N. Preclinical evidence for the addiction potential of highly palatable foods: current developments related to maternal influence. Appetite Elsevier Ltd. 2017;115:19–27. This article highlights very recent research and finds evidence to support that in uetero exposure to maternal diet may confer risk for problematic eating patterns in off-spring.
Goodman A. Neurobiology of addiction. An integrative review. Biochem Pharmacol. 2008;75(1):266–322.
Hyman SE, Malenka RC. Addiction and the brain: the neurobiology of compulsion and its persistence. Nat Rev Neurosci. 2001;2(10):695–703.
Robinson TE, Berridge KC. The psychology and neurobiology of addiction: an incentive-sensitization view. Addiction. 2000;95(8s2):91–117.
Koob GF, Volkow ND. Neurobiology of addiction: a neurocircuitry analysis. Lancet Psychiatry. 2016;3(8):760–73.
Potenza MN. The neurobiology of pathological gambling and drug addiction: an overview and new findings. Philos Trans R Soc B Biol Sci. 2008;363(1507):3181–9.
Volkow ND, Wang GJ, Fowler JS, Tomasi D, Baler R. Food and drug reward : overlapping circuits in human obesity and addiction. Curr Top Behav Neurosci. 2011;11:1–24.
•• Brown RM, Kupchik YM, Spencer S, Garcia-Keller C, Spanswick DC, Lawrence AJ, et al. Addiction-like synaptic impairments in diet-induced obesity. Biol Psychiatry. 2017;81(9):797–806. Using well established experimental paradigms, this paper discusses an interaction between preexisting vulnerabilities (i.e., obesity prone rats) and exposure to highly palatable food, which was found to produce synaptic impairments similar to those observed in drug addiction.
•• Noori HR, Cosa Linan A, Spanagel R. Largely overlapping neuronal substrates of reactivity to drug, gambling, food and sexual cues: a comprehensive meta-analysis. Eur Neuropsychopharmacol. 2016;26(9):1419–30. This study reviews data from 176 functional neuroimaging studies utilizing activation likelihood estimation, which represents a significant analytic advancement within the last two decades. The research supports largely overlapping substrates between natural rewards (e.g., food) and drugs of abuse.
Volkow ND, Wang G-J, Tomasi D, Baler RD. Obesity and addiction: neurobiological overlaps. Obes Rev. 2013;14(1):2–18.
• Volkow ND, Baler RD. NOW vs LATER brain circuits: implications for obesity and addiction. Trends Neurosci. 2015;38(6):345–52. Comprehensive review paper on neurbiological circuitry involved in obesity and addiction.
García-García I, Horstmann A, Jurado MA, Garolera M, Chaudhry SJ, Margulies DS, et al. Reward processing in obesity, substance addiction and non-substance addiction. Obes Rev. 2014;15(11):853–69.
Grant JE, Chamberlain SR. Impulsive action and impulsive choice across substance and behavioral addictions: cause or consequence? Addict Behav. 2014;39(11):1632–9.
Comings DE, Blum K. Reward deficiency syndrome: genetic aspects of behavioral disorders. Prog Brain Res. 2000;126:325–41.
Morin J-P, Rodríguez-Durán LF, Guzmán-Ramos K, Perez-Cruz C, Ferreira G, Diaz-Cintra S, et al. Palatable hyper-caloric foods impact on neuronal plasticity. Front Behav Neurosci. 2017;11(February):1–11.
Volkow ND, Koob GF, McLellan AT. Neurobiologic advances from the brain disease model of addiction. N Engl J Med. 2016;374(4):363–71.
Kotov R, Gamez W, Schmidt F, Watson D. Linking “big” personality traits to anxiety, depressive, and substance use disorders: a meta-analysis. Psychol Bull. 2010;136(5):768–821.
Cyders M a, Smith GT, Spillane NS, Fischer S, Annus AM, Peterson C. Integration of impulsivity and positive mood to predict risky behavior: development and validation of a measure of positive urgency. Psychol Assess. 2007;19(1):107–18.
Dawe S, Loxton NJ. The role of impulsivity in the development of substance use and eating disorders. Neurosci Biobehav Rev. 2004;28(3):343–51.
MacKillop J, Mattson RE, Anderson Mackillop EJ, Castelda BA, Donovick PJ. Multidimensional assessment of impulsivity in undergraduate hazardous drinkers and controls. J Stud Alcohol Drugs. 2007;68(6):785–8.
Meule A, Platte P. Facets of impulsivity interactively predict body fat and binge eating in young women. Appetite. 2015;87:352–7.
VanderBroek-Stice L, Stojek MK, Beach SRH, VanDellen MR, MacKillop J. Multidimensional assessment of impulsivity in relation to obesity and food addiction. Appetite. 2017;112:59–68.
Murphy CM, Stojek MK, Mackillop J. Interrelationships among impulsive personality traits, food addiction, and body mass index. Appetite Elsevier Ltd. 2013;73:45–50.
• Stojek MM, Fischer S, Murphy CM, MacKillop J. The role of impulsivity traits and delayed reward discounting in dysregulated eating and drinking among heavy drinkers. Appetite. 2014;80:81–8. This study integrates behavioral and self-report measures of impulsivity in the context of eating and drinking behaviors, using a clinical sample. The evidence suggests nuances in the measurement and type of imulsivity in predicting behavior.
Wolz I, Granero R, Fernandez-Aranda F. A comprehensive model of food addiction in patients with binge-eating symptomatology: the essential role of negative urgency. Compr Psychiatry. 2017;74:118–24.
Pivarunas B, Conner BT. Impulsivity and and emotion dysregulation as predictors of food addiction. Eat Behav. 2015;19:9–14.
Dir AL, Karyadi K, Cyders MA. The uniqueness of negative urgency as a common risk factor for self-harm behaviors, alcohol consumption, and eating problems. Addict Behav. 2013;38(5):2158–62.
Mallorquí-Bagué N, Fagundo AB, Jimenez-Murcia S, De La Torre R, Baños RM, Botella C, et al. Decision making impairment: a shared vulnerability in obesity, gambling disorder and substance use disorders? PLoS One. 2016;11(9):1–11.
Reiter AMF, Heinze H-J, Schlagenhauf F, Deserno L. Impaired flexible reward-based decision-making in binge eating disorder: evidence from computational modeling and functional neuroimaging. Neuropsychopharmacology. 2017;42(3):628–37.
Schulte EM, Grilo CM, Gearhardt AN. Shared and unique mechanisms underlying binge eating disorder and addictive disorders. Clin Psychol Rev. 2016;44:125–39.
Velázquez-Sánchez C, Ferragud A, Moore CF, Everitt BJ, Sabino V, Cottone P. High trait impulsivity predicts food addiction-like behavior in the rat. Neuropsychopharmacology. 2014;39(10):2463–72.
Jupp B, Caprioli D, Dalley JW. Highly impulsive rats: modelling an endophenotype to determine the neurobiological, genetic and environmental mechanisms of addiction. Dis Model Mech. 2013;6(2):302–11.
Peña-Oliver Y, Giuliano C, Economidou D, Goodlett CR, Robbins TW, Dalley JW, et al. Alcohol-preferring rats show goal oriented behaviour to food incentives but are neither sign-trackers nor impulsive. PLoS One. 2015;10(6):1–16.
Diergaarde L, van Mourik Y, Pattij T, Schoffelmeer ANM, De Vries TJ. Poor impulse control predicts inelastic demand for nicotine but not alcohol in rats. Addict Biol. 2012;17(3):576–87.
Moschak TM, Terry DR, Daughters SB, Carelli RM. Low distress tolerance predicts heightened drug seeking and taking after extended abstinence from cocaine self-administration. Addict Biol. 2017; 23(1):1330–141.
Wills T, Shiffman S. Coping and substance use: a conceptual framework. In: Shiffman S, Wills T, editors. Coping and Substance Use. San Diego: Academic; 1985.
Leehr EJ, Krohmer K, Schag K, Dresler T, Zipfel S, Giel KE. Emotion regulation model in binge eating disorder and obesity—a systematic review. Neurosci Biobehav Rev. 2015;49:125–34.
Gianini LM, White MA, Masheb RM. Eating pathology, emotion regulation, and emotional overeating in obese adults with binge eating disorder. Eat Behav. 2013;14(3):309–13.
Haedt-Matt AA, Keel PK. Revisiting the affect regulation model of binge eating: a meta-analysis of studies using ecological momentary assessment. Psychol Bull. 2011;137(4):660–81.
Joyner MA, Schulte EM, Wilt AR, Gearhardt AN. Addictive-like eating mediates the association between eating motivations and elevated body mass index. Transl Issues Psychol Sci. 2015;1(3):217–28.
Kozak AT, Fought A. Beyond alcohol and drug addiction. Does the negative trait of low distress tolerance have an association with overeating? Appetite. 2011;57(3):578–81.
Loxton NJ, Tipman RJ. Reward sensitivity and food addiction in women. Appetite. 2017;115:28–35.
Kober H. Emotion regulation in substance use disorders. In: Gross JJ, editor. Handbook of emotion regulation. 2nd ed. New York: Guilford Press; 2014. p. 428–46.
Tull MT, Bardeen JR, DiLillo D, Messman-Moore T, Gratz KL. A prospective investigation of emotion dysregulation as a moderator of the relation between posttraumatic stress symptoms and substance use severity. J Anxiety Disord. 2015;29:52–60.
Haedt-Matt AA, Keel PK, Racine SE, Burt SA, Hu JY, Boker S, et al. Do emotional eating urges regulate affect? Concurrent and prospective associations and implications for risk models of binge eating. Int J Eat Disord. 2014;47(8):874–7.
Spence S, Courbasson C. The role of emotional dysregulation in concurrent eating disorders and substance use disorders. Eat Behav. 2012;13(4):382–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Food Addiction
Rights and permissions
About this article
Cite this article
Saules, K.K., Carr, M.M. & Herb, K.M. Overeating, Overweight, and Substance Use: What Is the Connection?. Curr Addict Rep 5, 232–242 (2018). https://doi.org/10.1007/s40429-018-0208-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40429-018-0208-9