Abstract
Purpose of the Review
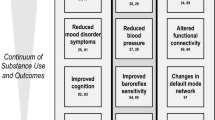
Substance use and overeating share phenomenological and neurophysiological characteristics. Researchers suggested that both dysfunctional behaviors may be improved with brain-directed treatments. This paper reviews 21 recent studies with applications of neurofeedback—an established brain-directed treatment technique—in both areas.
Recent Findings
While neurofeedback for substance use has a longer tradition, related research in the field of overeating emerged only recently. Encephalographic neurofeedback interventions in both areas show promising effects like reduced craving and psychological improvements. For functional brain imaging neurofeedback, most studies were still feasibility-focused. Participants were enabled to regulate their brain activity but effects on psychological outcomes remain unclear.
Summary
Neurofeedback may constitute a promising brain-directed treatment adjunct for substance use and overeating. However, further empirical foundation is needed—especially for functional brain imaging neurofeedback. Well-controlled study designs, comprehensive outcome assessments, and improved physiological methodology would increase our knowledge on the efficacy of this approach.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Avena NM, Bocarsly ME, Hoebel BG, Gold MS. Overlaps in the nosology of substance abuse and overeating: the translational implications of “food addiction”. Curr Drug Abuse Rev. 2011;4:133–9. doi:10.2174/1874473711104030133.
Davis C, Carter JC. Compulsive overeating as an addiction disorder. A review of theory and evidence. Appetite. 2009;2009(53):1–8. doi:10.1016/j.appet.2009.05.018.
Corsica JA, Pelchat ML. Food addiction: true or false? Curr Opin Gastroenterol. 2010;26:165–9. doi:10.1097/MOG.0b013e328336528d.
Ziauddeen H, Fletcher PC. Is food addiction a valid and useful concept? Obes Rev. 2013;14:19–28. doi:10.1111/j.1467-789X.2012.01046.x.
Avena NM, Gearhardt AN, Gold MS, Wang GJ, Potenza MN. Tossing the baby out with the bathwater after a brief rinse? The potential downside of dismissing food addiction based on limited data. Nat Rev Neurosci. 2012;13:514. doi:10.1038/nrn3212-c1.
Volkow ND, Wang GJ, Tomasi D, Baler RD. Obesity and addiction: neurobiological overlaps. Obes Rev. 2013;14:2–18. doi:10.1111/j.1467-789X.2012.01031.x.
Gearhardt AN, Yokum S, Orr PT, Stice E, Corbin WR, Brownell KD. Neural correlates of food addiction. Arch Gen Psychiatry. 2011;68:808–16. doi:10.1001/archgenpsychiatry.2011.32.
Kober H, Mende-Siedlecki P, Kross EF, Weber J, Mischel W, Hart CL, Ochsner KN. Prefrontal–striatal pathway underlies cognitive regulation of craving. P Natl Acad Sci USA. 2010;2010(107):14811–6. doi:10.1073/pnas.1007779107.
Heatherton TF, Wagner DD. Cognitive neuroscience of self-regulation failure. Trends Cogn Sci. 2011;15:132–9. doi:10.1016/j.tics.2010.12.005.
Dutra L, Stathopoulou G, Basden SL, Leyro TM, Powers MB, Otto MW. A meta-analytic review of psychosocial interventions for substance use disorders. Am J Psychiatry. 2008;165:179–87. doi:10.1176/appi.ajp.2007.06111851.
Brandon TH, Vidrine JI, Litvin EB. Relapse and relapse prevention. Annu Rev Clin Psychol. 2007;3:257–84. doi:10.1146/annurev.clinpsy.3.022806.091455.
Val-Laillet D, Aarts E, Weber B, Ferrari M, Quaresima V, Stoeckel LE, et al. Neuroimaging and neuromodulation approaches to study eating behavior and prevent and treat eating disorders and obesity. NeuroImage: Clinical. 2015;8:1–31. doi:10.1016/j.nicl.2015.03.016.
Feldstein Ewing SW, Chung T. Neuroimaging mechanisms of change in psychotherapy for addictive behaviors: emerging translational approaches that bridge biology and behavior. Psychol Addict Behav. 2013;27:329–35. doi:10.1037/a0031491.
Whitten LA. Translational neuroscience and potential contributions of functional magnetic resonance imaging (fMRI) to the prevention of substance misuse and antisocial behavior. Prev Sci. 2013;14:238–46. doi:10.1007/s11121-012-0341-y.
Schmidt U, Campbell IC. Treatment of eating disorders can not remain ‘brainless’: the case for brain-directed treatments. Eur Eat Disord Rev. 2013;21:425–7. doi:10.1002/erv.2257.
Cannon RL. Editorial perspective: defining neurofeedback and its functional processes. NeuroRegul. 2015;2:60–9. doi:10.15540/nr.2.2.60.
Hammond DC. What is neurofeedback: an update. J Neurother. 2011;15:305–36. doi:10.1080/10874208.2011.623090.
Niv S. Clinical efficacy and potential mechanisms of neurofeedback. Pers Indiv Differ. 2013;54:676–86. doi:10.1016/j.paid.2012.11.037.
Sherlin LH, Arns M, Lubar J, Heinrich H, Kerson C, Strehl U, et al. Neurofeedback and basic learning theory: implications for research and practice. J Neurother. 2011;15:292–304. doi:10.1080/10874208.2011.623089.
Sitaram R, Ros T, Stoeckel L, Haller S, Scharnowski F, Lewis-Peacock J, et al. Closed-loop brain training: the science of neurofeedback. Nat Rev Neurosci. 2017;18:86–100. doi:10.1038/nrn.2016.164.
Christoffersen GR, Schachtman TR. Electrophysiological CNS-processes related to associative learning in humans. Behav Brain Res. 2016;296:211–32. doi:10.1016/j.bbr.2015.09.011.
Glannon W. Neuromodulation, agency and autonomy. Brain Topogr. 2014;27:46–54. doi:10.1007/s10548-012-0269-3.
• Strehl U. What learning theories can teach us in designing neurofeedback treatments. Front Hum Neurosci. 2014;8:894. doi:10.3389/fnhum.2014.00894. This paper points out important methodological issues that should be considered in the design of neurofeedback intervention for clinical applications
• Thibault RT, Lifshitz M, Birbaumer N, Raz A. Neurofeedback, self-regulation, and brain imaging: clinical science and fad in the service of mental disorders. Psychother Psychosom. 2015;84:193–207. doi:10.1159/000371714. This paper provides a very good overview on common neurofeedback methods but also takes a very critical look at the neurofeedback approach, followed by good suggestions for approaches that tackle methodological problems
• Gruzelier JH. EEG neurofeedback for optimising performance. III: A review of methodological and theoretical considerations. Neurosci Biobehav Rev. 2014;44:159–82. doi:10.1016/j.neubiorev.2014.03.015. This recent review explains several different outcomes in neurofeedback research and describes a wide range of theoretical and methodological matters that neurofeedback researchers should be informed about and address in their studies
Yuan H, Young KD, Phillips R, Zotev V, Misaki M, Bodurka J. Resting-state functional connectivity modulation and sustained changes after real-time functional magnetic resonance imaging neurofeedback training in depression. Brain connectivity. 2014;4:690–701. doi:10.1089/brain.2014.0262.
Yucha C, Montgomery D. Evidence-based practice in biofeedback and neurofeedback. Wheat Ridge: AAPB; 2008.
Trudeau DL. EEG biofeedback for addictive disorders—the state of the art in 2004. J Adult Dev. 2005;12:139–46. doi:10.1007/s10804-005-7030-z.
Sokhadze TM, Cannon RL, Trudeau DL. EEG biofeedback as a treatment for substance use disorders: review, rating of efficacy and recommendations for further research. Appl Psychophys Biof. 2008;33:1–28. doi:10.1007/s10484-007-9047-5.
Weiskopf N. Real-time fMRI and its application to neurofeedback. NeuroImage. 2012;62:682–92. doi:10.1016/j.neuroimage.2011.10.009.
Peniston EG, Kulkosky PJ. Alpha-theta brainwave training and beta endorphin levels in alcoholics. Alcohol Clin Exp Res. 1989;13:271–9.
Peniston EG, Kulkosky PJ. Alcoholic personality and alpha-theta brainwave training. Med Psychother. 1990;2:37–55.
Rangaswamy M, Porjesz B, Chorlian DB, Wang K, Jones KA, Bauer LO, et al. Beta power in the EEG of alcoholics. Biol Psychiatry. 2002;52:831–42. doi:10.1016/S0006-3223(02)01362-8.
Scott W, Kaiser D. Augmenting chemical dependency treatment with neurofeedback training. J Neurother. 1998;3:66.
Scott WC, Kaiser D, Othmer S, Sideroff SI. Effects of an EEG biofeedback protocol on a mixed substance abusing population. Am J Drug Alcohol Ab. 2005;31:455–69. doi:10.1081/ADA-200056807.
Stevens L, Verdejo-García A, Goudriaan AE, Roeyers H, Dom G, Vanderplasschen W. Impulsivity as a vulnerability factor for poor addiction treatment outcomes: a review of neurocognitive findings among individuals with substance use disorders. J Subst Abus Treat. 2014;47:58–72. doi:10.1016/j.jsat.2014.01.008.
Schneider F, Elbert T, Heimann H, Welker A, Stetter F, Mattes R, et al. Self-regulation of slow cortical potentials in psychiatric patients: alcohol dependency. Biofeedback Self-Reg. 1993;18:23–32. doi:10.1007/BF00999511.
Sulzer J, Haller S, Scharnowski F, Weiskopf N, Birbaumer N, Blefari ML, et al. Real-time fMRI neurofeedback: progress and challenges. NeuroImage. 2013;76:386–99. doi:10.1016/j.neuroimage.2013.03.033.
• Thibault RT, Lifshitz M, Raz A. The self-regulating brain and neurofeedback: experimental science and clinical promise. Cortex. 2016;74:247–61. doi:10.1016/j.cortex.2015.10.024. This paper extensively introduces and argues for the use of proper approaches and especially control groups in clinical neurofeedback research
de Charms RC, Maeda F, Glover GH, Ludlow D, Pauly JM, Soneji D, et al. Control over brain activation and pain learned by using real-time functional MRI. P Natl Acad Sci USA. 2005;102:18626–31. doi:10.1073/pnas.0505210102.
Tang YY, Posner MI, Rothbart MK, Volkow ND. Circuitry of self-control and its role in reducing addiction. Trends Cognitive Sci. 2015;19:439–44. doi:10.1016/j.tics.2015.06.007.
Koob GF, Volkow ND. Neurocircuitry of addiction. Neuropsychopharmacology. 2010;35:217–38. doi:10.1038/npp.2009.110.
Tang DW, Fellows LK, Small DM, Dagher A. Food and drug cues activate similar brain regions: a meta-analysis of functional MRI studies. Physiol Behav. 2012;106:317–24.
Bartholdy S, Musiat P, Campbell IC, Schmidt U. The potential of neurofeedback in the treatment of eating disorders: a review of the literature. Eur Eat Disord Rev. 2013;21:456–63. doi:10.1002/erv.2250.
Dehghani-Arani F, Rostami R, Nostratabadi M. Effectiveness of neurofeedback training as a treatment for opioid-dependent patients. Clin EEG Neurosci. 2010;41:170–7. doi:10.1177/155005941004100313.
Dehghani-Arani F, Rostami R, Nadali H. Neurofeedback training for opiate addiction: improvement of mental health and craving. Appl Psychophys Biof. 2013;38:133–41. doi:10.1007/s10484-013-9218-5.
• Hashemian P. The effectiveness of neurofeedback therapy in craving of methamphetamine use. Open J Psychiatry. 2015;5:177–9. doi:10.4236/ojpsych.2015.52020. This study provides the only EEG neurofeedback study in our review that examined a sham control group and reported superiority of veritable EEG neurofeedback to sham neurofeedback
Horrell T, El-Baz A, Baruth J, Tasman A, Sokhadze G, Stewart C, Sokhadze E. Neurofeedback effects on evoked and induced EEG gamma band reactivity to drug-related cues in cocaine addiction. J Neurother. 2010;14(3):195–216. doi:10.1080/10874208.2010.501498.
• Rostami R, Dehghani-Arani F. Neurofeedback training as a new method in treatment of crystal methamphetamine dependent patients: a preliminary study. Appl Psychophys Biof. 2015;40:151–61. doi:10.1007/s10484-015-9281-1. This study provides a good overview on the most prevalent protocol in recent EEG neurofeedback for substance use (Scott-Kaiser modification of the Peniston protocol) and further constitutes the study with the highest statistical power in our review, showing efficacy of EEG neurofeedback for the treatment of methamphetamine dependence
Lackner N, Unterrainer HF, Skliris D, Wood G, Wallner-Liebmann SJ, Neuper C, Gruzelier JH. The effectiveness of visual short-time neurofeedback on brain activity and clinical characteristics in alcohol use disorders: practical issues and results. Clin EEG Neurosci. 2015;47:188–95. doi:10.1177/1550059415605686.
• Keith JR, Rapgay L, Theodore D, Schwartz JM, Ross JL. An assessment of an automated EEG biofeedback system for attention deficits in a substance use disorders residential treatment setting. Psychol Addict Behav. 2015;9:17–25. doi:10.1037/adb0000016. This paper is the only study to date that compared clinician-guided and automated neurofeedback with comparable beneficial effects. Further, the study design of this trial is highly commendable
Canterberry M, Hanlon CA, Hartwell KJ, Li X, Owens M, LeMatty T, et al. Sustained reduction of nicotine craving with real-time neurofeedback: exploring the role of severity of dependence. Nicotine Tob Res. 2013;15:2120–4. doi:10.1093/ntr/ntt122.
Hanlon CA, Hartwell KJ, Canterberry M, Li X, Owens M, LeMatty T, et al. Reduction of cue-induced craving through realtime neurofeedback in nicotine users: the role of region of interest selection and multiple visits. Psychiatry Res-Neuroim. 2013;213:79–81. doi:10.1016/j.pscychresns.2013.03.003.
• Hartwell KJ, Hanlon CA, Li X, Borckardt JJ, Canterberry M, Prisciandaro JJ, et al. Individualized real-time fMRI neurofeedback to attenuate craving in nicotine-dependent smokers. J Psychiatry Neurosci 2016;41:48–55. doi:10.1503/jpn.140200. This study was the only fMRI neurofeedback study for nicotine craving that included a no-feedback control group, showing superior effects of fMRI neurofeedback with regard to reductions in craving-related brain activity
• Kim DY, Yoo SS, Tegethoff M, Meinlschmidt G, Lee JH. The inclusion of functional connectivity information into fMRI-based neurofeedback improves its efficacy in the reduction of cigarette cravings. J Cogn Neurosci. 2015;27:1552–72. doi:10.1162/jocn_a_00802. This trial was the first one to compare veritable fMRI neurofeedback for substance use that either did or did not include feedback on functional connectivity. The latter one lead to greater modulation of neural activity related to cigarette craving
Li X, Hartwell KJ, Borckardt J, Prisciandaro JJ, Saladin ME, Morgan PS, et al. Volitional reduction of anterior cingulate cortex activity produces decreased cue craving in smoking cessation: a preliminary real-time fMRI study. Addicti Biol. 2013;18(4):739–48. doi:10.1111/j.1369-1600.2012.00449.
• Kirsch M, Gruber I, Ruf M, Kiefer F, Kirsch P. Real-time functional magnetic resonance imaging neurofeedback can reduce striatal cue-reactivity to alcohol stimuli. Addict Biology. 2015;21:982–92. doi:10.1111/adb.12278. This study compared veritable and yolk fMRI neurofeedback, showing that only veritable neurofeedback enabled participants to downregulate striatal activity
• Karch S, Keeser D, Hümmer S, Paolini M, Kirsch V, Karali T, et al. Modulation of craving related brain responses using real-time fMRI in patients with alcohol use disorder. PLoS One. 2015;10:e0133034. doi:10.1371/journal.pone.0133034. This was the only fMRI neurofeedback study that included a patient sample with alcohol dependency, showing that there is a wide variance in the ability of clinical patients to regulate the BOLD signal
• Schmidt J, Martin A. Neurofeedback reduces overeating episodes in female restrained eaters: a randomized controlled pilot-study. Appl Psychophys Biof. 2015;40:283–95. doi:10.1007/s10484-015-9297-6. This study was the first study to apply EEG neurofeedback to explicitly target overeating behaviors, showing beneficial effects compared to a waitlist. It is further the first study to develop and apply a cue exposure EEG neurofeedback protocol
• Schmidt J, Martin A. Neurofeedback against binge eating: a randomized controlled trial in a female subclinical threshold sample. Eur Eat Disord Rev. 2016;24:406–16. doi:10.1002/erv.2453. This RCT provides an example for the use of non-sham control groups in EEG neurofeedback research
• Imperatori C, Valenti EM, Della Marca G, Amoroso N, Massullo C, Carbone GA, et al. Coping food craving with neurofeedback. Evaluation of the usefulness of alpha/theta training in a non-clinical sample. Int J Psychophysiol 2017;112:89–97. doi:10.1016/j.ijpsycho.2016.11.010. This study was the first to transfer an alpha-theta training in EEG neurofeedback to the field of phenomena related to eating behavior with beneficial effects on food craving and observable changes in the resting-EEG, assessed with sophisticated high-resolution EEG analyses. Further, the well-designed report of the trial and blinded study design have to be highlighted
Chirita-Emandi A, Puiu M. Outcomes of neurofeedback training in childhood obesity management: a pilot study. J Altern Complem Med. 2014;20:831–7. doi:10.1089/acm.2014.0040.
Frank S, Lee S, Preissl H, Schultes B, Birbaumer N, Veit R. The obese brain athlete: self-regulation of the anterior insula in adiposity. PLoS One. 2012;7:e42570. doi:10.1371/journal.pone.0042570.
• Ihssen N, Sokunbi MO, Lawrence AD, Lawrence NS, Linden DE. Neurofeedback of visual food cue reactivity: a potential avenue to alter incentive sensitization and craving. Brain Imag Behav. 2016; doi:10.1007/s11682-016-9558-x. This is the first study that explicitly examined fMRI neurofeedback for regulation of visual food-cue reactivity. The applied motivational neurofeedback further constitutes an interesting new design for neurofeedback applications
• Spetter MS, Malekshahi R, Birbaumer N, Lührs M, van der Veer AH, Scheffler K, et al. Volitional regulation of brain responses to food stimuli on overweight and obese subjects: a real-time fMRI feedback study. Appetite 2017;112:188–95. doi:10.1016/j.appet.2017.01.032. This is the first fMRI neurofeedback study that examined a protocol based on functional connectivity in the domain of eating behavior. It further demonstrates how behavioral food intake tests can be used to determine outcomes of the interventions
Boswell RG, Kober H. Food cue reactivity and craving predict eating and weight gain: a meta-analytic review. Obes Rev. 2016;17:159–77. doi:10.1111/obr.12354.
Weiss F. Neurobiology of craving, conditioned reward and relapse. Curr Opin Pharmacol. 2005;5:9–19. doi:10.1016/j.coph.2004.11.001.
Welberg L. Addiction: craving: a core issue. Nat Rev Neurosci. 2013;14:307. doi:10.1038/nrn3483.
Ros T, Théberge J, Frewen PA, Kluetsch R, Densmore M, Calhoun VD, Lanius RA. Mind over chatter: plastic up-regulation of the fMRI salience network directly after EEG neurofeedback. NeuroImage. 2013;65:324–35. doi:10.1016/j.neuroimage.2012.09.046.
Ninaus M, Kober SE, Witte M, Koschutnig K, Stangl M, Neuper C, Wood G. Neural substrates of cognitive control under the belief of getting neurofeedback training. Front Hum Neurosci. 2013;7:62–71. doi:10.3389/fnhum.2013.00914.
Chung T, Noronha A, Carroll KM, Potenza MN, Hutchison K, Calhoun VD, et al. Brain mechanisms of change in addiction treatment: models, methods, and emerging findings. Curr Addict Rep. 2016;3:332–42. doi:10.1007/s40429-016-0113-z.
Potenza MN, Sofuoglu M, Carroll KM, Rounsaville BJ. Neuroscience of behavioral and pharmacological treatments for addictions. Neuron. 2011;69:695–712. doi:10.1016/j.neuron.2011.02.009.
Garrison KA, Potenza MN. Neuroimaging and biomarkers in addiction treatment. Curr Psychiatry Rep. 2014;16:513. doi:10.1007/s11920-014-0513-5.
Campbell M, Fitzpatrick R, Haines A, Kinmonth AL. Framework for design and evaluation of complex interventions to improve health. Brit Med J. 2000;321:694–6. doi:10.1136/bmj.321.7262.694.
La Vaque TJ, Rossiter T. The ethical use of placebo controls in clinical research: the Declaration of Helsinki. Appl Psychophys Biof. 2001;26:23–37. doi:10.1023/A:1009563504319.
Colloca L, Miller FG. The nocebo effect and its relevance for clinical practice. Psychosom Med. 2011;73:598–603. doi:10.1097/PSY.0b013e3182294a50.
Kirshenbaum AP, Olsen DM, Bickel WK. A quantitative review of the ubiquitous relapse curve. J Subst Abus Treat. 2009;36:8–17. doi:10.1016/j.jsat.2008.04.001.
Wing RR, Phelan S. Long-term weight loss maintenance. Am J Clin Nutr. 2005;82:222S–5S.
Button KS, Ioannidis JPA, Mokrysz C, Nosek BA, Flint J, Robinson ESJ, Munafò MR. Power failure: why small sample size undermines the reliability of neuroscience. Nat Rev Neurosci. 2013;14:365–76. doi:10.1038/nrn3475.
Eklund A, Nichols TE, Knutsson H. Cluster failure: why fMRI inferences for spatial extent have inflated false-positive rates. P Natl Acad Sci USA. 2016;113:7900–5. doi:10.1073/pnas.1602413113.
Gusnard DA, Raichle ME. Searching for a baseline: functional imaging and the resting human brain. Nat Rev Neurosci. 2001;2001(2):685–94. doi:10.1038/35094500.
Raichle ME, MacLeod AM, Snyder AZ, Powers WJ, Gusnard DA, Shulman GL. A default mode of brain function. P Natl Acad Sci USA. 2001;98:676–82. doi:10.1073/pnas.98.2.676.
Porjesz B, Rangaswamy M, Kamarajan C, Jones KA, Padmanabhapillai A, Begleiter H. The utility of neurophysiological markers in the study of alcoholism. Clin Neurophysiol. 2005;116:993–1018. doi:10.1016/j.clinph.2004.12.016.
Ersche KD, Williams GB, Robbins TW, Bullmore ET. Meta-analysis of structural brain abnormalities associated with stimulant drug dependence and neuroimaging of addiction vulnerability and resilience. Curr Opin Neurobiol. 2013;23:615–24. doi:10.1016/j.conb.2013.02.017.
Parvaz MA, Alia-Klein N, Woicik PA, Volkow ND, Goldstein RZ. Neuroimaging for drug addiction and related behaviors. Rev Neurosci. 2011;22(6):609–24. doi:10.1515/RNS.2011.055.
• Stoeckel LE, Garrison KA, Ghosh SS, Wighton P, Hanlon CA, Gilman JM, et al. Optimizing real time fMRI neurofeedback for therapeutic discovery and development. NeuroImage-Clin. 2014;5:245–55. doi:10.1016/j.nicl.2014.07.002. This paper provides a very good guideline for the design and application of studies using fMRI neurofeedback
Keil A, Debener S, Gratton G, Junghöfer M, Kappenman ES, Luck SJ, et al. Committee report: publication guidelines and recommendations for studies using electroencephalography and magnetoencephalography. Psychophysiology. 2014;51:1–21. doi:10.1111/psyp.12147.
Schulz KF, Altman DG, Moher D, for the CONSORT Group. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. Trials. 2010;11:32. doi:10.1186/1745-6215-11-32.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Jennifer Schmidt, Christian Kärgel, and Mareile Opwis declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Food Addiction
Rights and permissions
About this article
Cite this article
Schmidt, J., Kärgel, C. & Opwis, M. Neurofeedback in Substance Use and Overeating: Current Applications and Future Directions. Curr Addict Rep 4, 116–131 (2017). https://doi.org/10.1007/s40429-017-0137-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40429-017-0137-z