Abstract
Cardiovascular events are the consequence of vascular damage at both the macro and microcirculatory level. The relationship between large stiffening artery and microvascular disease may be bidirectional, since wave reflection from microvascular sites could increase systolic blood pressure and pulse pressure, while transmission of increased arterial pulsatility to microvessels could represent a mechanism of damage. Hypertension and aging share similar mechanisms of vascular dysfunction. In fact, vascular remodelling, endothelial dysfunction and vascular stiffness are common features in hypertension and aging. Structural and functional changes in small arteries occur during normal and accelerated aging, possibly triggered by hypertension. A cross-talk may be present between large and small artery changes, interacting with pressure wave transmission and reflection, exaggerating cardiac, brain and kidney damage, and finally leading to cardiovascular and renal complications.



Similar content being viewed by others
References
Nilsson PM, Boutouyrie P, Laurent S. Vascular aging: a tale of EVA and ADAM in cardiovascular risk assessment and prevention. Hypertension. 2009;54:3–10.
Weber T, Segers P. Changes in central hemodynamics, wave reflection, and heart-vessel coupling with normal and accelerated aging. In: Nilsson P, Olsen MH, Laurent S (eds) Early vascular aging (EVA): new directions in cardiovascular protection. pp 83–95, 2015.
Laurent S, Agabiti-Rosei E. The cross-talk between the macro- and the microcirculation. In: Nilsson P, Olsen MH, Laurent S (eds) Early vascular aging (EVA): new directions in cardiovascular protection. pp 105–118, 2015.
Laurent S, Rizzoni D. Targeting central blood pressure through the micro-and macrocirculation cross-talk. In: Nilsson P, Olsen MH, Laurent S (eds) Early vascular aging (EVA): new directions in cardiovascular protection. pp 297–306, 2015.
Reference Values for Arterial Stiffness Collaboration. Determinants of pulse wave velocity in healthy people and in the presence of cardiovascular risk factors: establishing normal and reference values. Eur Heart J. 2010;31:2338–50.
Mulvany MJ, Aalkjaer C. Structure and function of small arteries. Physiol Rev. 1990;70:921–71.
Rizzoni D, Castellano M, Porteri E, Bettoni G, Muiesan ML, Agabiti Rosei E. Delayed development of hypertension after short-term nitrendipine treatment. Hypertension. 1994;24:131–9.
Aalkjaer C, Eiskjaer H, Mulvany MJ, Jespersen B, Kjaer T, Sorensen SS, Pedersen EB. Abnormal structure and function of isolated subcutaneous resistance vessels from essential hypertensive patients despite antihypertensive treatment. J Hypertens. 1989;7:305–10.
Heagerty AM, Aalkjaaer C, Bund SJ, Korsgaard N, Mulvany MJ. Small artery structure in hypertension. Dual process of remodeling and growth. Hypertension. 1993;21:391–7.
Rizzoni D, Porteri E, Castellano M, Bettoni G, Muiesan ML, Muiesan P, Giulini SM, Agabiti Rosei E. Vascular hypertrophy and remodeling in secondary hypertension. Hypertension. 1996;28:785–90.
Rizzoni D, Porteri E, Guelfi D, Muiesan ML, Valentini U, Cimino A, Girelli A, Rodella L, Bianchi R, Sleiman I, Agabiti Rosei E. Structural alterations in subcutaneous small arteries of normotensive and hypertensive patients with non insulin dependent diabetes mellitus. Circulation. 2001;103:1238–44.
Boutouyrie P, Laurent S, Briet M. Importance of arterial stiffness as cardiovascular risk factor for future development of new type of drugs. Fundam Clin Pharmacol. 2008;22:241–6.
Mahmud A, Feely J. Spurious systolic hypertension of youth: fit young men with elastic arteries. Am J Hypertens. 2003;16(3):229–32.
Laurent S, Cockcroft J, Van Bortel L, Boutouyrie P, Giannattasio C, Hayoz D, Pannier B, Vlachopoulos C, Wilkinson I, Struijker-Boudier H, On behalf of the European Network for Non-invasive Investigation of Large Arteries. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J. 2006;27:2588–605.
Agabiti-Rosei E, Mancia G, O’Rourke MF, Roman MJ, Safar ME, Smulyan H, Wang JG, Wilkinson IB, Williams B, Vlachopoulos C. Central blood pressure measurements and antihypertensive therapy: a consensus document. Hypertension. 2007;50:154–60.
McEniery CM, Yasmin A, Hall IR, Qasem A, Wilkinson IB, Cockcroft JR, ACCT Investigators. Normal vascular aging: differential effects on wave reflection and aortic pulse wave velocity: the Anglo-Cardiff Collaborative Trial (ACCT). Am Coll Cardiol. 2005;46(9):1753–60.
Weber T, Wassertheurer S, Schmidt-Trucksäss A, Rodilla E, Ablasser C, Jankowski P, Lorenza Muiesan M, Giannattasio C, Mang C, Wilkinson I, Kellermair J, Hametner B, Pascual JM, Zweiker R, Czarnecka D, Paini A, Salvetti M, Maloberti A, McEniery C. Relationship between 24-h ambulatory central systolic blood pressure and left ventricular mass: a prospective multicenter study. Hypertension. 2017;70:1157–64.
Safar ME, Rizzoni D, Blacher J, Muiesan ML, Agabiti-Rosei E. Macro and microvasculature in hypertension: therapeutic aspects. J Hum Hypertens. 2008;22(9):590–5.
Westerhof BE, van den Wijngaard JP, Murgo JP, Westerhof N. Location of a reflection site is elusive: consequences for the calculation of aortic pulse wave velocity. Hypertension. 2008;52(3):478–83.
Rehman A, Schiffrin EL. Vascular effects of antihypertensive drug therapy. Curr Hypertens Rep. 2010;12:226–32.
Rizzoni D, Porteri E, Boari GEM, De Ciuceis C, Sleiman I, Muiesan ML, Castellano M, Miclini M, Agabiti-Rosei E. Prognostic significance of small artery structure in hypertension. Circulation. 2003;108:2230–5.
Boari GE, Rizzardi N, de Ciuceis C, Platto C, Paiardi S, Porteri E, Paini A, Salvetti M, Muiesan ML, Rizzoni D, Agabiti-Rosei E. Determinants of the structure of resistance-sized arteries in hypertensive patients. Blood Press. 2008;17(4):204–11.
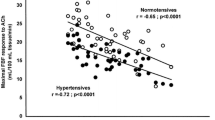
Muiesan ML, Salvetti M, Rizzoni D, Paini A, Agabiti-Rosei C, Aggiusti C, Bertacchini F, Stassaldi D, Gavazzi A, Porteri E, De Ciuceis C, Agabiti-Rosei E. Pulsatile hemodynamics and microcirculation: evidence for a close relationship in hypertensive patients. Hypertension. 2013;61:130–6.
Harazny JM, Ritt M, Baleanu D, Ott C, Heckmann J, Schlaich MP, Michelson G, Schmieder RE. Increased wall:lumen ratio of retinal arterioles in male patients with a history of a cerebrovascular event. Hypertension. 2007;50(4):623–829.
Rizzoni D, Porteri E, Duse S, De Ciuceis C, Agabiti Rosei C, La Boria E, Semeraro F, Costagliola C, Sebastiani A, Danzi P, Tiberio GA, Giulini SM, Docchio F, Sansoni G, Sarkar A, Agabiti Rosei E. J Hypertens. 2012;30:1169–75.
Ott C, Raff U, Harazny JM, Michelson G, Schmieder RE. Central pulse pressure is an independent determinant of vascular remodeling in the retinal circulation. Hypertension. 2013;61:1340–5.
Salvetti M, Agabiti Rosei C, Paini A, Aggiusti C, Cancarini A, Duse S, Semeraro F, Rizzoni D, Agabiti Rosei E, Muiesan ML. Relationship of wall-to-lumen ratio of retinal arterioles with clinic and 24-hour blood pressure. Hypertension. 2014;63:1110–5.
Paini A, Muiesan ML, Agabiti-Rosei C, Aggiusti C, De Ciuceis C, Bertacchini F, Duse S, Semeraro F, Rizzoni D, Agabiti-Rosei E, Salvetti M. Carotid stiffness is significantly correlated with wall-to-lumen ratio of retinal arterioles. J Hypertens. 2018;36:580–6.
Laurent S, Briet M, Boutouyrie P. Large and small artery cross-talk and recent morbidity-mortality trials in hypertension. Hypertension. 2009;54:388–92.
Hashimoto J, Aikawa T, Imai Y. Large artery stiffening as a link between cerebral lacunar infarction and renal albuminuria. Am J Hypertens. 2008;21(12):1304–9.
Brisset M, Boutouyrie P, Pico F, Zhu Y, Zureik M, Schilling S, Dufouil C, Mazoyer B, Laurent S, Tzourio C, Debette S. Large-vessel correlates of cerebral small-vessel disease. Neurology. 2013;80:662–9.
Wåhlin A, Ambarki K, Birgander R, Malm J, Eklund A. Intracranial pulsatility is associated with regional brain volume in elderly individuals. Neurobiol Aging. 2014;35:365–72.
Lamballais S, Sajjad A, Leening MJG, Gaillard R, Franco OH, Mattace-Raso FUS, Jaddoe VWV, Roza SJ, Tiemeier H, Ikram MA. Association of blood pressure and arterial stiffness with cognition in 2 population-based child and adult cohorts. J Am Heart Assoc. 2018;7:e009847.
Waldstein SR, Rice SC, Thayer JF, Najjar SS, Scuteri A, Zonderman AB. Pulse pressure and pulse wave velocity are related to cognitive decline in the Baltimore Longitudinal Study of Aging. Hypertension. 2008;51:99–104.
SPRINT MIND Investigators for the SPRINT Research Group, Williamson JD, Pajewski NM, Auchus AP, Bryan RN, Chelune G, Cheung AK, Cleveland ML, Coker LH, Crowe MG, Cushman WC, Cutler JA, Davatzikos C, Desiderio L, Erus G, Fine LJ, Gaussoin SA, Harris D, Hsieh MK, Johnson KC, Kimmel PL, Tamura MK, Launer LJ, Lerner AJ, Lewis CE, Martindale-Adams J, Moy CS, Nasrallah IM, Nichols LO, Oparil S, Ogrocki PK, Rahman M, Rapp SR, Reboussin DM, Rocco MV, Sachs BC, Sink KM, Still CH, Supiano MA, Snyder JK, Wadley VG, Walker J, Weiner DE, Whelton PK, Wilson VM, Woolard N, Wright JT Jr, Wright CB. Effect of intensive vs standard blood pressure control on probable dementia: a randomized clinical trial. JAMA. 2019;321:553–61.
Mitchell GF, van Buchem MA, Sigurdsson S, Gotal JD, Jonsdottir MK, Kjartansson Ó, Garcia M, Aspelund T, Harris TB, Gudnason V, Launer LJ. Arterial stiffness, pressure and flow pulsatility and brain structure and function: the Age. Gene/Environment Susceptibility-Reykjavik study. Brain. 2011;134(Pt 11):3398–407.
Webb AJ, Simoni M, Mazzucco S, Kuker W, Schulz U, Rothwell PM. Increased cerebral arterial pulsatility in patients with leukoaraiosis: arterial stiffness enhances transmission of aortic pulsatility. Stroke. 2012;43:2631–6.
O’Rourke MF, Safar ME. Relationship between aortic stiffening and microvascular disease in brain and kidney: cause and logic of therapy. Hypertension. 2005;46:200–4.
Scuteri A, Nilsson PM, Tzourio C, Redon J, Laurent S. Microvascular brain damage with aging and hypertension: pathophysiological consideration and clinical implications. J Hypertens. 2011;29:1469–77.
Taddei S, Virdis A, Mattei P, Ghiadoni L, Fasolo CB, Sudano I, Salvetti A. Hypertension causes premature aging of endothelial function in humans. Hypertension. 1997;29:736–43.
De Ciuceis C, Rossini C, Agabiti Rosei C, Sarkar A, Porteri E, La Boria E, Gavazzi A, Petroboni B, Pileri P, Agabiti Rosei E, Rizzoni D. Relationship between age and structural alterations in subcutaneous small resistance arteries in hypertensive patients. In: 25th European meeting on Hypertension and cardiovascular protection (ESH) 2015, Milan, 12–15 June, e100 (7D.03), 2015.
Bruno RM, Duranti E, Ippolito C, Segnani C, Bernardini N, Di Candio G, Chiarugi M, Taddei S, Virdis A. Different impact of essential hypertension on structural and functional age-related vascular changes. Hypertension. 2017;69:71–8.
Bruno RM, Grassi G, Seravalle G, Savoia C, Rizzoni D, Virdis A, Study Group on Micro- and Macrocirculation of the Italian Society of Hypertension (SIIA). Age- and sex-specific reference values for media/lumen ratio in small arteries and relationship with risk factors. Hypertension. 2018;71:1193–200.
Savoia C, Battistoni A, Calvez V, Cesario V, Montefusco G, Filippini A. Microvascular alterations in hypertension and vascular aging. Curr Hypertens Rev. 2017;13:16–23.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Rizzoni, D., Rizzoni, M., Nardin, M. et al. Vascular Aging and Disease of the Small Vessels. High Blood Press Cardiovasc Prev 26, 183–189 (2019). https://doi.org/10.1007/s40292-019-00320-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40292-019-00320-w