Abstract
Background
The absence of evidence-based guidelines make medical disqualification (MDQ) following concussion one of the most challenging decision-making processes faced by sports medicine professionals.
Objective
We aimed to compare premorbid and postmorbid factors between student-athletes that were and were not medically disqualified from sport following a concussion.
Methods
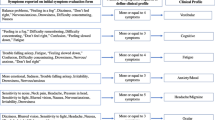
Among 1832 student-athletes diagnosed with concussion within the CARE Consortium, 53 (2.9%) were medically disqualified (MDQ +) and 1779 (97.1%) were not medically disqualified (MDQ−). We used contingency tables and descriptive statistics for an initial evaluation of a broad list of premorbid and postmorbid factors. For those factors showing association with MDQ status, we calculated odds ratios and 95% confidence intervals for the odds of being MDQ + in the presence of the identified factor.
Results
History of 2 (OR: 3.2, 95% CI 1.5, 6.9) or 3 + (OR: 7.4, 95% CI 3.4, 15.9) previous concussions; 1 + headaches in past 3 months (OR: 1.8, 95% CI 1.0, 3.2); immediate removal from play (OR: 2.4, 95% CI 1.2, 4.9); alcohol (OR: 2.6, 95% CI 1.2, 5.4), tobacco (OR: 3.3, 95% CI 1.1, 9.5), or marijuana use since injury (OR: 5.4, 95% CI 1.5, 19.0); as well as prolonged recovery due to mental health alterations (OR: 5.3, 95% CI 2.0, 14.1) or motivation/malingering (OR: 7.5, 95% CI 3.3, 17.0) increased odds of being MDQ + . The MDQ + group took longer to become asymptomatic relative to the MDQ− group (MDQ + : 23.5 days, 95% CI 15.8, 31.2; MDQ−: 10.6 days, 95% CI 9.5, 11.6; p < 0.001).
Conclusions
MDQ following concussion was relatively rare. We identified three patterns related to MDQ following concussion: (1) concussion and headache history were the only premorbid factors that differed (2) initial concussion presentation was more severe and more immediate in the MDQ + group, and (3) post-concussion recovery outcomes expressed the greatest differences between groups.


Similar content being viewed by others
Data Availability Statement
Data are available within the Federal Interagency Traumatic Brain Injury Research (FITBIR) informatics system at https://fitbir.nih.gov/.
References
Davis-Hayes C, Baker DR, Bottiglieri TS, et al. Medical retirement from sport after concussions: a practical guide for a difficult discussion. Neurol Clin Pract. 2018;8(1):40–7.
Tirabassi J, Brou L, Khodaee M, et al. Epidemiology of high school sports-related injuries resulting in medical disqualification. Am J Sports Med. 2016;44(11):2925–32.
Harmon KG, Clugston JR, Dec K, et al. American Medical Society for Sports Medicine position statement on concussion in sport. Br J Sports Med. 2019;53(4):213–25.
Cantu RC. Recurrent athletic head injury: risks and when to retire. 2003, W B SAUNDERS CO: United States. p. 593.
Sedney CL, Orphanos J, Bailes JE. When to consider retiring an athlete after sports-related conclusion. Clin Sports Med. 2011;30:189–200.
Huml MR. A Factor Structure Examination of Athletic Identity Related to NCAA Divisional Differences. J Coll Stud Dev. 2018;59(3):376–81.
Broglio SP, McCrea M, McAllister T, et al. A national study on the effects of concussion in collegiate athletes and US military service academy members: the NCAA-DoD concussion assessment, research and education (CARE) consortium structure and methods. Sports Med. 2017;47(7):1437–51.
Hoyle RH, Stephenson MT, Palmgreen P, et al. Reliability and validity of a brief measure of sensation seeking. Pers Individ Dif. 2002;32:401–14.
Broglio SP, AP Kontos, H Levin, et al. National Institute of Neurological Disorders and Stroke and Department of Defense Sport-Related Concussion Common Data Elements Version 1.0 Recommendations. J Neurotrauma. 2018;35(23):2776–2783.
Davidhizar R. The pursuit of illness for secondary gain. Health Care Superv. 1994;13(1):10–5.
Harmon KG, Drezner J, Gammons M, et al. American medical society for sports medicine position statement: concussion in sport. Clin J Sport Med. 2013;23(1):1–18.
Conley KM, Bolin DJ, Carek PJ, et al. National Athletic Trainers' Association position statement: Preparticipation physical examinations and disqualifying conditions. J Athl Train. 2014;49(1):102–20.
Welton KL, Kraeutler, MJ, Pierpoint, LA, et al. Injury recurrence among high school athletes in the United States: a decade of patterns and trends, 2005–2006 through 2015–2016. Orthop J Sports Med 6(1):2325967117745788.
Kroshus E, Baugh CM, Meehan WP, et al. Personal subjectivity in clinician discussion about retirement from sport post-concussion. Soc Sci Med. 2018;218:37–44.
Asken BM, Bauer RM, Guskiewicz KM, et al. Immediate removal from activity after sport-related concussion is associated with shorter clinical recovery and less severe symptoms in collegiate student-athletes. Am J Sports Med. 2018;46(6):1465–74.
Elbin RJ, Sufrinko A, Schatz P, et al. Removal from play after concussion and recovery time. Pediatrics. 2016;138(3):1.
Rice SM, Parker AG, Rosenbaum S, et al. Sport-related concussion and mental health outcomes in elite athletes: a systematic review. Sports Med. 2018;48(2):447.
Chaput G, Giguère J-F, Chauny J-M, et al. Relationship among subjective sleep complaints, headaches, and mood alterations following a mild traumatic brain injury. Sleep Med. 2009;10(7):713–6.
Solomon GS, Kuhn AW, Zuckerman SL. Depression as a modifying factor in sport-related concussion: a critical review of the literature. Phys Sportsmed. 2016;44(1):14–9.
Kaier E, Cromer LD, Johnson MD, et al. Perceptions of mental illness stigma: comparisons of athletes to nonathlete peers. J Coll Stud Dev. 2015;56(7):735–9.
Silver JM. Effort, exaggeration and malingering after concussion. J Neurol Neurosurg Psychiatry. 2012;83(8):836–42.
Merckelbach H, Dandachi-FitzGerald B, van Helvoort D, et al. When Patients Overreport Symptoms: More Than Just Malingering. Curr Dir Psychol Sci. 2019;28(3):321–6.
Silverberg ND, Hallam BJ, Rose A, et al. Cognitive-behavioral prevention of postconcussion syndrome in at-risk patients: a pilot randomized controlled trial. J Head Trauma Rehabil. 2013;28(4):313–22.
Acknowledgements
CARE Consortium Investigators (institution): April Hoy MS, ATC, CSCS (School of Behavioral and Applied Sciences, Azusa Pacific University). Joseph Hazzard, Jr., PhD, ATC (Department of Exercise Science, Bloomsburg University). Louise Kelly, PhD (Department of Exercise Science, California Lutheran University). Christina Master, MD (Division of Orthopedics, Children’s Hospital of Philadelphia). Justus Ortega, PhD (Department of Kinesiology & Recreation Administration, Humboldt State University). Nicholas Port, PhD (School of Optometry, Indiana University). Darren Campbell MD, Col USAF (retired) (Intermountain Sports Medicine). Steven J. Svoboda, MD, Colonel, US Army(retired) (MedStar Orthopaedic Institute). Margot Putukian, MD (Athletic Medicine, Princeton University). Sara P.D. Chrisman MD, MPH (Center for Child Health, Behavior and Development, Seattle Children’s Research Institute). Dianne Langford, PhD (Lewis Katz School of Medicine, Temple University). Gerald McGinty, PT, DPT (United States Air Force Academy). Jonathan C. Jackson MD (United States Air Force Academy). Kenneth L. Cameron, PhD, MPH, ATC, FNATA (Keller Army Hospital, United States Military Academy). Megan N. Houston, PhD, ATC (Keller Army Hospital, United States Military Academy). Adam James Susmarski, DO (Department Head Brigade Orthopaedics and Sports Medicine, United States Naval Academy). Joshua T. Goldman, MD, MBA (Departments of Family Medicine & Orthopaedic Surgery, University of California, Los Angeles). Christopher Giza, MD (Department of Pediatrics, University of California, Los Angeles). Holly Benjamin, MD (Department of Rehabilitation Medicine and Pediatrics, University of Chicago). Thomas Buckley, PhD (Department of Kinesiology & Applied Physiology, University of Delaware). Thomas Kaminski, PhD, ATC (Department of Kinesiology & Applied Physiology, University of. Delaware). Luis Feigenbaum, DPT, ATC (Department of Physical Therapy, Miller School of Medicine, University of Miami). James T. Eckner, M.D., M.S. (Department of PM&R, University of Michigan). Jason P. Mihalik, PhD, CAT(C), ATC, FACSM (Department of Exercise and Sport Science, The University of North Carolina at Chapel Hill). Scott Anderson ATC (University of Oklahoma). Anthony Kontos, PhD (Department of Orthopaedic Surgery, University of Pittsburgh). M. Alison Brooks, MD, MPH (Department of Orthopedics, University of Wisconsin, Madison). Stefan M. Duma, PhD (Institute for Critical Technology and Applied Science, Virginia Tech). Steve Rowson, PhD (Department of Biomedical Engineering and Mechanics, Virginia Tech). Christopher Miles, MD (Department of Family and Community Medicine, Wake Forest University). Laura Lintner, DO (Wake Forest School of Medicine Family Medicine, Winston Salem State University).
Author information
Authors and Affiliations
Consortia
Contributions
JDS, MLWR, and RCL contributed to the conception and design of this study. All authors contributed to the acquisition, analysis, and interpretation of data. JDS drafted the manuscript, which was then revised critically for important intellectual content by all authors. All authors granted final approval of the version to be published and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Funding
This publication was made possible, in part, with support from the Grand Alliance Concussion Assessment, Research, and Education (CARE) Consortium, funded, in part by the National Collegiate Athletic Association (NCAA) and the Department of Defense (DOD). The U.S. Army Medical Research Acquisition Activity, 820 Chandler Street, Fort Detrick MD 21702-5014 is the awarding and administering acquisition office. This work was supported by the Office of the Assistant Secretary of Defense for Health Affairs through the Psychological Health and Traumatic Brain Injury Program under Award NO W81XWH-14-2-0151. Opinions, interpretations, conclusions and recommendations are those of the author and are not necessarily endorsed by the Department of Defense (DHP funds). This manuscript was also made possible, in part, with support from the Air Force Research Laboratory’s Summer Faculty Fellowship Program.
Conflict of Interest
Julianne Schmidt, Michelle Weber Rawlins, James Clugston, Steven Broglio, Michael McCrea, and Thomas McAllister received funding from the National Collegiate Athletic Association and the Department of Defense to complete this investigation and cover travel costs related to the study. The remaining authors declare that they have no conflicts of interest.
Additional information
This article is part of a Topical Collection on The NCAA-DoD Concussion Assessment, Research and Education (CARE) Consortium.
The members of the CARE Consortium are listed in acknowledgements section.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Schmidt, J.D., Rawlins, M.L.W., Lynall, R.C. et al. Medical Disqualification Following Concussion in Collegiate Student-Athletes: Findings from the CARE Consortium. Sports Med 50, 1843–1855 (2020). https://doi.org/10.1007/s40279-020-01302-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-020-01302-y