Abstract
Background
Although cardiorespiratory fitness (CRF) in childhood and adolescence may be linked to future cardiovascular health, there is currently limited evidence for a longitudinal association.
Objectives
To provide a systematic review on the prospective association between CRF in childhood and adolescence and cardiovascular disease (CVD) risk factors at least 2 years later.
Methods
Using a systematic search of Medline, Embase, and SPORTDiscus, relevant articles were identified by the following criteria: generally healthy children and adolescents between 3 and 18 years of age with CRF assessed at baseline, and a follow-up period of ≥ 2 years. The outcome measures were CVD risk factors. We appraised quality of the included articles with STROBE and QUIPS checklists.
Results
After screening 7524 titles and abstracts, we included 38 articles, assessing 44,169 children and adolescents followed up for a median of 6 years. Eleven articles were of high quality. There was considerable heterogeneity in methodology, measurement of CRF, and outcomes, which hampered meta-analysis. In approximately half of the included articles higher CRF in childhood and adolescence was associated with lower body mass index (BMI), waist circumference, body fatness and lower prevalence of metabolic syndrome in later life. No associations between CRF in childhood and adolescence and future waist-to-hip ratio, blood pressure, lipid profile, and glucose homeostasis were observed.
Conclusion
Although about half of the included articles reported inverse associations between CRF in childhood and adolescence and future BMI, body fatness, and metabolic syndrome, evidence for other CVD risk factors was unconvincing. Many articles did not account for important confounding factors such as adiposity. Recommendations for future research include standardizing the measurement of CRF, i.e. by reporting VO2max, using standardized outcome assessments, and performing individual patient data meta-analyses.
Similar content being viewed by others
A high level of physical fitness in childhood and adolescence is associated with lower risks of future overweight, fatness, and metabolic syndrome. |
There is no convincing evidence linking a high level of physical fitness in childhood and adolescence to healthier future blood pressure, lipid profile, or glucose homeostasis. |
1 Introduction
Cardiovascular disease (CVD) remains the leading cause of death in adults worldwide [1]. While CVD often becomes clinically apparent during late adulthood, there is mounting evidence that the disease originates in early life [2,3,4,5,6]. For example, higher blood pressure in childhood predicts poorer cardiovascular health in mid-adulthood, and high body mass index (BMI) in early age reduces later cardiovascular health even further [7]. A high level of physical fitness is associated with reduction of CVD risk factors in adults [8, 9], and the American Heart Association recognizes low levels of fitness as an important risk factor for CVD [10]. However, there is limited evidence of the relation between physical fitness at a young age and CVD risk factors later in life. Potentially, physical fitness in childhood and adolescence is a useful early predictor of CVD risk factors and overall health [11].
Physical fitness comprises various entities, such as muscular strength, agility, balance, and cardiorespiratory fitness (CRF); of these CRF is most strongly associated with health outcomes [12]. The gold standard to test CRF is by exercising until voluntary exhaustion with direct measurement of the maximum volume of oxygen consumption (VO2max), and requires specialized equipment. Fortunately, many field-tests, sub-maximal tests, and even predicting equations provide reliable estimates of CRF in a wide range of settings and participants [10, 13, 14], thus making them implementable in many areas. By assessing CRF, a quantification of individual capacities of numerous body systems is provided [15, 16], and thus CRF provides a quantification of total body health.
Cross-sectional studies in children and adolescents show strong correlations of CRF with CVD risk factors [17,18,19]; however, it has been suggested that these associations could be more readily explained by a child’s adiposity [20]. It is likely that children and adolescents who are active have better CRF, but being active also directly affects adiposity [21]. Some studies have linked higher levels of physical activity (PA) to better CRF, but correlations were moderate [22, 23]. This could be explained by the fact that a large proportion of the variability in CRF is genetically determined, as seen in the heterogeneity in the response to regular exercise in individuals [24, 25]. Hence, the genetic component of CRF may affect the ability of the body to resist the effects of an unhealthy lifestyle, or to be more susceptible to the beneficial effects of regular PA, protecting against future CVD development.
Indeed, the potential health benefits of high levels of CRF in early life for cardiovascular function in later life have been demonstrated in a large number of publications. Thus far, due to the difficulties in following children and adolescents without potential risk factors into late adulthood when CVD becomes apparent, follow-up has focused on CVD risk factors. These include obesity, high blood pressure, high levels of cholesterol and triglycerides, and insulin resistance as proxies for CVD [26, 27]. Previous reviews have shown that reduced CRF is associated with higher prevalence of CVD risk factors; however, these reviews have some important limitations [12, 28, 29]. First, most evidence is based on cross-sectional studies, which makes it impossible to assess directionality. Prospective studies are more suitable to provide insight into the direction of the association, but thus far no conclusive prospective systematic review has been published. Second, some of these reviews included articles with only adults at baseline. This might interfere with the validity of the association between early life fitness and later CVD risk factors, as these risks are more prevalent in the adult population. From a preventive viewpoint, the relation between CRF in childhood and adolescence and the development of CVD risk factors is paramount. Therefore, we aimed to systematically review the current evidence for a prospective association between CRF in childhood and adolescence and CVD risk factors.
2 Methods
This review has been registered in PROSPERO (CRD42015025064). The methodology applied in this review adhered to the guidelines outlined in the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement [30].
2.1 Literature Search
A comprehensive systematic literature search was constructed with the help of a clinical librarian and performed in the databases Medline, Embase, and SPORTDiscus from inception until 23 October 2017. Key concepts derived from a scoping search using among others forward/backward citation tracking in Google Scholar and searching the WHO-ICTRP search portal, are embodied as follows in the systematic search strategy: (“Children aged 3 till 18 years” AND (“fitness” OR “cardiorespiratory tests” OR “cardiorespiratory test parameters”) AND “prospective studies”) OR “young hearts study”.
Key papers identified in the scoping search were all retrieved by the systematic search strategy. Furthermore, conference abstracts and books were filtered out when possible in the search. No other filters were used. The search syntax was adapted to the indexing terms of each database. The full search strategy is included as Electronic Supplementary Material Appendix S1.
2.2 Eligibility Criteria
Articles were included if they met the following criteria: (1) Longitudinal prospective study design with a follow-up period of ≥ 2 years; (2) participants at baseline were aged 3 up to and including 18 years (3) the study population was based on a general healthy population, irrespective of BMI; (4) physical fitness was assessed at baseline; and (5) it was an original article published in a peer-reviewed journal. There were no restrictions on type of fitness testing, i.e., objectively measured CRF, field tests, and composite tests were considered, since the aim of this review was to provide an overall estimate of the association between CRF and future CVD risk factors. There was no restriction on language; if after screening of the (English) title and abstract the article was deemed eligible, it was then translated. The outcomes measures included were confined to the following three categories: (1) anthropometry (e.g., BMI, overweight/obesity status, waist and/or hip circumference, skinfolds, percentage body fat (%BF), fat-free mass (FFM)), (2) circulatory system (e.g., systolic/diastolic blood pressure (SBP/DBP), arterial stiffness, pulse wave velocity (PWV), intima media thickness (IMT), cardiovascular events), and (3) metabolic (e.g., lipid profiles, glucose levels, insulin sensitivity, low grade infection). Also, articles reporting on the prevalence of metabolic syndrome or CVD risk scores were included.
2.3 Study Selection Process
First, two reviewers (SM and MM) independently screened titles and abstracts of the articles retrieved by the search strategy for eligibility. Second, full texts of articles were acquired. The same two reviewers independently screened the full texts of articles to determine whether to include the article based on the inclusion criteria. During both stages discrepancies were discussed, and when no consensus was reached a third reviewer (RG) made the final decision about inclusion.
2.4 Data Extraction and Assessment
Two reviewers (SM and MM) independently extracted data from the included articles using a pilot-tested standardized form. The following information was extracted: (1) study aim; (2) study design; (3) characteristics of cohort/participants at baseline; (4) characteristics of subjects with complete follow-up; (5) type of fitness test and representation of result; (6) the primary outcome of the study; (7) outcome of interest for this review and what confounders were corrected for. When data were unclear or not reported, attempts were made to contact authors. Inconsistencies in the extracted data were discussed between reviewers until consensus was reached.
Quality assessment was done independently by the same two reviewers. Based upon the STROBE quality assessment tool [31], the reporting in each article was scored as good, sufficient, or poor. Bias was assessed with the Quality In Prognostic Studies tool (QUIPS) [32]. This tool assesses the following six areas: participation, attrition, prognostic factor measurement, confounding measurement and account, outcome measurement, and analysis and reporting. Each of the potential bias domains was rated as having high, moderate, or low risk of bias. Based on both the QUIPS and STROBE score, studies were rated as indicated in Table 1. The lowest score in QUIPS or STROBE determined the overall rating. Discrepancies in quality and risk of bias assessment were discussed between reviewers until consensus was reached.
2.5 Data Synthesis
A flowchart of the included articles is presented according to the PRISMA guidelines [30] in Fig. 1. Relevant characteristics of the articles are presented in Table 2. Table 3 presents the outcomes of the risk of bias and quality assessment. Although our aim was to perform a meta-analysis and present pooled data, the heterogeneity of the included articles precluded execution of this plan. Hence, we present a narrative data-synthesis. In Table 4 a summary of the reported associations is presented per outcome and stratified per sex where possible.
3 Results
The literature search yielded a total of 9158 references (Fig. 1). After removal of duplicates there were 7524 unique references, and by screening the titles and abstracts we excluded 7178 references. Of the remaining 346 articles, 96 full texts of articles were neither retrievable from the libraries of our institutes nor from the authors. The other 173 articles were excluded due to reasons indicated in Fig. 1, most because of determinants or outcomes that were irrelevant to our aim. Eventually, 38 articles met the inclusion criteria and were used for further analyses.
3.1 Study Characteristics
All included articles reported on prospective cohorts, and there were no randomized controlled trials (RCT). A summary of the key characteristics of the included articles and the outcomes of interest is presented in Table 2.
The median number of included children and adolescents per article at baseline was N = 479, ranging from N = 48 [33] up to N = 8498 [34]. At follow-up the median number of included participants was N = 291, ranging from N = 29 [35] to N = 4878 [36]. Mean age at baseline of the participants of the included articles ranged from 5.9 years [37] up to 17.5 years old [38], with a median age of 11.3 years. Most articles studied pre-adolescen t children at baseline, i.e., younger than 12 years [37, 39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54]. In 11 articles the mean age of the included participants at baseline was 12 years or older; these children were considered adolescents [33, 35, 38, 55,56,57,58,59,60,61,62]. In the ten remaining articles both children and adolescents were included [34, 36, 63,64,65,66,67,68,69,70]. The median follow-up time was 6 years, varying from 2 years [40, 43, 46, 49, 53, 64, 70] to 25 years [35].
Physical fitness was measured in a variety of ways (Table 2). Twenty-one articles (55%) reported measured or estimated VO2max or peak oxygen uptake, either expressed as absolute values or adjusted for body mass or FFM. Of these, 11 articles reported objectively measured CRF by using a maximal exercise test with direct assessment of VO2max or peak oxygen uptake [33, 38, 39, 42,43,44,45, 51, 53, 57,58,59,60,61, 65, 70], while others used submaximal or field tests to estimate VO2max. Six articles reported the time it took to complete a certain test [33,34,35, 37, 40, 47]. The achieved level of the 20-m Multi Stage Shuttle Run Test (20 m-MSRT) was used in three articles [52, 54, 56]. Three articles used the distance covered within a pre-specified time [46, 55, 68]. A composite score of multiple health-related fitness components was used in three articles [62,63,64]. Furthermore, physical working capacity on an ergometer at heart rate 170 was used [66]. One article used various hemodynamic properties during a graded maximal fitness test [42]. CRF was expressed as a continuous measure in most articles, but in 11 articles authors categorized CRF using different cut-offs [35, 36, 38, 41, 50, 54, 62,63,64, 66, 70].
Some of the included articles reported on the same cohort; these included two articles about a cohort of Portuguese schoolchildren [63, 64]; two articles based on the Northern Ireland Young Hearts Project [54, 56]; three from the Amsterdam Growth and Health Longitudinal study [57, 58, 61]; and two based on the European Youth Heart Study [42, 59]. These articles are shown first in Table 2. We assessed these articles separately, since they included different subsamples or measured different outcomes at different times, but the reader should be aware that the included samples in these articles could overlap.
3.2 Quality Assessment
The methodical quality of articles was assessed by the STROBE and QUIPS checklists, and results are presented in Table 3. Overall, 11 articles were qualified as high quality [40, 41, 43, 51,52,53, 55, 58, 65, 66, 69], and 12 articles were of moderate quality [33,34,35, 37, 44, 54, 56, 57, 60, 61, 64, 70], which was in most cases due to unclear attrition. The remaining 15 articles were judged to be of low overall quality. The most common issue was the absence of clear descriptions about study attrition and lack of or unclear description about adjustments for confounding in analyses.
3.3 Association Between Childhood Baseline Physical Fitness and CVD Risk Factors
A summary of the associations between childhood baseline CRF and the different CVD risk factors at least 2 years later is presented in Table 4. A [+] indicates a significant association between higher baseline fitness and better health outcomes, e.g., a negative regression coefficient indicating higher fitness was associated with lower BMI. A [−] indicates a significant association between higher baseline fitness and poorer health outcomes, e.g., a positive regression coefficient indicating higher fitness was associated with higher BMI. Articles with no significant association are presented as [o]. High-quality articles are indicated by bold print in Table 4. We only included the fully adjusted models when there were multiple models reported in an article. All significant associations were in the expected direction, and most of the non-significant associations were also in the expected direction.
3.4 BMI
In boys, higher CRF was associated with healthier (lower) BMI in two out of four articles [36, 55], of which one was of high quality [55]. In girls, only Savva et al. showed that higher CRF was associated with a lower risk of being overweight [36]. Three other articles, including one high-quality article [55], showed no associations. Five articles, of which two were of high quality, found that better CRF was associated with lower BMI in both sexes combined [33, 41, 48, 64, 66], while three other articles, of which one was of high quality [51], found no associations [49, 63]. Liew et al. showed a significant association between CRF and BMI for children aged 11 years after 2 years’ follow-up, which was no longer significant at the third year of follow-up [47]. Of the three articles reporting on adolescents [33, 55, 62], higher CRF was associated with lower BMI in boys [55] and both sexes combined [33], while the other article showed no association [62]. Only one article used objectively measured VO2max, which was associated with lower BMI [33].
3.5 Waist or Hip Measurements
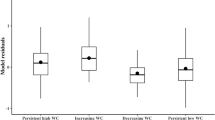
In boys, none of the articles reported a significant association between childhood CRF and waist circumference (WC) [60,61,62]. In girls, Yoonsuk et al. reported higher odds of increased WC for those in the lowest tertile of an aggregated fitness test [62]. Twisk et al. measured CRF by VO2max as absolute measure and per kg of body mass, and CRF was assessed at baseline (age 13 years) or as the average CRF between age 13 and 16 years. Girls with higher absolute VO2max between 13 and 16 years had lower WC as adults, which was not the case when CRF only at age 13 years was considered. In contrast, when VO2max per kg was used only CRF at age 13 was associated with lower adulthood WC, and a maintained exposure from 13 till 16 years was not statistically significant [61]. Two out of three articles that did not report on sex separately showed healthier WC in those with high CRF; one of these studies was of high quality [40]. Only two articles included pre-adolescents instead of adolescents; of those a high-quality article found that CRF was associated with lower WC [40], while in the other article there was no association [68]. Three articles measured CRF objectively and reported no association in boys and girls [60], while higher absolute VO2max from age 13 till 16 years and VO2max per kg at age 13 in girls was associated with lower WC [61], as was also the case in both sexes combined [33].
When waist-to-hip ratio (WHR) was the outcome of interest, one high-quality article showed no significant association between CRF and WHR for both boys and girls [55], while the high-quality article reporting on both sexes combined reported a significant inverse association [40], which was not found in a moderate-quality article [61]. Two articles included adolescents and showed no associations between CRF and WHR [55, 61]. One article used objectively measured CRF and found no association [61]. Lastly, only one high-quality article reported on waist-to-height ratio (WHtR) and showed that those with low CRF before adolescence had increased odds of high WHtR 2 years later (not shown in Table 4) [40].
3.6 Body Composition
For boys, three out of five articles showed a significant association between higher CRF and lower body fatness [54, 56, 68], and also in one high-quality article [65]. In girls, CRF was inversely associated with body fatness in three articles [54, 56, 60], while no association was found in two others including one high-quality article [65]. Out of five articles reporting on both sexes together, one high-quality article showed a significant inverse association between CRF and fat mass and %BF [53]. The other articles showed similar significant associations [33, 37, 45, 61]. In adolescents, no association was found for boys, but in girls higher CRF was associated with lower body fatness [60], and in both sexes combined higher CRF was associated with lower body fatness [33, 61]. In articles with objectively measured CRF conflicting results for boys and girls were found [60, 65], while in both sexes combined higher CRF was associated with lower body fatness [33, 45, 61], except when VO2max was expressed as absolute values instead of per kg of body mass [61].
3.7 Blood Pressure
One high-quality article reported no significant association between CRF and systolic blood pressure (SBP) for boys and girls separately [55]. For boys, two out of six articles showed a significant inverse association, which in Twisk et al. was only reported for absolute VO2max at age 13 years [61]. In girls, none of the five articles reported a significant association. In four articles that reported on both sexes combined no associations were found, except that Grontved et al. reported a significant association for one specific hemodynamic variable included in their fitness test (rate pressure product) with future SBP [33, 42, 46, 48]. All articles that separately reported on associations in boys and girls included adolescents. When findings in boys and girls were not reported separately, one article included adolescents and showed no association between CRF and SBP [33]. Three articles reported no association between objectively assessed CRF and SBP [42, 60, 61]; however, rate pressure product was found to be associated with lower SBP [42].
No high-quality articles reported on diastolic blood pressure (DBP). Two out of five articles reported a significant association in boys [35, 54]. In girls and when both sexes were combined, none of the seven articles reported a significant association between CRF and later DBP. Two articles included pre-adolescents [48, 54], of which one showed that higher CRF was associated with lower DBP in boys only [54]. Three articles showed no association of objectively measured CRF and DBP [33, 60, 61].
3.8 Lipid Profile
One high-quality article reported no significant association between higher CRF and lower total cholesterol (TC) for boys and girls separately [55]. Similar findings were reported in two other articles [56, 60]. Furthermore, for both boys and girls combined, no significant associations between CRF and TC were found in all three articles [33, 48, 61]. All but one reported on adolescents [48], and three articles used objectively measured CRF [33, 60, 61]; none reported an association between CRF and TC.
Regarding the outcome high-density lipoprotein cholesterol (HDL-C), three articles reported separately for boys and girls and found no significant associations [56, 60, 62]. For boys and girls combined also no significant associations were found in three articles [33, 52, 61], of which one was of high quality [52]. One article reported on pre-adolescents [52], and three articles used objectively measured CRF [33, 60, 61]; none reported an association between CRF and HDL-C.
When the TC:HDL ratio was the outcome of interest, in boys three out of five articles showed a significant association between a higher CRF and lower TC:HDL ratio [54, 56, 70]. However, this was only true for 15-year-olds and not 12-year-olds [56], or when VO2max was expressed per kg body mass and not per kg FFM [70]. In girls, two out of four articles found a significant inverse association; however, in Boreham et al. this was only for CRF measured at 12 years and not at 15 years old [56]. The two articles reporting on both sexes together showed no association between CRF and TC:HDL ratio. Four articles included adolescents, of which one showed disparate results between boys and girls at age 12 or 15 years [56], while the others reported no association [33, 60, 61]. Four articles objectively assessed CRF [33, 60, 61, 70], and only higher VO2max per kg of body mass in boys was associated with lower TC:HDL ratio [70].
Triglycerides (TG) were the outcome of interest in one high-quality article, and no significant associations for boys and girls separately was found [52]. Similarly, no significant associations were found for boys in the three other articles, except for Latt et al. where a significant association was reported between higher VO2max per kg body mass but not per kg of FFM and lower TG [70]. In girls, there was a significant association in one article [60], while the other article showed no association [62]. When both sexes were combined there were no significant associations in two articles [33, 46]. Three articles reported on adolescents; no associations between CRF and TG were reported in boys and both sexes combined [33, 62], while an inverse association was found in girls in one article [60]. Two articles objectively assessed CRF [33, 60]; no associations were found for boys and both sexes combined, but in girls higher CRF was associated with lower TG [60].
Lastly, CRF in pre-adolescents was not associated with low density lipoprotein cholesterol (LDL-C) in one high-quality article in the adjusted model for boys and girls separately (not shown in Table 4) [52].
3.9 Glucose Homeostasis
CRF was not associated with glucose in boys and girls separately [62], or when they were combined [33, 59]. All three articles reported on adolescents. The two articles that objectively assessed CRF found no association for both sexes [33, 59]. For the homeostatic model of insulin resistance (HOMA-IR), all articles reported on boys and girls together. Two high-quality articles showed no association between CRF and HOMA-IR [43, 66], but low CRF was associated with increased odds of belonging to the top 75th percentile of HOMA-IR [66]. High CRF was also significantly associated with lower HOMA-IR in two articles [59, 70], although this was not true for VO2max expressed per kg FFM instead of per kg body mass [70]. The other article did not show an association between CRF and HOMA-IR [46]. One article including adolescents reported that higher CRF was associated with lower HOMA-IR [59]. Three articles objectively measured CRF. One high-quality article showed no association [43], while two reported that higher CRF was associated with lower HOMA-IR [59, 70]; of these two studies, one reported an inverse association only when VO2max was expressed per kg of body mass and not per kg of FFM [70]. Furthermore, pre-adolescent CRF was not significantly associated with insulin sensitivity determined by the Matsuda index in a high-quality article [43]. However, objectively measured CRF in adolescents was significantly associated with insulin and HOMA-B (beta-cell function) for both sexes (not shown in Table 4) [59].
3.10 Metabolic Syndrome and Risks Scores
Two articles reported on the association between CRF and metabolic syndrome in boys and girls separately. One article found cut-off values of CRF predicted metabolic syndrome for boys aged 12, 13 and 14 years, and girls aged 12 and 13 years, but not for 14-year-old girls [67]. Another article only reporting on boys found no association [62]. Of the articles reporting on boys and girls combined, three showed an association between higher CRF and lower risk of metabolic syndrome [39, 50, 69], of which Schmidt et al. was of high quality [69]. Five other articles showed no association. All five articles including adolescents reported no association between CRF and the development of metabolic syndrome [33, 38, 57, 60, 62]. Objectively measured CRF was used in five articles in both sexes combined [33, 38, 39, 57, 60], of which one showed an inverse association between CRF and metabolic syndrome [33, 38, 39, 57, 60].
3.11 Other Outcomes
Two moderate- and one high-quality article reported on other outcomes, which are not shown in Table 4. No association between objectively measured CRF and left ventricular mass in pre-adolescent boys was found, but in girls peak oxygen uptake explained 35% of the variability in left ventricular mass [44]. Sun et al. assessed high sensitivity C-reactive protein (hsCRP) and fibrinogen in pre-adolescents, showing an inverse association between CRF and fibrinogen in both sexes, and with hsCRP in girls, but not in boys [34]. Finally, a high-quality article showed that out of many arterial properties, objectively measured high CRF in adolescence was associated with reduced carotid intima media thickness (IMT) in boys, and with increased femoral artery diameter and stiffness in both sexes [58].
4 Discussion
We showed that higher physical fitness, specifically CRF, during childhood and adolescence was associated with lower BMI, lower waist circumference, lower body fatness and a lower prevalence of metabolic syndrome later in life. There was no convincing evidence of an association between CRF in children and adolescents and future WHR, blood pressure, lipid profile, and glucose homeostasis. Of the articles reporting a significant association between CRF and CVD risk factors, all showed that a higher CRF was associated with lower future CVD risk factors; none of the included articles reported that higher CRF was associated with increased CVD risk factors. We therefore infer that the overall longitudinal association between CRF and CVD risk factors is probably weak to moderate. Since the most convincing evidence was found for an association between early life CRF and future adiposity, efforts to improve CRF from childhood onwards might improve the overall burden of CVD by reducing adiposity.
There are many factors affecting the variability of CRF, and a large proportion of these have a genetic origin [25]. Moderate to vigorous PA and adiposity are thought to be the largest influencers of CRF, together with sex and age [22, 71, 72]. Similarly, adiposity together with duration and intensity of PA are important factors in the development of CVD [73, 74]. Cross-sectional studies show strong correlations between CRF, PA, BMI, and CVD risk factors [17,18,19], meaning that these factors at time of outcome measurement might overshadow potential longitudinal associations. In particular, changes in body fatness greatly influence longitudinal associations of CRF with CVD risk factors. For instance, high adiposity at baseline resulted in lower fitness after 2 years, but reducing adiposity over the 2-year period resulted in CRF similar to controls [75]. In many of the included articles that adjusted for baseline adiposity, significant associations between CRF and future CVD risk factors were attenuated, e.g., Klakk et al. [46], Ortega et al. [51], and Grontved et al. [59]. Furthermore, adiposity at baseline significantly impacted performance in fitness testing, possibly because the additional energy required to move a larger body mass hampers individuals' ability to attain a similar level as their normal weight peers, and thus is a not necessarily a reflection of a lower level of cardiorespiratory functioning [76,77,78]. This could limit the ability of certain fitness (field) tests to adequately determine CRF in obese children and adolescents, and might have obscured associations between CRF and future CVD risk factors. To illustrate this, associations altered when VO2max was expressed relative to body mass instead of relative to fat-free mass [50, 70]. However, when adiposity at follow-up was taken into account, CRF was more strongly associated with future BP in one article [35]. Despite the large biological effect of adiposity on CRF and outcome measures, not all articles adjusted for this confounder, which could have reduced the reliability of the findings.
Levels of PA and CRF are not stable and decline when children grow older [79], which could be both environmentally determined and a biological effect [80]. Associations between CRF, PA, and CVD risk factors are intricate and are probably bidirectional [81, 82]. These intricate relations could be explained in terms of those with low CRF being possibly less inclined to perform PA, resulting in reduced energy expenditure and increasing adiposity [83]. However, the opposite might also be true, i.e., adipose children might be less inclined to perform PA and therefore have decreased CRF [84]. This reverse causality could explain the varying effectiveness of childhood and adolescent PA interventions in tackling obesity [85]. This complexity and other factors influencing these relations might also explain why some authors found significant associations while others did not.
4.1 Strengths and Limitations
A strength of this review is that stringent inclusion criteria were used. By only including children and adolescents aged 3–18 years at baseline our results were not obscured by adult participants. The minimum 2 years of follow-up ensured that a true longitudinal association was explored. There are also some limitations that warrant discussion, particularly regarding the merits of the individual studies that were available for this review. The included articles were heterogeneous with respect to methodology and measurement of CRF and outcomes, which hampered our intended meta-analysis. We attempted to convert effect estimates of individual articles so they could be pooled [86], or tried to select only articles reporting on VO2max, which proved futile. Although we were unable to weigh the effect estimates for each association, articles with smaller samples (e.g., below 100 participants) were among the articles that reported significant associations, thus suggesting that adequate sample sizes were included in these articles [33, 35, 45, 53]. The ambiguity in the reported associations might also have been due to selection bias. Many of the included articles had poor reporting on attrition, and only 11 articles were of high quality. Potentially, this could mean that individuals examined at follow-up were healthier or less healthy than the overall sample, which could have led to overestimated or underestimated associations. As with every systematic review, the quality of the data is dependent on the quality of the original articles and the way the data are reported.
In part, the heterogeneity of articles might explain the inconsistent findings. For instance, some of the included articles reported on boys and girls separately, while others corrected for sex in their models. The sex difference in CRF and prevalence of CVD risk factors would justify reporting separately for boys and girls [87]. Furthermore, differences in baseline age and duration of follow-up both could have interfered with whether significant associations were found, since CRF constantly changes during the life course [68, 88, 89]. Most studies and our review assessed CRF and outcomes at certain fixed times, and it would be interesting to specifically explore whether sustained high levels or improving CRF in children and adolescents resulted in lower future CVD risk factors.
4.2 Recommendations
To achieve more homogeneity in future studies some recommendations are warranted. First, a uniform measure of CRF is strongly recommended. The most feasible method to express CRF seems to be as VO2max per kg of body mass [90], since most CRF field-test results can be satisfactorily expressed as VO2max [91, 92]. Thus, reporting CRF in both absolute values and VO2max per kg of body mass would aid comparisons between studies. Second, the development of a core-outcome set would greatly benefit this field of research [93]. Third, we recommend reporting detailed information on the statistical methods and detailed output of the effect estimates, including confidence intervals or standard errors. Besides providing more insight into effect sizes, this would aid future systematic reviews in calculating standardized effect sizes to be pooled in meta-analyses [86]. Furthermore, specifics and outcomes of unadjusted and adjusted models should be reported. Fourth, to clarify attrition rates authors should adhere to reporting guidelines such as the STROBE guideline [31]. Last, since CRF and most of the outcomes of interest are age- and sex-dependent, we would recommend use of age adjusted z-scores when possible [94], and reporting on boys and girls separately, even if there were no differences in the associations found [95].
Future systematic reviews on this topic should aim to gather individual patient fitness data at baseline and outcome data at follow-up [96]. This would give the authors the ability to infer stronger conclusions and if possible adjust for potential confounders, such as adiposity [97, 98]. Unfortunately, we did not account for this during the planning of this systematic review.
5 Conclusion
We showed that higher CRF in childhood and adolescence is associated with lower BMI, body fatness, and metabolic syndrome incidence at least 2 years later. For WHR, blood pressure, lipid metabolism and glucose homeostasis the evidence is unconvincing. These findings could be hampered by confounders that were not uniformly accounted for, such as adiposity at baseline and/or follow-up. High CRF in children and adolescents was not linked to increased CVD risk factors in any of the articles. Addressing CRF in children and adolescents could reduce future adiposity and thus be an important factor in improving health. Recommendations for future research include standardizing the measurement of CRF, reporting standardized outcome assessments, and performing individual patient data meta-analyses.
References
Mendis S, Davis S, Norrving B. Organizational update: the World Health Organization Global Status Report on Noncommunicable Diseases 2014; one more landmark step in the combat against stroke and vascular disease. Stroke. 2015;46(5):e121–2. https://doi.org/10.1161/STROKEAHA.115.008097.
Juonala M, Magnussen CG, Berenson GS, Venn A, Burns TL, Sabin MA, et al. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Engl J Med. 2011;365(20):1876–85. https://doi.org/10.1056/NEJMoa1010112.
Laitinen TT, Pahkala K, Venn A, Woo JG, Oikonen M, Dwyer T, et al. Childhood lifestyle and clinical determinants of adult ideal cardiovascular health: the Cardiovascular Risk in Young Finns Study, the Childhood Determinants of Adult Health Study, the Princeton Follow-Up Study. Int J Cardiol. 2013;169(2):126–32. https://doi.org/10.1016/j.ijcard.2013.08.090.
Magnussen CG, Smith KJ, Juonala M. When to prevent cardiovascular disease? As early as possible: lessons from prospective cohorts beginning in childhood. Curr Opin Cardiol. 2013;28(5):561–8. https://doi.org/10.1097/HCO.0b013e32836428f4.
Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts). Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J. 2016;37(29):2315–81. https://doi.org/10.1093/eurheartj/ehw106.
Friedemann C, Heneghan C, Mahtani K, Thompson M, Perera R, Ward AM. Cardiovascular disease risk in healthy children and its association with body mass index: systematic review and meta-analysis. BMJ. 2012;345:e4759. https://doi.org/10.1136/bmj.e4759.
Theodore RF, Broadbent J, Nagin D, Ambler A, Hogan S, Ramrakha S, et al. Childhood to early-midlife systolic blood pressure trajectories: early-life predictors, effect modifiers, and adult cardiovascular outcomes. Hypertension. 2015;66(6):1108–15. https://doi.org/10.1161/HYPERTENSIONAHA.115.05831.
Kodama S, Saito K, Tanaka S, Maki M, Yachi Y, Asumi M, et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women a meta-analysis. JAMA. 2009;301(19):2024–35.
Blair SN, Kampert JB, Kohl HW iii, et al. Influences of cardiorespiratory fitness and other precursors on cardiovascular disease and all-cause mortality in men and women. JAMA. 1996;276(3):205–10. https://doi.org/10.1001/jama.1996.03540030039029.
Ross R, Blair SN, Arena R, Church TS, Després J-P, Franklin BA, et al. Importance of assessing cardiorespiratory fitness in clinical practice: a case for fitness as a clinical vital sign: a scientific statement from the American Heart Association. Circulation. 2016. https://doi.org/10.1161/cir.0000000000000461.
Ortega FB, Ruiz JR, Castillo MJ, Sjostrom M. Physical fitness in childhood and adolescence: a powerful marker of health. Int J Obes (Lond). 2008;32(1):1–11. https://doi.org/10.1038/sj.ijo.0803774.
Ruiz JR, Castro-Pinero J, Artero EG, Ortega FB, Sjostrom M, Suni J, et al. Predictive validity of health-related fitness in youth: a systematic review. Br J Sports Med. 2009;43(12):909–23. https://doi.org/10.1136/bjsm.2008.056499.
McNaughton L, Hall P, Cooley D. Validation of several methods of estimating maximal oxygen uptake in young men. Percept Mot Skills. 1998;87(2):575–84.
Artero EG, Espana-Romero V, Castro-Pinero J, Ortega FB, Suni J, Castillo-Garzon MJ, et al. Reliability of field-based fitness tests in youth. Int J Sports Med. 2011;32(3):159–69. https://doi.org/10.1055/s-0030-1268488.
Armstrong N. Oxford textbook of children’s sport and exercise medicine. Oxford: Oxford University Press; 2017.
Plowman SA, Smith DL. Exercise physiology for health fitness and performance. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2014.
Hurtig-Wennlof A, Ruiz JR, Harro M, Sjostrom M. Cardiorespiratory fitness relates more strongly than physical activity to cardiovascular disease risk factors in healthy children and adolescents: the European Youth Heart Study. Eur J Cardiovasc Prev Rehabil. 2007;14(4):575–81. https://doi.org/10.1097/HJR.0b013e32808c67e3.
Dencker M, Thorsson O, Karlsson MK, Linden C, Wollmer P, Andersen LB. Aerobic fitness related to cardiovascular risk factors in young children. Eur J Pediatr. 2012;171(4):705–10. https://doi.org/10.1007/s00431-011-1617-0.
Aires L, Silva P, Silva G, Santos MP, Ribeiro JC, Mota J. Intensity of physical activity, cardiorespiratory fitness, and body mass index in youth. J Phys Act Health. 2010;7(1):54–9.
Bailey DP, Savory LA, Denton SJ, Kerr CJ. The association between cardiorespiratory fitness and cardiometabolic risk in children is mediated by abdominal adiposity: the HAPPY study. J Phys Act Health. 2014. https://doi.org/10.1123/jpah.2014-0311.
Jiménez-Pavón D, Kelly J, Reilly JJ. Associations between objectively measured habitual physical activity and adiposity in children and adolescents: systematic review. Int J Pediatr Obes. 2010;5(1):3–18. https://doi.org/10.3109/17477160903067601.
Marques A, Santos R, Ekelund U, Sardinha LB. Association between physical activity, sedentary time, and healthy fitness in youth. Med Sci Sports Exerc. 2015;47(3):575–80. https://doi.org/10.1249/MSS.0000000000000426.
De Baere S, Philippaerts R, De Martelaer K, Lefevre J. Associations between objectively assessed components of physical activity and health-related fitness in 10- to 14-year-old children. J Phys Act Health. 2016;13(9):993–1001. https://doi.org/10.1123/jpah.2015-0596.
Bouchard C, Rankinen T. Individual differences in response to regular physical activity. Med Sci Sports Exerc. 2001;33(6 Suppl):S446–51 (discussion S52–3).
Bouchard C, An P, Rice T, Skinner JS, Wilmore JH, Gagnon J, et al. Familial aggregation of VO2 max response to exercise training: results from the HERITAGE family study. J Appl Physiol. 1999;87(3):1003–8.
Berry JD, Dyer A, Cai X, Garside DB, Ning H, Thomas A, et al. Lifetime risks of cardiovascular disease. N Engl J Med. 2012;366(4):321–9. https://doi.org/10.1056/NEJMoa1012848.
NHLBI. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report: National Heart, Lung, and Blood Institute (NHLBI)2011 Dec. Report No.: 1098-4275 (Electronic) 0031-4005 (Linking).
Rauner A, Mess F, Woll A. The relationship between physical activity, physical fitness and overweight in adolescents: a systematic review of studies published in or after 2000. BMC Pediatr. 2013;13(1):19.
Ruiz JR, Cavero-Redondo I, Ortega FB, Welk GJ, Andersen LB, Martinez-Vizcaino V. Cardiorespiratory fitness cut points to avoid cardiovascular disease risk in children and adolescents; what level of fitness should raise a red flag? A systematic review and meta-analysis. Br J Sports Med. 2016. https://doi.org/10.1136/bjsports-2015-095903.
Moher D. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009. https://doi.org/10.7326/0003-4819-151-4-200908180-00135.
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–9. https://doi.org/10.1016/j.ijsu.2014.07.013.
Hayden JA, van der Windt DA, Cartwright JL, Côté P, Bombardier C. Assessing bias in studies of prognostic factors. Ann Intern Med. 2013;158(4):280–6. https://doi.org/10.7326/0003-4819-158-4-201302190-00009.
Eisenmann JC, Wickel EE, Welk GJ, Blair SN. Relationship between adolescent fitness and fatness and cardiovascular disease risk factors in adulthood: the Aerobics Center Longitudinal Study (ACLS). Am Heart J. 2005;149(1):46–53.
Sun C, Magnussen CG, Ponsonby A-L, Schmidt MD, Carlin JB, Huynh Q, et al. The contribution of childhood cardiorespiratory fitness and adiposity to inflammation in young adults. Obesity (Silver Spring). 2014;22(12):2598–605.
Mikkelsson L, Kaprio J, Kautiainen H, Nupponen H, Tikkanen MJ, Kujala UM. Endurance running ability at adolescence as a predictor of blood pressure levels and hypertension in men: a 25-year follow-up study. Int J Sports Med. 2005;26(6):448–52.
Savva SC, Tornaritis MJ, Kolokotroni O, Chadjigeorgiou C, Kourides Y, Karpathios T, et al. High cardiorespiratory fitness is inversely associated with incidence of overweight in adolescence: a longitudinal study. Scand J Med Sci Sports. 2014;24(6):982–9. https://doi.org/10.1111/sms.12097.
Lopes VP, Maia JAR, Rodrigues LP, Malina R. Motor coordination, physical activity and fitness as predictors of longitudinal change in adiposity during childhood. Eur J Sport Sci. 2012;12(4):384–91.
Andersen LB, Hasselstrom H, Grontfeldt V, Hansen SE, Karsten F. The relationship between physical fitness and clustered risk, and tracking of clustered risk from adolescence to young adulthood: eight years follow-up in the Danish Youth and Sport Study. Int J Behav Nutr Phys Act. 2004;1(1):6. https://doi.org/10.1186/1479-5868-1-6.
Andersen LB, Bugge A, Dencker M, Eiberg S, El-Naaman B. The association between physical activity, physical fitness and development of metabolic disorders. Int J Pediatr Obes. 2011;6(Suppl 1):29–34. https://doi.org/10.3109/17477166.2011.606816.
Chen YC, Tu YK, Huang KC, Chen PC, Chu DC, Lee YL. Pathway from central obesity to childhood asthma. Physical fitness and sedentary time are leading factors. Am J Respir Crit Care Med. 2014;189(10):1194–203. https://doi.org/10.1164/rccm.201401-0097OC.
Ekblom OB, Bak EA, Ekblom BT. Trends in body mass in Swedish adolescents between 2001 and 2007. Acta Paediatr. 2009;98(3):519–22. https://doi.org/10.1111/j.1651-2227.2008.01154.x.
Grontved A, Brage S, Moller NC, Kristensen PL, Wedderkopp N, Froberg K, et al. Hemodynamic variables during exercise in childhood and resting systolic blood pressure levels 6 years later in adolescence: the European Youth Heart Study. J Hum Hypertens. 2011;25(10):608–14. https://doi.org/10.1038/jhh.2010.103.
Henderson M, Benedetti A, Barnett TA, Mathieu ME, Deladoey J, Gray-Donald K. Influence of adiposity, physical activity, fitness, and screen time on insulin dynamics over 2 years in children. JAMA Pediatr. 2016;170(3):227–35. https://doi.org/10.1001/jamapediatrics.2015.3909.
Janz KF, Dawson JD, Mahoney LT. Predicting heart growth during puberty: the Muscatine study. Pediatrics. 2000;105(5):E63.
Johnson MS, Figueroa-Colon R, Herd SL, Fields DA, Sun M, Hunter GR, et al. Aerobic fitness, not energy expenditure, influences subsequent increase in adiposity in black and white children. Pediatrics. 2000;106(4):E50.
Klakk H, Grøntved A, Møller NC, Heidemann M, Andersen LB, Wedderkopp N. Prospective association of adiposity and cardiorespiratory fitness with cardiovascular risk factors in healthy children. Scand J Med Sci Sports. 2014;24(4):e275–82. https://doi.org/10.1111/sms.12163.
Liew J, Xiang P, Johnson AY, Kwok OM. Effortful persistence and body mass as predictors of running achievement in children and youth: a longitudinal study. J Phys Act Health. 2011;8(2):234–43.
Martins C, Santos R, Gaya A, Twisk J, Ribeiro J, Mota J. Cardiorespiratory fitness predicts later body mass index, but not other cardiovascular risk factors from childhood to adolescence. Am J Hum Biol. 2009;21(1):121–3. https://doi.org/10.1002/ajhb.20826.
McGavock JM, Torrance BD, McGuire KA, Wozny PD, Lewanczuk RZ. Cardiorespiratory fitness and the risk of overweight in youth: the Healthy Hearts Longitudinal Study of Cardiometabolic Health. Obesity (Silver Spring). 2009;17(9):1802–7.
McMurray RG, Bangdiwala SI, Harrell JS, Amorim LD. Adolescents with metabolic syndrome have a history of low aerobic fitness and physical activity levels. Dyn Med. 2008;7:5. https://doi.org/10.1186/1476-5918-7-5.
Ortega FB, Labayen I, Ruiz JR, Kurvinen E, Loit HM, Harro J, et al. Improvements in fitness reduce the risk of becoming overweight across puberty. Med Sci Sports Exerc. 2011;43(10):1891–7. https://doi.org/10.1249/MSS.0b013e3182190d71.
Telford RD, Cunningham RB, Waring P, Telford RM, Potter JM, Hickman PE, et al. Sensitivity of blood lipids to changes in adiposity, exercise, and diet in children. Med Sci Sports Exerc. 2015;47(5):974–82.
Treuth MS, Butte NF, Sorkin JD. Predictors of body fat gain in nonobese girls with a familial predisposition to obesity. Am J Clin Nutr. 2003;78(6):1212–8.
Twisk JW, Boreham C, Cran G, Savage JM, Strain J, van Mechelen W. Clustering of biological risk factors for cardiovascular disease and the longitudinal relationship with lifestyle of an adolescent population: the Northern Ireland Young Hearts Project. J Cardiovasc Risk. 1999;6(6):355–62.
Barnekow-Bergkvist M, Hedberg G, Janlert U, Jansson E. Adolescent determinants of cardiovascular risk factors in adult men and women. Scand J Public Health. 2001;29(3):208–17.
Boreham C, Twisk J, Neville C, Savage M, Murray L, Gallagher A. Associations between physical fitness and activity patterns during adolescence and cardiovascular risk factors in young adulthood: the Northern Ireland Young Hearts Project. Int J Sports Med. 2002;23(Suppl 1):S22–6. https://doi.org/10.1055/s-2002-28457.
Ferreira I, Twisk JW, van Mechelen W, Kemper HC, Stehouwer CD. Development of fatness, fitness, and lifestyle from adolescence to the age of 36 years: determinants of the metabolic syndrome in young adults: the Amsterdam Growth and Health Longitudinal Study. Arch Intern Med. 2005;165(1):42–8.
Ferreira I, Twisk JW, Van Mechelen W, Kemper HC, Stehouwer CD, Amsterdam G, et al. Current and adolescent levels of cardiopulmonary fitness are related to large artery properties at age 36: the Amsterdam Growth and Health Longitudinal Study. Eur J Clin Invest. 2002;32(10):723–31.
Grontved A, Ried-Larsen M, Ekelund U, Froberg K, Brage S, Andersen LB. Independent and combined association of muscle strength and cardiorespiratory fitness in youth with insulin resistance and beta-cell function in young adulthood: the European Youth Heart Study. Diabetes Care. 2013;36(9):2575–81. https://doi.org/10.2337/dc12-2252.
Hasselstrom H, Hansen SE, Froberg K, Andersen LB. Physical fitness and physical activity during adolescence as predictors of cardiovascular disease risk in young adulthood. Danish Youth and Sports Study. An eight-year follow-up study. Int J Sports Med. 2002;23(Suppl 1):S27–31.
Twisk JW, Kemper HC, van Mechelen W. The relationship between physical fitness and physical activity during adolescence and cardiovascular disease risk factors at adult age. The Amsterdam Growth and Health Longitudinal Study. Int J Sports Med. 2002;23(Suppl 1):S8–14.
Yoonsuk J, YoonMyung K, Ji Eun Y, Eun Sung K, Masayo N, Ji Hye P, et al. The association of adolescent fatness and fitness with risk factors for adult metabolic syndrome: a 22-year follow-up study. J Phys Act Health. 2014;11(4):823–30.
Aires L, Andersen LB, Mendonca D, Martins C, Silva G, Mota J. A, 3-year longitudinal analysis of changes in fitness, physical activity, fatness and screen time.[Erratum appears in Acta Paediatr. 2010 Jan; 99(1):153]. Acta Paediatr. 2010;99(1):140–4. https://doi.org/10.1111/j.1651-2227.2009.01536.x.
Aires L, Mendonça D, Silva C, Gaya AR, Santos MP, Ribeiro JC, et al. A 3-year longitudinal analysis of changes in body mass index. Int J Sports Med. 2010;31(2):133–7.
Byrd-Williams CE, Shaibi GQ, Sun P, Lane CJ, Ventura EE, Davis JN, et al. Cardiorespiratory fitness predicts changes in adiposity in overweight Hispanic boys. Obesity (Silver Spring). 2008;16(5):1072–7. https://doi.org/10.1038/oby.2008.16.
Dwyer T, Magnussen CG, Schmidt MD, Ukoumunne OC, Ponsonby AL, Raitakari OT, et al. Decline in physical fitness from childhood to adulthood associated with increased obesity and insulin resistance in adults. Diabetes Care. 2009;32(4):683–7. https://doi.org/10.2337/dc08-1638.
Flouris AD, Bouziotas C, Christodoulos AD, Koutedakis Y. Longitudinal preventive-screening cutoffs for metabolic syndrome in adolescents. Int J Obes (Lond). 2008;32(10):1506–12. https://doi.org/10.1038/ijo.2008.142.
Freitas D, Beunen G, Maia J, Claessens A, Thomis M, Marques A, et al. Tracking of fatness during childhood, adolescence and young adulthood: a 7-year follow-up study in Madeira Island. Portugal. Ann Hum Biol. 2012;39(1):59–67.
Schmidt MD, Magnussen CG, Rees E, Dwyer T, Venn AJ. Childhood fitness reduces the long-term cardiometabolic risks associated with childhood obesity. Int J Obes (Lond). 2016;40(7):1134–40. https://doi.org/10.1038/ijo.2016.61.
Latt E, Maestu J, Raask T, Jurimae T, Jurimae J. Cardiovascular fitness, physical activity, and metabolic syndrome risk factors among adolescent Estonian boys: a longitudinal study. Am J Hum Biol. 2016;28(6):782–8. https://doi.org/10.1002/ajhb.22866.
Zaqout M, Vyncke K, Moreno LA, De Miguel-Etayo P, Lauria F, Molnar D, et al. Determinant factors of physical fitness in European children. Int J Public Health. 2016. https://doi.org/10.1007/s00038-016-0811-2.
Costigan SA, Eather N, Plotnikoff RC, Taaffe DR, Lubans DR. High-intensity interval training for improving health-related fitness in adolescents: a systematic review and meta-analysis. Br J Sports Med. 2015;49(19):1253–61. https://doi.org/10.1136/bjsports-2014-094490.
Juonala M, Magnussen CG, Venn A, Dwyer T, Burns TL, Davis PH, et al. Influence of age on associations between childhood risk factors and carotid intima-media thickness in adulthood clinical perspective: the Cardiovascular Risk in Young Finns Study, the Childhood Determinants of Adult Health Study, the Bogalusa Heart Study, and the Muscatine Study for the International Childhood Cardiovascular Cohort (i3C) Consortium. Circulation. 2010;122(24):2514–20.
Kavey RE, Daniels SR, Lauer RM, Atkins DL, Hayman LL, Taubert K, et al. American Heart Association guidelines for primary prevention of atherosclerotic cardiovascular disease beginning in childhood. J Pediatr. 2003;142(4):368–72.
Fairchild TJ, Klakk H, Heidemann MS, Andersen LB, Wedderkopp N. Exploring the relationship between Adiposity and fitness in young children. Med Sci Sports Exerc. 2016;48(9):1708–14. https://doi.org/10.1249/mss.0000000000000958.
Castro-Piñero J, Ortega F, Keating XD, González-Montesinos J, Sjöstrom M, Ruíz JR. Percentile values for aerobic performance running/walking field tests in children aged 6 to 17 years; influence of weight status. Nutr Hosp. 2011;26(3):572–8.
Aucouturier J, Thivel D. Cardiorespiratory fitness evaluation in obese youth. European Childhood Obesity Group, Brussels, Belgium. http://ebook.ecog-obesity.eu/wp-content/uploads/2014/12/ECOG-Obesity-eBook-Article-11.4-Cardiorespiratory-Fitness-Evaluation-in-Obese-Youth.pdf. Accessed July 2018.
Norman A-C, Drinkard B, McDuffie JR, Ghorbani S, Yanoff LB, Yanovski JA. Influence of excess adiposity on exercise fitness and performance in overweight children and adolescents. Pediatrics. 2005;115(6):e690–6.
Cooper AR, Goodman A, Page AS, Sherar LB, Esliger DW, van Sluijs EMF, et al. Objectively measured physical activity and sedentary time in youth: the International Children’s Accelerometry Database (ICAD). Int J Behav Nutr Phys Act. 2015;12:113. https://doi.org/10.1186/s12966-015-0274-5.
Metcalf BS, Hosking J, Jeffery AN, Henley WE, Wilkin TJ. Exploring the adolescent fall in physical activity: a 10-yr cohort study (EarlyBird 41). Med Sci Sports Exerc. 2015;47(10):2084–92. https://doi.org/10.1249/mss.0000000000000644.
Malina RM. Physical activity and fitness: pathways from childhood to adulthood. Am J Hum Biol. 2001;13(2):162–72.
Blair SN, Cheng Y, Holder JS. Is physical activity or physical fitness more important in defining health benefits? Med Sci Sports Exerc. 2001;33(6 Suppl):S379–99; (discussion S419–20).
Dennison BA, Straus JH, Mellits ED, Charney E. Childhood physical fitness tests: predictor of adult physical activity levels? Pediatrics. 1988;82(3):324–30.
Metcalf BS, Hosking J, Jeffery A, Voss L, Henley W, Wilkin T. Fatness leads to inactivity, but inactivity does not lead to fatness: a longitudinal study in children (EarlyBird 45). Arch Dis Child. 2010:archdischild175927.
Van Sluijs EM, McMinn AM, Griffin SJ. Effectiveness of interventions to promote physical activity in children and adolescents: systematic review of controlled trials. BMJ. 2007;335(7622):703.
Nieminen P, Lehtiniemi H, Vähäkangas K, Huusko A, Rautio A. Standardised regression coefficient as an effect size index in summarising findings in epidemiological studies. Epidemiol Biostatistics Public Health. 2013;10(4):e8854-1-e-15. https://doi.org/10.2427/8854.
Ramirez-Velez R, Palacios-Lopez A, Humberto Prieto-Benavides D, Enrique Correa-Bautista J, Izquierdo M, Alonso-Martinez A, et al. Normative reference values for the 20 m shuttle-run test in a population-based sample of school-aged youth in Bogota, Colombia: the FUPRECOL study. Am J Hum Biol. 2017. https://doi.org/10.1002/ajhb.22902.
Kaminsky LA, Imboden MT, Arena R, Myers J. Reference standards for cardiorespiratory fitness measured with cardiopulmonary exercise testing using cycle ergometry: data from the Fitness Registry and the Importance of Exercise National Database (FRIEND) registry. Mayo Clin Proc. 2017;92(2):228–33. https://doi.org/10.1016/j.mayocp.2016.10.003.
Rump P, Verstappen F, Gerver WJ, Hornstra G. Body composition and cardiorespiratory fitness indicators in prepubescent boys and girls. Int J Sports Med. 2002;23(1):50–4. https://doi.org/10.1055/s-2002-19274.
Ortega FB, Ruiz JR, Mesa JL, Gutierrez A, Sjostrom M. Cardiovascular fitness in adolescents: the influence of sexual maturation status-the AVENA and EYHS studies. Am J Hum Biol. 2007;19(6):801–8. https://doi.org/10.1002/ajhb.20640.
Castro-Pinero J, Artero EG, Espana-Romero V, Ortega FB, Sjostrom M, Suni J, et al. Criterion-related validity of field-based fitness tests in youth: a systematic review. Br J Sports Med. 2010;44(13):934–43. https://doi.org/10.1136/bjsm.2009.058321.
Batista MB, Romanzini CLP, Castro-Piñero J, Ronque ERV. Validity of field tests to estimate cardiorespiratory fitness in children and adolescents: a systematic review. Revista Paulista de Pediatria. 2017;35(2):222–33.
Kirkham JJ, Gargon E, Clarke M, Williamson PR. Can a core outcome set improve the quality of systematic reviews?—a survey of the coordinating editors of Cochrane review groups. Trials. 2013;14(1):21. https://doi.org/10.1186/1745-6215-14-21.
WHO. WHO child growth standards: length/height for age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age, methods and development. Geneva: World Health Organization; 2006. p. xx + 312 pp.
Dencker M, Thorsson O, Karlsson MK, Linden C, Eiberg S, Wollmer P, et al. Gender differences and determinants of aerobic fitness in children aged 8-11 years. Eur J Appl Physiol. 2007;99(1):19–26. https://doi.org/10.1007/s00421-006-0310-x.
Egger M, Smith GD, Phillips AN. Meta-analysis: principles and procedures. BMJ. 1997;315(7121):1533.
Simmonds MC, Higgins JP, Stewart LA, Tierney JF, Clarke MJ, Thompson SG. Meta-analysis of individual patient data from randomized trials: a review of methods used in practice. Clin Trials. 2005;2(3):209–17.
Schmid CH, Stark PC, Berlin JA, Landais P, Lau J. Meta-regression detected associations between heterogeneous treatment effects and study-level, but not patient-level, factors. J Clin Epidemiol 57(7):683–97. https://doi.org/10.1016/j.jclinepi.2003.12.001.
Author information
Authors and Affiliations
Contributions
Stijn Mintjens conceived and planned the review, wrote the protocol, assisted in development of the search strategy, screened titles, abstracts and full texts, extracted and interpreted the data and wrote the manuscript. Malou Menting contributed to writing the protocol, screened titles, abstracts and full texts, extracted and interpreted data and revised the manuscript. Joost Daams built the systematic search, assisted in retrieving articles from library databases and revised the manuscript. Mireille van Poppel contributed to drafting the protocol, interpreted data and revised the manuscript. Tessa Roseboom contributed to drafting the protocol, interpreted data and revised the manuscript. Reinoud Gemke contributed to writing the protocol, resolved conflicts during screening, interpreted data and revised the manuscript. All authors approved the final submitted manuscript.
Corresponding author
Ethics declarations
Funding
Stijn Mintjens and Malou Menting are supported by a Dutch Heart Foundation grant. (Grant no. 2013T085). No other sources of funding were used to assist in the preparation of this article.
Conflicts of interest
Stijn Mintjens, Malou Menting, Joost Daams, Mireille van Poppel, Tessa Roseboom, and Reinoud Gemke declare that they have no conflicts of interest relevant to the content of this review.
Data availability statement
The data that support the findings of this review are available on reasonable request from the corresponding author (Stijn Mintjens).
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Mintjens, S., Menting, M.D., Daams, J.G. et al. Cardiorespiratory Fitness in Childhood and Adolescence Affects Future Cardiovascular Risk Factors: A Systematic Review of Longitudinal Studies. Sports Med 48, 2577–2605 (2018). https://doi.org/10.1007/s40279-018-0974-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-018-0974-5