Abstract
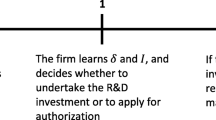
In this article, we model the behavior of a pharmaceutical firm that has marketing authorization for a new therapy believed to be a candidate for personalized use in a subset of patients, but that lacks information as to why a response is seen only in some patients. We characterize the optimal outcome-based reimbursement policy a health authority should follow to encourage the pharmaceutical firm to undertake research and development activities to generate the information needed to effectively stratify patients. Consistent with the literature, we find that for a pharmaceutical firm that does not undertake research and development activities, when the treatment fails, the total price of the drug must be returned to the healthcare system (full penalization). By contrast, if the firm undertakes research and development activities that make the implementation of personalized medicine possible, treatment failure should not be fully penalized. Surprisingly, in some cases, particularly for high-efficacy drugs and small target populations, the optimal policy may not require any penalty for treatment failure. To illustrate the main results of the analysis, we provide a numerical simulation and a graphical analysis.




Similar content being viewed by others
Notes
Implicitly, it is assumed that a physician, given the available information, prescribes the drug if the expected health benefits are positive.
Alternatively, we may think of a treatment that has been commercialized for some time, and with which we have observed the proportion of responders who are cured (\(h\pi\)), the proportion of responders not fully cured (\(h\left( {1 - \pi } \right)\)), and the proportion of non-responders (\(1 - h\)). We assume that these parameters remain constant for the population of patients with the disease.
In fact, there may be several laboratories competing in the market and offering the same test or similar tests.
The drug panitumumab together with a co-developed companion diagnostic test for patients with metastatic colorectal cancer and epidermal growth factor receptor overexpression was approved in 2006. A year later, an additional test developed by an independent diagnostic company showed that the drug was ineffective in a subset of the subpopulation. Prices did not rise to reflect the higher efficacy in the smaller selected subpopulation. See Trusheim et al. [25].
References
Redekop WK, Mladsi D. The faces of personalized medicine: a framework for understanding its meaning and scope. Value Health. 2013;16:54–9.
Antoñanzas F, Juárez-Castelló C, Rodríguez-Ibeas R. Some economics on personalized and predictive medicine. Eur J Health Econ. 2015;16(9):985–94.
Annemans L, Redekop K, Payne K. Current methodological issues in the economic assessment of personalized medicine. Value Health. 2013;16(6 Suppl.):S20–6.
Sairamesh J, Rossbach M. An economic perspective on personalized medicine. Hugo J. 2013;7(1):1–2.
Connor S. Our Drugs Do Not Work On Most Patients. The Independent (London), 13 Dec 2011. http://www.rense.com/general69/glax.htm. Accessed 6 Feb 2018.
Culbertson AW, Valentine SJ, Naylor S. Personalized medicine: technological innovation and patient empowerment or exuberant hyperbole? Drug Discov World. 2007;8(3):18–32.
Trusheim MR, Berndt ER, Douglas FL. Stratified medicine: strategic and economic implications of combining drugs and clinical biomarkers. Nat Rev Drug Discov. 2007;6(4):287–93.
Jain S, Shankaran V. The economics of personalized therapy in metastatic colorectal cancer. Curr Colorectal Cancer Rep. 2016;12:123–9.
Lièvre A, Bachet JB, Le Corre D, Boige V, Landi B, Emile JF, Côté JF, Tomasic G, Penna C, Ducreux M, Rougier P, Penault-Llorca F, Laurent-Puig P. KRAS mutation status is predictive of response to cetuximab therapy in colorectal cancer. Cancer Res. 2006;66(8):3992–5.
Behl AS, Goddard KA, Flottemesch TJ, Veenstra D, Meenan RT, Lin JS, Maciosek MV. Cost-effectiveness analysis of screening for KRAS and BRAF mutations in metastatic colorectal cancer. J Natl Cancer Inst. 2012;104(23):1785–95.
Thierry AR, Mouliere F, El Messaoudi S, Mollevi C, Lopez-Crapez E, Rolet F, Gillet B, Gongora C, Dechelotte P, Robert B, Del Rio M, Lamy PJ, Bibeau F, Nouaille M, Loriot V, Jarrousse AS, Molina F, Mathonnet M, Pezet D, Ychou M. Clinical validation of the detection of KRAS and BRAF mutations from circulating tumor DNA. Nat Med. 2014;20:430–5.
Carlson JJ, Garrison LP, Ramsey SD, Veenstra DL. The potential clinical and economic outcomes of pharmacogenomic approaches to EGFR-tyrosine kinase inhibitor therapy in non-small-cell lung cancer. Value Health. 2009;12(1):20–7.
NICE. Erlotinib and gefitinib for treating non-small-cell lung cancer that has progressed after prior chemotherapy. 2015. nice.org.uk/guidance/ta374. Accessed 9 Jan 2018.
Faulkner E, Annemans L, Garrison L, Helfand M, Holtorf AP, Hornberger J, Hughes D, Li T, Malone D, Payne K, Siebert U, Towse A, Veenstra D, Watkins J, Personalized Medicine Development and Reimbursement Working Group. Challenges in the development and reimbursement of personalized medicine: payer and manufacturer perspectives and implications for health economics and outcomes research: a report of the ISPOR Personalized Medicine Special Interest Group. Value Health. 2012;15(8):1162–71.
Carlson JJ, Chen S, Garrison LP. Performance-based risk-sharing arrangements: an updated international review. Pharmacoeconomics. 2017;35:1063–72.
Towse A, Garrison LP. Can’t get no satisfaction? Will pay for performance health? Pharmacoeconomics. 2010;28(2):93–102.
de Pouvourville G. Risk-sharing agreements for innovative drugs. Eur J Health Econ. 2006;7:155–7.
Pita-Barros P. The simple economics of risk-sharing agreements between the NHS and the pharmaceutical industry. Health Econ. 2011;20:461–70.
Zaric GS, O’Brien BJ. Analysis of a pharmaceutical risk sharing agreement based on the purchaser’s total budget. Health Econ. 2005;14:793–803.
Zaric GS, Xie B. The impact of two pharmaceutical risk-sharing agreements on pricing, promotion and net health benefits. Value Health. 2009;12(5):838–45.
Antoñanzas F, Juaréz-Castelló C, Rodríguez-Ibeas R. Should health authorities offer risk-sharing contracts to pharmaceutical firms? A theoretical approach. Health Econ Policy Law. 2011;6:391–403.
Towse A, Garrison LP. Economic incentives for evidence generation: promoting an efficient path to personalized medicine. Value Health. 2013;16(6 Suppl.):S39–43.
O’Donnell JC. Personalized medicine and the role of health economics and outcomes research: issues, applications, emerging trends, and future research. Value Health. 2013;16(6 Suppl.):S1–3.
Pita-Barros P, Martínez-Giralt X. Health economics: an industrial organization perspective. London, New York: Routledge, Taylor and Francis Group; 2012.
Trusheim MR, Burgess B, Hu SX, Long T, Averbuch SD, Flynn AA, et al. Quantifying factors for the success of stratified medicine. Nat Rev Drug Discov. 2011;10(11):817–33.
Satanove D. The challenging economics of the companion diagnostic industry; a compelling case for patent protection. J Intell Prop Ent Law. 2016;6(1):142–71.
Graf von der Schulenburg JM. Frank M. Rare is frequent and frequent is costly: rare diseases as a challenge for health care systems. Eur J Health Econ. 2015;16(2):113–8.
Acknowledgments
Financial support from MINECO (Project ECO2016-78685-R) is gratefully acknowledged. We thank Paul Overton from Beacon Medical Communications (UK) for the English editing of this manuscript. We thank the editor and two anonymous referees for their comments and suggestions.
Author information
Authors and Affiliations
Contributions
RR-I acted as a health economist on this article, developed the model analytical results, and contributed to the writing of the text. CAJ-C acted as a health economist on this article, programmed and ran the numerical simulations, and designed the figures. FA acted as a health economist on this article, conceptualized the research problem, contributed to the writing of the test, and acted as the overall guarantor for the overall content of this article. All authors contributed to the conception and planning of the work, and critically revised and approved the final submitted version of the manuscript.
Corresponding author
Ethics declarations
Funding
This study was funded by the Spanish Ministry of Economics, MINECO (Project ECO2016-78685-R).
Conflict of interest
Fernando Antoñanzas, Carmelo A. Juárez-Castelló, and Roberto Rodríguez-Ibeas have no conflicts of interest directly relevant to the content of this article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Antoñanzas, F., Rodríguez-Ibeas, R. & Juárez-Castelló, C.A. Personalized Medicine and Pay for Performance: Should Pharmaceutical Firms be Fully Penalized when Treatment Fails?. PharmacoEconomics 36, 733–743 (2018). https://doi.org/10.1007/s40273-018-0619-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-018-0619-4