Abstract
Introduction
Structural uncertainty relates to differences in model structure and parameterization. For many published health economic analyses in oncology, substantial differences in model structure exist, leading to differences in analysis outcomes and potentially impacting decision-making processes. The objectives of this analysis were (1) to identify differences in model structure and parameterization for cost-effectiveness analyses (CEAs) comparing tamoxifen and anastrazole for adjuvant breast cancer (ABC) treatment; and (2) to quantify the impact of these differences on analysis outcome metrics.
Methods
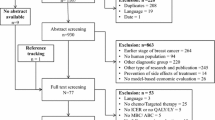
The analysis consisted of four steps: (1) review of the literature for identification of eligible CEAs; (2) definition and implementation of a base model structure, which included the core structural components for all identified CEAs; (3) definition and implementation of changes or additions in the base model structure or parameterization; and (4) quantification of the impact of changes in model structure or parameterizations on the analysis outcome metrics life-years gained (LYG), incremental costs (IC) and the incremental cost-effectiveness ratio (ICER).
Results
Eleven CEA analyses comparing anastrazole and tamoxifen as ABC treatment were identified. The base model consisted of the following health states: (1) on treatment; (2) off treatment; (3) local recurrence; (4) metastatic disease; (5) death due to breast cancer; and (6) death due to other causes. The base model estimates of anastrazole versus tamoxifen for the LYG, IC and ICER were 0.263 years, €3,647 and €13,868/LYG, respectively. In the published models that were evaluated, differences in model structure included the addition of different recurrence health states, and associated transition rates were identified. Differences in parameterization were related to the incidences of recurrence, local recurrence to metastatic disease, and metastatic disease to death. The separate impact of these model components on the LYG ranged from 0.207 to 0.356 years, while incremental costs ranged from €3,490 to €3,714 and ICERs ranged from €9,804/LYG to €17,966/LYG. When we re-analyzed the published CEAs in our framework by including their respective model properties, the LYG ranged from 0.207 to 0.383 years, IC ranged from €3,556 to €3,731 and ICERs ranged from €9,683/LYG to €17,570/LYG.
Conclusion
Differences in model structure and parameterization lead to substantial differences in analysis outcome metrics. This analysis supports the need for more guidance regarding structural uncertainty and the use of standardized disease-specific models for health economic analyses of adjuvant endocrine breast cancer therapies. The developed approach in the current analysis could potentially serve as a template for further evaluations of structural uncertainty and development of disease-specific models.


Similar content being viewed by others
References
Briggs AH, Weinstein MC, Fenwick EA, Karnon J, Sculpher MJ, Paltiel AD. Model parameter estimation and uncertainty: a report of the ISPOR-SMDM Modeling Good Research Practices Task Force–6. Value Health. 2012;15(6):835–42.
Briggs AH, Gray AM. Handling uncertainty in economic evaluations of healthcare interventions. BMJ. 1999;319(7210):635–8.
National Institute for Health and Care Excellence. Guide to the methods of technology appraisal 2013. http://publications.nice.org.uk/guide-to-the-methods-of-technology-appraisal-2013-pmg9. Accessed 3 Oct 2013.
Claxton K, Sculpher M, Drummond M. A rational framework for decision making by the National Institute for Clinical Excellence (NICE). Lancet. 2002;360(9334):711–5.
Spiegelhalter DJ, Best NG. Bayesian approaches to multiple sources of evidence and uncertainty in complex cost-effectiveness modelling. Stat Med. 2003;22(23):3687–709.
Bojke L, Claxton K, Sculpher M, Palmer S. Characterizing structural uncertainty in decision analytic models: a review and application of methods. Value Health. 2009;12(5):739–49.
Jackson CH, Bojke L, Thompson SG, Claxton K, Sharples LD. A framework for addressing structural uncertainty in decision models. Med Decis Mak. 2011;31(4):662–74.
Russell LB. Comparing model structures in cost-effectiveness analysis. Med Decis Mak. 2005;25(5):485–6.
Kim LG, Thompson SG. Uncertainty and validation of health economic decision models. Health Econ. 2010;19(1):43–55.
Forouzanfar MH, Foreman KJ, Delossantos AM, Lozano R, Lopez AD, Murray CJ, et al. Breast and cervical cancer in 187 countries between 1980 and 2010: a systematic analysis. Lancet. 2011;378(9801):1461–84.
Tamoxifen for early breast cancer: an overview of the randomised trials. Early Breast Cancer Trialists’ Collaborative Group. Lancet. 1998;351(9114):1451–67.
Annemans L. Methodological issues in evaluating cost effectiveness of adjuvant aromatase inhibitors in early breast cancer: a need for improved modelling to aid decision making. Pharmacoeconomics. 2008;26(5):409–23.
Gluck S, Gorouhi F. Clinical and economic benefits of aromatase inhibitor therapy in early-stage breast cancer. Am J Health Syst Pharm. 2011;68(18):1699–706.
Hind D, Ward S, De Nigris E, Simpson E, Carroll C, Wyld L. Hormonal therapies for early breast cancer: systematic review and economic evaluation. Health Technol Assess. 2007;11(26):iii-xi, 1.
Karnon J. Aromatase inhibitors in breast cancer: a review of cost considerations and cost effectiveness. Pharmacoeconomics. 2006;24(3):215–32.
Frederix GW, Severens JL, Hövels AM, Raaijmakers JA, Schellens JH. Reviewing the cost-effectiveness of endocrine early breast cancer therapies: influence of differences in modeling methods on outcomes. Value Health. 2012;15(1):94–105.
Frederix GW, van Hasselt JG, Severens JL, Hövels AM, Huitema AD et al. Development of a framework for cohort simulation in cost-effectiveness analyses using a multistep ordinary differential equation solver algorithm in R. Med Decis Making. 2013;33(6):780–92.
R Development Core Team. R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. http://www.R-project.org/. (2011). ISBN 3-900051-07-0.
Fonseca M, Araujo GT, Saad ED. Cost-effectiveness of anastrozole, in comparison with tamoxifen, in the adjuvant treatment of early breast cancer in Brazil. Rev Assoc Med Bras. 2009;55(4):410–5.
Gil JM, Rubio-Terres C, Del Castillo A, Gonzalez P, Canorea F. Pharmacoeconomic analysis of adjuvant therapy with exemestane, anastrozole, letrozole or tamoxifen in postmenopausal women with operable and estrogen receptor-positive breast cancer. Clin Transl Oncol. 2006;8(5):339–48.
Hillner BE. Benefit and projected cost-effectiveness of anastrozole versus tamoxifen as initial adjuvant therapy for patients with early-stage estrogen receptor-positive breast cancer. Cancer. 2004;101(6):1311–22.
Karnon J, Delea T, Barghout V. Cost utility analysis of early adjuvant letrozole or anastrozole versus tamoxifen in postmenopausal women with early invasive breast cancer: the UK perspective. Eur J Health Econ. 2008;9(2):171–83.
Locker GY, Mansel R, Cella D, Dobrez D, Sorensen S, Gandhi SK. Cost-effectiveness analysis of anastrozole versus tamoxifen as primary adjuvant therapy for postmenopausal women with early breast cancer: a US healthcare system perspective. The 5-year completed treatment analysis of the ATAC (‘Arimidex’, Tamoxifen Alone or in Combination) trial. Breast Cancer Res Treat. 2007;106(2):229–38.
Lux MP, Wockel A, Benedict A, Buchholz S, Kreif N, Harbeck N, et al. Cost-effectiveness analysis of anastrozole versus tamoxifen in adjuvant therapy for early-stage breast cancer—a health-economic analysis based on the 100-month analysis of the ATAC trial and the German health system. Onkologie. 2010;33(4):155–66.
Mansel R, Locker G, Fallowfield L, Benedict A, Jones D. Cost-effectiveness analysis of anastrozole vs tamoxifen in adjuvant therapy for early stage breast cancer in the United Kingdom: the 5-year completed treatment analysis of the ATAC (‘Arimidex’, Tamoxifen Alone or in Combination) trial. Br J Cancer. 2007;97(2):152–61.
Moeremans K, Annemans L. Cost-effectiveness of anastrozole compared to tamoxifen in hormone receptor-positive early breast cancer: analysis based on the ATAC trial. Int J Gynecol Cancer. 2006;16(Suppl 2):576–8.
Rocchi A, Verma S. Anastrozole is cost-effective vs tamoxifen as initial adjuvant therapy in early breast cancer: Canadian perspectives on the ATAC completed-treatment analysis. Support Care Cancer. 2006;14(9):917–27.
Skedgel C, Rayson D, Dewar R, Younis T. Cost-utility of adjuvant hormone therapies with aromatase inhibitors in post-menopausal women with breast cancer: upfront anastrozole, sequential tamoxifen-exemestane and extended tamoxifen-letrozole. Breast. 2007;16(3):252–61.
Skedgel C, Rayson D, Dewar R, Younis T. Cost-utility of adjuvant hormone therapies for breast cancer in post-menopausal women: sequential tamoxifen-exemestane and upfront anastrozole. Breast Cancer Res Treat. 2007;101(3):325–33.
Howell A, Cuzick J, Baum M, Buzdar A, Dowsett M, Forbes JF, et al. Results of the ATAC (Arimidex, Tamoxifen, Alone or in Combination) trial after completion of 5 years’ adjuvant treatment for breast cancer. Lancet. 2005;365(9453):60–2.
UK Office of National Statistics (2002). http://www.statistics.gov.uk/. Accessed 6 Oct 2013.
Briggs A, Sculpher M. An introduction to Markov modelling for economic evaluation. Pharmacoeconomics. 1998;13(4):397–409.
Coates AS, Keshaviah A, Thurlimann B, Mouridsen H, Mauriac L, Forbes JF, et al. Five years of letrozole compared with tamoxifen as initial adjuvant therapy for postmenopausal women with endocrine-responsive early breast cancer: update of study BIG 1-98. J Clin Oncol. 2007;25(5):486–92.
National Institute for Health and Care Excellence. Guide to the methods of technology appraisal. London: NICE, 2008. 2012.
Borner M, Bacchi M, Goldhirsch A, Greiner R, Harder F, Castiglione M, et al. First isolated locoregional recurrence following mastectomy for breast cancer: results of a phase III multicenter study comparing systemic treatment with observation after excision and radiation. Swiss Group for Clinical Cancer Research. J Clin Oncol. 1994;12(10):2071–7.
Haylock BJ, Coppin CM, Jackson J, Basco VE, Wilson KS. Locoregional first recurrence after mastectomy: prospective cohort studies with and without immediate chemotherapy. Int J Radiat Oncol Biol Phys. 2000;46(2):355–62.
Kamby C, Sengelov L. Pattern of dissemination and survival following isolated locoregional recurrence of breast cancer: a prospective study with more than 10 years of follow up. Breast Cancer Res Treat. 1997;45(2):181–92.
Moran MS, Haffty BG. Local-regional breast cancer recurrence: prognostic groups based on patterns of failure. Breast J. 2002;8(2):81–7.
Schmoor C, Sauerbrei W, Bastert G, Schumacher M. Role of isolated locoregional recurrence of breast cancer: results of four prospective studies. J Clin Oncol. 2000;18(8):1696–708.
Toonkel LM, Fix I, Jacobson LH, Wallach CB. The significance of local recurrence of carcinoma of the breast. Int J Radiat Oncol Biol Phys. 1983;9(1):33–9.
Saphner T, Tormey DC, Gray R. Annual hazard rates of recurrence for breast cancer after primary therapy. J Clin Oncol. 1996;14(10):2738–46.
Chen RC, Lin NU, Golshan M, Harris JR, Bellon JR. Internal mammary nodes in breast cancer: diagnosis and implications for patient management—a systematic review. J Clin Oncol. 2008;26(30):4981–9.
Fisher B, Jeong JH, Bryant J, Anderson S, Dignam J, Fisher ER, et al. Treatment of lymph-node-negative, oestrogen-receptor-positive breast cancer: long-term findings from National Surgical Adjuvant Breast and Bowel Project randomised clinical trials. Lancet. 2004;364(9437):858–68.
Hines SL, Vallow LA, Tan WW, McNeil RB, Perez EA, Jain A. Clinical outcomes after a diagnosis of brain metastases in patients with estrogen- and/or human epidermal growth factor receptor 2-positive versus triple-negative breast cancer. Ann Oncol. 2008;19(9):1561–5.
Haffty BG, Yang Q, Reiss M, Kearney T, Higgins SA, Weidhaas J, et al. Locoregional relapse and distant metastasis in conservatively managed triple negative early-stage breast cancer. J Clin Oncol. 2006;24(36):5652–7.
Cianfrocca M, Goldstein LJ. Prognostic and predictive factors in early-stage breast cancer. Oncologist. 2004;9(6):606–16.
Bauer KR, Brown M, Cress RD, Parise CA, Caggiano V. Descriptive analysis of estrogen receptor (ER)-negative, progesterone receptor (PR)-negative, and HER2-negative invasive breast cancer, the so-called triple-negative phenotype: a population-based study from the California Cancer Registry. Cancer. 2007;109(9):1721–8.
Haentjens P, Magaziner J, Colon-Emeric CS, Vanderschueren D, Milisen K, Velkeniers B, et al. Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med. 2010;152(6):380–90.
Afzali HH, Karnon J, Merlin T. Improving the accuracy and comparability of model-based economic evaluations of health technologies for reimbursement decisions: a methodological framework for the development of reference models. Med Decis Making. 2013;33(3):325–32.
Drummond M, Maetzel A, Gabriel S, March L. Towards a reference case for use in future economic evaluations of interventions in osteoarthritis. J Rheumatol Suppl. 2003;68:26–30.
Gabriel SE, Tugwell P, Drummond M. Progress towards an OMERACT-ILAR guideline for economic evaluations in rheumatology. Ann Rheum Dis. 2002;61(4):370–3.
Coyle D, Tosteson AN. Towards a reference case for economic evaluation of osteoporosis treatments. J Rheumatol Suppl. 2003;68:31–6.
Claret L, Gupta M, Han K, Joshi A, Sarapa N, He J, et al. Evaluation of tumor-size response metrics to predict overall survival in Western and Chinese patients with first-line metastatic colorectal cancer. J Clin Oncol. 2013;31(17):2110–4.
Friberg LE, Henningsson A, Maas H, Nguyen L, Karlsson MO. Model of chemotherapy-induced myelosuppression with parameter consistency across drugs. J Clin Oncol. 2002;20(24):4713–21.
van Hasselt JG, Gupta A, Hussein Z, Beijnen JH, Schellens JH, Huitema AD. Population pharmacokinetic-pharmacodynamic analysis for eribulin mesilate associated neutropenia. Br J Clin Pharmacol. 2013;76(3):412–24.
Committee Pharmaceutical Benefits Advisory. Guidelines for preparing submissions to the Pharmaceutical Benefits Advisory Committee. Canberra: Australian Government; 2008. p. 2013.
Garattini L, Koleva D, Casadei G. Modeling in pharmacoeconomic studies: funding sources and outcomes. Int J Technol Assess Health Care. 2010;26(3):330–3.
Jang S, Chae YK, Haddad T, Majhail NS. Conflict of interest in economic analyses of aromatase inhibitors in breast cancer: a systematic review. Breast Cancer Res Treat. 2010;121(2):273–9.
Acknowledgments
G. W. J. Frederix was a PhD student funded by an unrestricted grant from GlaxoSmithKline.
Conflict of interest
The authors declare no conflict of interest.
Author Contributions
Literature review: G. W. J. Frederix. Modelling: G. W. J. Frederix, J. G. C. van Hasselt, A. D. R. Huitema and J. L. Severens. Interpretation of outcomes: all authors. Manuscript preparation: all authors. Manuscript submission: G. W. J. Frederix. Guarantor of overall content: G. W. J. Frederix.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Frederix, G.W.J., van Hasselt, J.G.C., Schellens, J.H.M. et al. The Impact of Structural Uncertainty on Cost-Effectiveness Models for Adjuvant Endocrine Breast Cancer Treatments: the Need for Disease-Specific Model Standardization and Improved Guidance. PharmacoEconomics 32, 47–61 (2014). https://doi.org/10.1007/s40273-013-0106-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-013-0106-x