Abstract
Background
Statins have been associated with later life, long-term care admission in observational studies. However, by preventing vascular events, statins may also prevent or delay admission. We wished to determine statin and long-term care admission associations in a randomised controlled trial context, and describe associations between long-term care admission and other clinical and demographic factors.
Methods
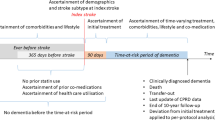
We used extended follow-up of two randomised trial populations, using national data to assign the long-term care admission outcome, and included individuals screened or recruited to two large randomised trials of pravastatin 40 mg daily—the West of Scotland Coronary Prevention Study (WOSCOPS) and the pravastatin in elderly individuals at risk of vascular disease (PROSPER) study. We described univariable and multivariable analyses of potential predictors of long-term care admission with corresponding survival curves of incident long-term care admission and analyses adjusted for competing risk.
Results
In total 11,015 (10%) of the trial participants were admitted to long-term care. There was no difference between participants in the statin or placebo arms of either trial in regard to admissions to long-term care. On multivariable analyses, independent associations with incident long-term care admission in the PROSPER trial were age (hazard ratio [HR] 1.06 per year, 95% confidence interval [CI] 1.03–1.09) and male sex (HR 0.72, 95% CI 0.53–0.99). In the WOSCOPS, age (HR 1.12 per year, 95% CI 1.10–1.13) and increasing social deprivation (HR 1.05, 95% CI 1.03–1.08) were associated with incident long-term care admission.
Conclusion
We did not demonstrate an association between historical statin use and future long-term care admission. The strongest associations with incident long-term care admission were non-modifiable factors of age, sex and socioeconomic deprivation.



Similar content being viewed by others
References
Ford I, Murray H, Packard CJ, et al. Long-term follow-up of the West of Scotland Coronary Prevention Study. N Engl J Med. 2007;357(15):1477–86.
Davies JT, Delfino SF, Feinberg CE, et al. Current and emerging uses of statins in clinical therapeutics: a review. Lipid Insights. 2016;9:13–29.
McGuinness B, Craig D, Bullock R, Passmore P. Statins for the prevention of dementia. Cochrane Database Syst Rev. 2016;(1):CD003160.
Scott D, Blizzard L, Fell J, Jones G. Statin therapy, muscle function and falls risk in community-dwelling older adults. QJM. 2009;102(9):625–33.
Salkeld G, Cameron ID, Cumming RG, et al. Quality of life related to fear of falling and hip fracture in older women: a time trade off study. BMJ. 2000;320:241–6.
Quinn TJ, McArthur K, Ellis G, Stott DJ. Functional assessment in older people. BMJ. 2011;343:d4681.
Rubin EB, Buehler AE, Halpern SD. States worse than death among hospitalized patients with serious illnesses. JAMA Intern Med. 2016;176:1557–9.
Ribbe MW, Ljunggren G, Steel K, et al. Nursing homes in 10 nations: a comparison between countries and settings. Age Ageing. 1997;26(Suppl 2):3–12.
Shepherd J, Cobbe SM, Ford I, et al. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. West of Scotland Coronary Prevention Study Group. N Engl J Med. 1995;333(20):1301–7.
Shepherd J, Blauw GJ, Murphy MB, et al. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. Lancet. 2002;360(9346):1623–30.
WOSCOPS Study Group. Screening experience and baseline characteristics in the West of Scotland Coronary Prevention Study. Am J Cardiol. 1995;76:485–91.
Ford I, Blauw GJ, Murphy MB, et al. A prospective study of pravastatin in the elderly at risk (PROSPER) screening experience and baseline characteristics. Curr Control Trials Cardiovasc Med. 2002;3:8.
Ford I, Murray H, McCowan C, Packard CJ. Long-term safety and efficacy of lowering low-density lipoprotein cholesterol with statin therapy: 20-year follow-up of West of Scotland Coronary Prevention Study. Circulation. 2016;133(11):1073–80.
The West of Scotland Coronary Prevention Study Group. A coronary primary prevention study of Scottish men aged 45–64 years: trial design. J Clin Epidemiol. 1992;45(8):849–60.
Shepherd J, Blauw GJ, Murphy MB, et al. The design of a prospective study of pravastatin in the elderly at risk (PROSPER). PROSPER Study Group. PROspective Study of Pravastatin in the Elderly at Risk. Am J Cardiol. 1999;84(10):1192–7.
Carstairs V, Morris R. Deprivation and health in Scotland. Health Bull (Edinb). 1990;48(4):162–75.
McLoone P, Boddy FA. Deprivation and mortality in Scotland, 1981 and 1991. BMJ. 1994;309(6967):1465–70.
Barry SJ, Dinnett E, Kean S, et al. Are routinely collected NHS administrative records suitable for endpoint identification in clinical trials? Evidence from the West of Scotland Coronary Prevention Study. PLoS One. 2013;8(9):e75379.
Gnjidic D, Le Couteur DG, Blyth FM, et al. Statin use and clinical outcomes in older men: a prospective population-based study. BMJ Open. 2013;3(3):e002333.
Pruchno R, Hahn S, Wilson-Genderson M. Cigarette smokers, never-smokers, and transitions: implications for successful aging. Int J Aging Hum Dev. 2012;74(3):193–209.
Harrison JK, Walesby KE, Hamilton L, et al. Predicting discharge to institutional long-term care following acute hospitalisation: a systematic review and meta-analysis. Age Ageing. 2017;46(4):547–58.
Luppa M, Luck T, Weyerer S, et al. Prediction of institutionalization in the elderly. A systematic review. Age Ageing. 2010;39(1):31–8.
Doubal FN, Ali M, Batty GD, et al. Big data and data repurposing: using existing data to answer new questions in vascular dementia research. BMC Neurol. 2017;17(1):72.
Ruscica M, Macchi C, Pavanelo C, Corsini A, Sahebkar A, Sirtoni CR. Appropriateness of statin prescription in the ederly. Eur J Intern Med. 2018;50:33–40.
Murphy C, Bennett K, Fahey T, et al. Statin use in adults at high risk of cardiovascular disease mortality: cross-sectional analysis of baseline data from The Irish Longitudinal Study on Ageing (TILDA). BMJ Open. 2015;5(7):e008017.
Lloyd SM, Stott DJ, de Craen AJ, et al. Long-term effects of statin treatment in elderly people: extended follow-up of the PROspective Study of Pravastatin in the Elderly at Risk (PROSPER). PLoS One. 2013;8(9):e72642.
Sever PS, Chang CL, Gupta AK, et al. The Anglo-Scandinavian Cardiac Outcomes Trial: 11 year mortality follow-up of the lipid lowering arm in the UK. Eur Heart J. 2011;32:2525–32.
Ridker PM, Lonn E, Paynter NP, Glynn R, Yusuf S. Primary prevention with statin therapy in the elderly. Circulaton. 2017;135:1979–81.
Acknowledgements
All contributors to this analysis are listed as authors.
Author information
Authors and Affiliations
Contributions
JKB drafted the manuscript; RP, CH, CM, IF handled the data management and analyses; and DJS and TJQ created the protocol and awarded funding. All authors contributed to interpretation of data and the final manuscript.
Corresponding author
Ethics declarations
Funding
This work was supported by the NHS Scotland, Chief Scientist Office (HICG/1/14).
Conflict of interest
Jennifer K. Burton, Richard Papworth, Caroline Haig, Colin McCowan, Ian Ford, and Terence J. Quinn declare that they have no relevant conflicts of interest that may be relevant to this manuscript. David J. Stott received research funding support from Bristol-Myers Squibb for the PROSPER and WOSCOPS studies.
Sponsor’s role
The sponsors played no part in the design, conduct or analysis of this study.
Rights and permissions
About this article
Cite this article
Burton, J.K., Papworth, R., Haig, C. et al. Statin Use is Not Associated with Future Long-Term Care Admission: Extended Follow-Up of Two Randomised Controlled Trials. Drugs Aging 35, 657–663 (2018). https://doi.org/10.1007/s40266-018-0560-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-018-0560-4