Abstract
Background
M3 muscarinic receptor antagonism has been associated with glucose intolerance and disturbance of insulin secretion.
Objective
Our objective was to examine the risk of type 2 diabetes mellitus (T2DM) in patients using antidepressants with and without M3 muscarinic receptor antagonism (AD_antaM3 and AD_nonantaM3, respectively).
Methods
We designed a case–control study using a pharmacy prescription database. We selected a cohort of patients who initiated antidepressant use between the ages of 20 and 40 years and who did not receive any anti-diabetic prescriptions at baseline. Cases were defined as those who developed T2DM [i.e., receiving oral anti-diabetic medication, Anatomical Therapeutic Chemical (ATC) code A10B] during the follow-up period (1994–2014), and ten random controls were picked for each case from the cohort of patients who did not develop T2DM.
Results
A total of 530 cases with incident T2DM and 5300 controls were included. Compared with no use of antidepressants during the previous 2 years, recent (within the last 6 months) exposure to AD_antaM3 was associated with a moderately increased risk of T2DM: adjusted odds ratio 1.55 (95% confidence interval 1.18–2.02). In the stratified analyses, this association was dose dependent (>365 defined daily doses) and significant for patients who were in the younger age group (<45 years at the end of follow-up), were female and had no co-morbidity. On the other hand, recent exposure to AD_nonantaM3 was not associated with a risk for T2DM in any of our analyses.
Conclusion
Our results suggest that exposure to AD_antaM3 was associated with the development of T2DM among antidepressant users.
Similar content being viewed by others
Antagonism of M3 muscarinic receptors (antaM3) has been related to the development of hyperglycemia. |
Recent exposure to antidepressants with antaM3 activity was associated with an increased risk for type 2 diabetes mellitus in the adult population, but exposure to antidepressants without antaM3 was not. |
This association was dose dependent and more pronounced in patients who were in the younger age group (<45 years old), were female and had no co-morbidity. |
1 Introduction
Diabetes is a group of glucose metabolism disorders leading to hyperglycemia and is classified into two main types: type 1 diabetes mellitus (T1DM) or type 2 (T2DM). T1DM results from autoimmune beta-cell destruction followed by absolute insulin deficiency, whereas T2DM is characterized by insulin resistance in peripheral tissues (muscle, fat, and liver) and a progressive decline in pancreatic beta-cell function [1].
A meta-analysis found the incidence of diabetes was significantly higher among depressed than among non-depressed subjects (0.72 vs. 0.47% yearly) [2]. Several mechanisms have been postulated for this link: eating disorders plus sedentary lifestyle induced by depressed mood, disturbance of the hypothalamic–pituitary–adrenocortical axis, disturbance of the sympathetic nervous system, dysregulation of the immune system, and the use of antidepressants [2, 3]. It is unclear whether antidepressants increase the risk for diabetes or the use of antidepressants is a proxy for depression, which can be an independent risk factor. Recent literature also offers controversial findings about the glycemic effect of antidepressants: while some studies reported a significantly increased incidence of diabetes for antidepressant users (varying from 17 to 84%) [4,5,6,7], others found no association [3, 8,9,10,11,12,13], and one paper even suggested that antidepressant treatment may prevent the onset of diabetes by normalizing the abnormal physiology induced by depression [14].
Inactivation of M3 muscarinic receptors by antipsychotics such as clozapine and olanzapine has been associated with the development of T2DM [15, 16]. It is suggested that these drugs decrease fasting plasma insulin and glucose-stimulated insulin response via their antagonism at M3 receptors in the brain and pancreas in the short term, whereas chronic treatment could lead to hyperinsulinemia, hepatic insulin resistance, and T2DM because of compensatory upregulation of M3 receptors over time [15]. It is noteworthy that some antidepressants possess an affinity at M3 muscarinic receptors (desipramine, imipramine, amitriptyline, nortriptyline, doxepin, dosulepin, maprotiline, and paroxetine) and may thus influence the risk for diabetes. We hypothesized that exposure to antidepressants with M3 antagonistic effect (AD_antaM3) might increase the risk for T2DM.
2 Methods
2.1 Design and Setting
We designed a case–control study using the Dutch pharmacy prescription database IADB (http://www.IADB.nl), a population-based database that holds the prescription records of approximately 600,000 patients in the northern Netherlands. Each record contains basic patient information (anonymous identifier, sex, date of birth) and medication information, including Anatomical Therapeutic Chemical (ATC) classification code, drug dispensing date, total amount of drugs dispensed, and dosage. Strong commitment from patients–pharmacies in the Netherlands means the prescription records for each patient in the database are nearly complete, with the exception of records of over-the-counter drugs and drugs dispensed during hospitalization [17].
2.2 Study Population
In the study period 1994–2014, we selected a cohort of patients aged 20–40 years who started taking antidepressants (ATC codes N06A* and N06CA*, not including Hyperici herba N06AX25). The cohort entry was defined as the date of the first antidepressant prescription. We included patients who received at least two antidepressant prescriptions within the year after cohort entry. This was to ensure persistent exposure and to prevent the possibility that a single prescription might not have been used by the patient.
Patients were excluded if information about the date of birth or sex was not available, if they had less than 6 months of pharmacy data before or after the cohort entry date, or if they had received an anti-diabetic prescription (ATC code A10) at or before cohort entry. Because we were interested in the risk for T2DM, patients who probably developed T1DM during follow-up (i.e., receiving only insulin) were excluded because T1DM may have a different etiology.
Cases were defined as patients who developed T2DM (i.e., receiving oral anti-diabetic medication, ATC code A10B) during the study period. The date of the first anti-diabetic medication was defined as the index date. For each case, we randomly selected up to ten control subjects (matched on birth year ±2 years, cohort entry date ±1 year, and sex) from the same cohort who were still being followed up and who had not developed diabetes. A date that resulted in the same follow-up time in a case subject was assigned to its respective control as the index date.
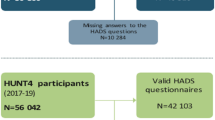
Figure 1 presents the flow diagram for the study population.
2.3 Exposure Definition
We first identified all antidepressants used by the study population. We classified them based on their antagonistic activity at M3 muscarinic receptors (antaM3) using the lists from DrugBank [36] and the IUPHAR/BPS Guide to Pharmacology [37] [see Table S1 in the Electronic Supplementary Material (ESM) for details]. There were eight AD_antaM3: desipramine, imipramine, amitriptyline, nortriptyline, doxepin, dosulepin, maprotiline, and paroxetine. The remaining antidepressants that did not antagonize M3 receptors (AD_nonantaM3) were clomipramine, opipramol, trimipramine, fluoxetine, citalopram, sertraline, fluvoxamine, escitalopram, phenelzine, tranylcypromine, moclobemide, mianserin, trazodone, nefazodone, mirtazapine, bupropion, venlafaxine, duloxetine, and agomelatine.
We categorized exposure to antidepressants as “recent”, “former”, or “past” use. Recent use was defined as a prescription that lasted into 6 months before the index date (because a previous study [7] found this window of antidepressant exposure to be associated with an increased risk for diabetes); former use was defined as a prescription that lasted into the period from 2 years to 6 months before the index date, and past use was a prescription that ended more than 2 years before the index date with no new prescription filled until the index date. In patients recently exposed to antidepressants, we further categorized their exposure into subgroups: combination (AD_antaM3 and AD_nonantaM3), AD_antaM3 only, and AD_nonantaM3 only.
2.4 Covariates
Co-medications were included as study covariates and comprised benzodiazepines and drugs that have been documented to disturb glucose homeostasis: beta-blockers, thiazide diuretics, systemic corticosteroids, calcineurin inhibitors, and antipsychotics [18]. To be considered co-medications, these drugs had to have been used in the previous 6 months before the index date. Although the hyperglycemic effect of benzodiazepines is unknown, we considered them co-medications because they are primarily prescribed for psychosocial complaints that have been associated with diabetes [3]. Given that (1) many antipsychotics are well-known for their antaM3 [15], (2) the US FDA has issued a special warning about the diabetogenic risk of antipsychotic agents, and (3) higher percentages of cases were exposed to antipsychotics than were controls (Table 1), this could influence our findings if antaM3 is associated with the risk for T2DM. We therefore excluded patients with a concurrent use of antipsychotics in subsequent analyses (see Sect. 2.5).
2.5 Statistical Analysis
We used SPSS 22.0 for Windows (IBM Corp., Armonk, NY, USA) to perform the analyses.
The following descriptive statistics were used to describe the study population: age at index date, sex, follow-up time, comorbidities, and co-medications. We considered cardiovascular diseases and dyslipidemia as comorbidities and used the drugs dispensed in the year preceding their index date as a proxy for these diseases [19]. Cardiovascular comorbidities were defined as patients exposed to the following drugs: cardiac therapy ATC code C01*, antihypertensives C02*, diuretics C03*, beta blockers C07*, calcium channel blockers C08*, agents acting on the rennin–angiotensin systems C09*, and antithrombotic agents B01*. Dyslipidemia comorbidities were defined as patients exposed to lipid-modifying agents (C10*). A p value <0.05 was considered statistically significant.
Past use was considered the reference category in all our analyses. To account for the inter-dependency between a case and its matched controls, a conditional logistic regression was used to calculate the odds ratios (ORs) and 95% confidence intervals (CIs) of developing T2DM in patients with former use and recent use of antidepressants (including the antidepressant combination, AD_antaM3 only, and AD_nonantaM3 only). We also calculated the risk for T2DM in the presence and absence of antipsychotic co-medication.
Since the persistency of the effect of AD_antaM3 (if any) is unknown, we undertook sensitivity analyses on other time windows of recent use (i.e., previous 3 months, previous 1 month, and currently being treated) to examine whether the results changed notably.
We also performed stratified analyses to examine whether the association with T2DM was modified by the patients’ characteristics, including age at index date, sex, and comorbidities. Only a few patients were exposed to the antidepressant combination (both AD_antaM3 and AD_nonantaM3), so this subgroup was not included in the stratified analyses.
To investigate the dose–response relationship between antidepressant use and new-onset T2DM, we calculated the cumulative defined daily dose (DDD; defined by the World Health Organization as “the assumed average maintenance dose per day for a drug used for its main indication in adults” [38]) that recent users had been prescribed from their starting point to the index date. If patients had used antidepressants (either AD_antaM3 or AD_nonantaM3) continuously since cohort entry, the starting point would be their cohort entry date. If patients had stopped using antidepressants for more than 6 months (discontinuation) and then restarted, the starting point would be the date of first antidepressant prescription after the discontinuation period. We used DDD as a dose standard unit for various antidepressants. The cumulative DDDs were calculated as the number of DDDs per day multiplied by the number of days (duration) the patients had been continuously using the drugs. We chose the cut-off values of ≤180 DDDs, 181–365 DDDs, and >365 DDDs to examine the dose–response relationship of the antidepressant subgroups.
We adjusted for covariates in the regression models. To limit statistical instability, we did not calculate ORs if there were fewer than five cases or controls per exposure category.
3 Results
The study population included 530 cases with new-onset diabetes and 5300 matching controls. Their characteristics are shown in Table 1. The mean follow-up period was 7.8 [standard deviation (SD) 4.7] years.
Our matching criteria ensured characteristics such as age, sex, and follow-up time were similar for cases and controls (Table 1). The majority of patients developed T2DM before the age of 45 years. At the index date, the oldest patients were aged 56.7 and 58.4 years in the case and control groups, respectively. The diabetic cases were more likely to have a comorbidity (i.e., cardiovascular diseases and/or dyslipidemia) preceding the occurrence of T2DM. They were also more likely to have received medications associated with psychosocial problems (i.e., benzodiazepines) or with hyperglycemia (i.e., beta blockers, thiazide diuretics, systemic corticosteroids, or antipsychotics). Only a few patients received calcineurin inhibitors (and exposure rates were similar in the case and control groups), so we did not adjust for this covariate in further regression models.
When we considered antidepressant users (Table 1), patients with past use of antidepressants were significantly older than other users at the index date. However, comorbidities were more prevalent among recent users. For the antidepressant subgroups, patients with past or recent use of AD_nonantaM3 had a significantly longer follow-up time than recent users of AD_antaM3 (9.1 and 7.7 vs. 6.7 years, respectively). Antipsychotics were more frequently used by patients with AD_nonantaM3 and by patients with the antidepressant combination.
Table 2 shows that the majority of exposed cases were from the past and recent use categories. Incident T2DM was associated with recent use of antidepressants but not with former use in the multivariate-adjusted regression model. Results for the four time windows (i.e., previous 6 months, previous 3 months, previous 1 month, and currently being treated) were similar. All showed a significantly increased albeit moderate risk of T2DM in recent AD_antaM3 users (OR approximately 1.50), but not in AD_nonantaM3 users. Therefore, it was reasonable to select the window of previous 6 months for further analyses.
It is worth noting that, in Table 2, ORs were reduced in patients with no concurrent use of antipsychotics; therefore, patient use of antipsychotics might influence our findings. To examine the role of AD_antaM3 and AD_nonantaM3 in T2DM development, we further excluded patients with antipsychotic comedication (86 cases and 320 controls) in the subsequent analyses.
On examining patients’ records for characteristics that predicted the risk for T2DM (Fig. 2), we found an elevated risk of T2DM with AD_antaM3 exposure in patients who were aged <45 years at the index date (OR 1.70; 95% CI 1.19–2.42), were female (OR 1.71; 95% CI 1.20–2.44), and had no prevalent comorbidity (OR 1.74; 95% CI 1.16–2.63). In contrast, exposure to AD_nonantaM3 was not associated with a risk for T2DM in any strata.
Risk of type 2 diabetes in patients with ‘recent use’ of antidepressants (excluding patients with concurrent use of antipsychotics), stratified by patients’ characteristics. AD_antaM 3 Antidepressants that antagonize M3 muscarinic receptors; AD_nonantaM 3 Antidepressants that do not antagonize M3 muscarinic receptors; OR Odds ratio; CI Confidence interval
Table 3 demonstrates a relationship between the dosing regimens of AD_antaM3 and the development of T2DM. We found that the increased use of AD_antaM3 was significantly associated with T2DM (>365 DDDs: OR 1.57; 95% CI 1.12–2.19), whereas lower dosing regimens of AD_antaM3 and any use of AD_nonantaM3 showed no association.
4 Discussion
We examined the risk of T2DM in patients exposed to antidepressants from a mechanism-based point of view. Antidepressants were grouped according to their antaM3 effect. The results showed that recent exposure to AD_antaM3 significantly increased the risk of new-onset T2DM by 50% but former use of antidepressants had no effect. However, the increased risk with AD_antaM3 had a moderate magnitude and was associated with a higher dosing regimen (>365 DDDs). On the other hand, recent exposure to AD_nonantaM3 was not associated with T2DM development at any dose.
The literature suggests an increased incidence of T2DM in people aged >45 years [20], which may be due to a weakening of the antioxidant defense system with aging [21]. While previous studies about the risk of T2DM among antidepressant users [3,4,5,6,7,8,9,10,11,12,13, 22] focused on the adult population and had no upper age limit, our study selected a fairly young cohort who initiated antidepressants between the age of 20–40 years and, by the end of the follow-up, developed T2DM before the age of 60 years. In agreement with previous studies that found a positive association between antidepressants and T2DM in the younger age group (<45 years) [5] and in females [9], our stratification analyses revealed similar findings for AD_antaM3 users but not for AD_nonantaM3 users. Although we and other authors [5, 7] noted a higher prevalence of comorbidities (cardiovascular diseases and dyslipidemia) among diabetic cases, their relationship with T2DM is still unclear. It has been suggested that these comorbidities may share a common genetic pathway with T2DM [23] or result from the use of antidepressants [24]. If this is true, patients with these comorbidities might have an increased risk for T2DM, and this could influence our findings. When we examined the group of patients without comorbidities, the association with T2DM remained for AD_antaM3 users but not for AD_nonantaM3 users. This strengthens our hypothesis that AD_antaM3 is associated with a risk for T2DM.
When the sensitivity analyses were performed for different time windows of exposure, the effect magnitude did not change. We therefore believe that our choice of a 6-month recent window was justified. Our reference group included patients with a past use of antidepressants who had a longer follow-up than patients recently treated with AD_antaM3. If follow-up time had any influence on the incidence of T2DM, it would lead to a decrease (rather than an increase) in the effect magnitude of AD_antaM3. Therefore, the association between AD_antaM3 and T2DM remains valid.
Although the risk of T2DM has been widely studied in antidepressant users [3,4,5,6,7,8,9,10,11,12,13, 22], only a few publications [4, 5, 7, 9] examined the types of antidepressants, and only Andersohn et al. [7] specified this risk for individual antidepressants. However, Andersohn et al. [7] did not take the antaM3 mechanism into account and thus did not exclude patients with antipsychotic co-medication as we did. In addition, we applied stricter inclusion criteria for the study population (i.e., ages 20–40 years at cohort entry date and receiving at least two prescriptions within a year after cohort entry) than did Andersohn et al. [7]. To examine the risk of T2DM in individual antidepressants, we only considered the exposure to a single antidepressant and thus additionally excluded patients who received two or more different antidepressants within the previous 6 months (except for those receiving amitriptyline and/or nortriptyline and those receiving citalopram and/or escitalopram because of the relation between these compounds, i.e., nortriptyline is the metabolite of amitriptyline and escitalopram is the S-enantiomer of citalopram). Adopting such criteria meant we only had a limited number of patients left for our analysis (Table S2 in the ESM). Andersohn et al. [7] found a borderline increased risk with amitriptyline, fluvoxamine, and paroxetine and the highest risk with venlafaxine. Our study also found a modestly increased risk with amitriptyline and/or nortriptyline. In contrast, venlafaxine and fluvoxamine, which were classified as AD_nonantaM3, had lower exposure rates in cases than in controls. In agreement with the results of Andersohn at al. [7], we found the exposure rate to paroxetine was 18% higher in cases than in controls. However, this difference did not reach significance in our study. Possible explanations include the limited number of patients and the very low affinity towards M3 muscarinic receptors of paroxetine compared with other AD_antaM3 (amitriptyline had the highest affinity) [25]. Increasing exposure to paroxetine (i.e., by combining with pravastatin) has been shown to increase the risk for T2DM [26,27,28]. However, we could not examine the paroxetine–pravastatin combination because it was used by only three cases. Interestingly, paroxetine is a unique antidepressant with an antioxidant property that, paradoxically, mitigates the hyperglycemic adverse effect [29].
We examined antaM3 as the antidepressant mechanism that increased the risk for T2DM. Other mechanisms are also proposed in the literature. For example, because serotonin is involved in glucose homeostasis, and most antidepressants (except for agomelatine and bupropion) act by increasing the neurotransmission of serotonin [13,14,15], use of antidepressants may alter the regulation of glucose and subsequently increase the risk for T2DM [16]. However, an examination of AD_nonantaM3 with serotonin effect (excluding agomelatine and bupropion) found no association with incident T2DM (Table S3 in the ESM). Another mechanism is antagonism of the 5-HT2C receptors, which can lead to weight gain and subsequent insulin resistance [16], although this effect is expected to be minor [17]. In addition, activities of 5-HT2A receptors (either agonism or antagonism) have been involved in insulin secretion and insulin resistance, but experimental studies [30,31,32] reported inconsistent findings. No antidepressants with 5-HT2A activation effects were used by our study population. Among antidepressants with 5-HT2A/5-HT2C antagonism, four were classified in the AD_antaM3 subgroup (imipramine, amitriptyline, nortriptyline, and doxepin) and five in the AD_nonantaM3 subgroup (clomipramine, amoxapine, mianserin, nefazodone, mirtazapine). However, we found no increased risk of T2DM in patients using AD_nonantaM3 with 5-HT2A/5-HT2C antagonism (Table S2 in the ESM).
An alternative explanation for the association between AD_antaM3 and T2DM is the presence and/or severity of depression, which is also a risk factor for T2DM [8, 12]. However, confounding by indication was unlikely in this study, based on findings from the other exposure subgroup, AD_nonantaM3. On the one hand, recent use of AD_nonantaM3 suggested the prevalence of depressive symptoms. On the other hand, given Table 1, AD_nonantaM3 users had a significantly longer follow-up time than AD_antaM3 users (7.7 vs. 6.7 years, post hoc analysis p < 0.001). This implies that AD_nonantaM3 did not relate to initial treatment of depression in our study population and that users of AD_nonantaM3 were not likely to have a shorter duration of depression or less severe symptoms than AD_antaM3 users. Since recent use of AD_antaM3 increased the risk for T2DM but recent use of AD_nonantaM3 did not, none of our analyses suggest the association of AD_antaM3 with T2DM was affected by the presence and/or severity of depression.
We used a large prescription database representative of the Dutch population with proven high accuracy and the possibility of tracking patients over time even when patients receive their medications from different pharmacies [17, 33]. Both antidepressant exposure and new-onset T2DM were recorded prospectively, so results were not affected by recall bias. Therefore, this database is suitable for our current study design, which requires a large sample size with matching conditions and a long follow-up time.
However, our study does have some limitations. First, we do not know whether patients actually took the drugs. If patients had poor compliance due to their mental status (e.g., being depressed), this could lead to an overestimation of exposure. However, if compliance was poor, it would be expected to have the same effect direction in both the case and the control groups and in the subgroups of antidepressant users. Second, since the definition of T2DM (the outcome) was based on the use of oral anti-diabetic medications, potential T2DM cases might have been missed if they were undiagnosed, were managed solely with lifestyle therapy (diet and exercise), or were initially treated with insulin because of impaired renal function. To account for the first and second instances, we conducted an additional sensitivity analysis comparing patients who used AD_antaM3 or AD_nonantaM3 continuously for more than 1 year (without discontinuation) with past users. The 1-year window of continuous use allowed more exposure time for a diabetic case to be detected and for detection of patients initially treated with lifestyle therapy. This could improve detection of lifestyle therapy because, for most patients with T2DM, this treatment will be insufficient within the first year and then pharmacologic therapy should be started [34]. In this additional analysis, the risk for T2DM remained significantly increased for AD_antaM3 users but not for AD_nonantaM3 users [adjusted OR 1.44 (95% CI 1.04–1.99) vs. 0.97 (95% CI 0.69–1.37)]. In the third instance, our study selected a rather young cohort (as previously mentioned), and therefore a severe reduction in kidney function was unlikely (it should be noted that metformin is the first-line therapy for T2DM and is contraindicated in markedly impaired renal function, i.e., estimated glomerular filtration rate <30 ml/min [35]). Although the glycated hemoglobin (HbA1c) values of patients were not available, given the above approach we believe the number of undetected T2DM cases (if any) was not particularly substantial. Finally, the database did not record patient lifestyle factors such as smoking, body mass index, and obesity, which may be related to insulin resistance. This should not lessen our findings because (1) our study was designed with a random matching method, in which cases and controls originated from one large cohort (26,475 antidepressant users), which would smooth the problem of any unequally distributed risk factors; (2) we used cardiovascular diseases and dyslipidemia as a proxy for obesity, and still found an effect of AD_antaM3 in the stratification analyses; (3) it is possible that depressed patients might have eating disorders and sedentary lifestyles that could result in overweight/obesity and enhance their susceptibility to T2DM; however, this effect would be expected to have the same impact in both the case and the control groups and in the subgroups of antidepressant users; and, finally, (4) our findings about AD_antaM3 were strengthened by detecting a dose–response relationship with the increased risk of T2DM at >365 DDDs.
5 Conclusions
We found exposure to AD_antaM3 to be associated with a moderately increased risk of new-onset T2DM. This increased risk was seen in patients who aged <45 years at the index date, were female, had no comorbidities, and were exposed to a higher dosing regimen (>365 DDDs). In contrast, the use of AD_nonantaM3 was not associated with T2DM in any analyses. Based on the results from the two treatment subgroups (AD_antaM3 vs. AD_nonantaM3), we suggest that antagonism of M3 muscarinic receptors has an important role in the development of T2DM among users of antidepressants. Further large population-based studies to confirm our findings are warranted.
References
Ergun-Longmire B, Maclaren NK. Etiology and pathogenesis of diabetes mellitus in children. In: De Groot LJ, Beck-Peccoz P, Chrousos G, et al., editors. Endotext. South Dartmouth: MDText.com, Inc.; 2000.
Rotella F, Mannucci E. Depression as a risk factor for diabetes: a meta-analysis of longitudinal studies. J Clin Psychiatry. 2013;74(1):31–7.
Knol MJ, Geerlings MI, Egberts AC, Gorter KJ, Grobbee DE, Heerdink ER. No increased incidence of diabetes in antidepressant users. Int Clin Psychopharmacol. 2007;22(6):382–6.
Pan A, Sun Q, Okereke OI, Rexrode KM, Rubin RR, Lucas M, et al. Use of antidepressant medication and risk of type 2 diabetes: results from three cohorts of US adults. Diabetologia. 2012;55(1):63–72.
Wu CS, Gau SS, Lai MS. Long-term antidepressant use and the risk of type 2 diabetes mellitus: a population-based, nested case–control study in Taiwan. J Clin Psychiatry. 2014;75(1):31–8 (quiz 8).
Vimalananda VG, Palmer JR, Gerlovin H, Wise LA, Rosenzweig JL, Rosenberg L, et al. Depressive symptoms, antidepressant use, and the incidence of diabetes in the Black Women’s Health Study. Diabetes Care. 2014;37(8):2211–7.
Andersohn F, Schade R, Suissa S, Garbe E. Long-term use of antidepressants for depressive disorders and the risk of diabetes mellitus. Am J Psychiatry. 2009;166(5):591–8.
Atlantis E, Browning C, Sims J, Kendig H. Diabetes incidence associated with depression and antidepressants in the Melbourne Longitudinal Studies on Healthy Ageing (MELSHA). Int J Geriatr Psychiatry. 2010;25(7):688–96.
Khoza S, Barner JC, Bohman TM, Rascati K, Lawson K, Wilson JP. Use of antidepressant agents and the risk of type 2 diabetes. Eur J Clin Pharmacol. 2012;68(9):1295–302.
Bhattacharya R, Ajmera M, Bhattacharjee S, Sambamoorthi U. Use of antidepressants and statins and short-term risk of new-onset diabetes among high risk adults. Diabetes Res Clin Pract. 2014;105(2):251–60.
Chang KJ, Hong CH, Lee Y, Lee KS, Roh HW, Back JH, et al. Effect of psychotropic drugs on development of diabetes mellitus in patients with Alzheimer’s disease. Medicine (Baltimore). 2015;94(23):e919.
Campayo A, de Jonge P, Roy JF, Saz P, de la Camara C, Quintanilla MA, et al. Depressive disorder and incident diabetes mellitus: the effect of characteristics of depression. Am J Psychiatry. 2010;167(5):580–8.
Sambamoorthi U, Ma Y, Findley PA, Rust G. Antidepressant use, depression, and new-onset diabetes among elderly Medicare beneficiaries. J Diabetes. 2013;5(3):327–35.
McIntyre RS, Soczynska JK, Konarski JZ, Kennedy SH. The effect of antidepressants on glucose homeostasis and insulin sensitivity: synthesis and mechanisms. Expert Opin Drug Saf. 2006;5(1):157–68.
Weston-Green K, Huang XF, Deng C. Second generation antipsychotic-induced type 2 diabetes: a role for the muscarinic M3 receptor. CNS Drugs. 2013;27(12):1069–80.
Jindal RD, Keshavan MS. Critical role of M3 muscarinic receptor in insulin secretion: implications for psychopharmacology. J Clin Psychopharmacol. 2006;26(5):449–50.
Visser ST, Schuiling-Veninga CC, Bos JH, de Jong-van den Berg LT, Postma MJ. The population-based prescription database IADB.nl: its development, usefulness in outcomes research and challenges. Expert Rev Pharmacoecon Outcomes Res. 2013;13(3):285–92.
Rehman A, Setter SM, Vue MH. Drug-induced glucose alterations. Part 2: drug-induced hyperglycemia. Diabetes Spectr. 2011;24(4):234.
Von Korff M, Wagner EH, Saunders K. A chronic disease score from automated pharmacy data. J Clin Epidemiol. 1992;45(2):197–203.
Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27(5):1047–53.
Okoduwa SI, Umar IA, Ibrahim S, Bello F, Habila N. Age-dependent alteration of antioxidant defense system in hypertensive and type-2 diabetes patients. J Diabetes Metab Disord. 2015;14:32.
Demakakos P, Pierce MB, Hardy R. Depressive symptoms and risk of type 2 diabetes in a national sample of middle-aged and older adults: the English longitudinal study of aging. Diabetes Care. 2010;33(4):792–7.
Chan KH, Huang YT, Meng Q, Wu C, Reiner A, Sobel EM, et al. Shared molecular pathways and gene networks for cardiovascular disease and type 2 diabetes mellitus in women across diverse ethnicities. Circ Cardiovasc Genet. 2014;7(6):911–9.
Chokka P, Tancer M, Yeragani VK. Metabolic syndrome: relevance to antidepressant treatment. J Psychiatry Neurosci. 2006;31(6):414.
Stanton T, Bolden-Watson C, Cusack B, Richelson E. Antagonism of the five cloned human muscarinic cholinergic receptors expressed in CHO-K1 cells by antidepressants and antihistaminics. Biochem Pharmacol. 1993;45(11):2352–4.
An L, Ravindran PP, Renukunta S, Denduluri S. Co-medication of pravastatin and paroxetine—a categorical study. J Clin Pharmacol. 2013;53(11):1212–9.
Gooden KM, Bibeau KB, Wood J, Irizarry MC, Pan X, Allen J, et al. Incidence of type 2 diabetes among patients exposed to the combination of pravastatin and paroxetine. Curr Drug Saf. 2015;10(2):152–8.
Li F, Zhang M, Xu D, Liu C, Zhong ZY, Jia LL, et al. Co-administration of paroxetine and pravastatin causes deregulation of glucose homeostasis in diabetic rats via enhanced paroxetine exposure. Acta Pharmacol Sin. 2014;35(6):792–805.
Gero D, Szoleczky P, Suzuki K, Modis K, Olah G, Coletta C, et al. Cell-based screening identifies paroxetine as an inhibitor of diabetic endothelial dysfunction. Diabetes. 2013;62(3):953–64.
Hamada K, Yoshida M, Isayama H, Yagi Y, Kanazashi S, Kashihara Y, et al. Possible involvement of endogenous 5-HT in aggravation of cerulein-induced acute pancreatitis in mice. J Pharmacol Sci. 2007;105(3):240–50.
Guenette MD, Giacca A, Hahn M, Teo C, Lam L, Chintoh A, et al. Atypical antipsychotics and effects of adrenergic and serotonergic receptor binding on insulin secretion in-vivo: an animal model. Schizophr Res. 2013;146(1–3):162–9.
Bennet H, Balhuizen A, Medina A, Dekker Nitert M, Ottosson Laakso E, Essen S, et al. Altered serotonin (5-HT) 1D and 2A receptor expression may contribute to defective insulin and glucagon secretion in human type 2 diabetes. Peptides. 2015;71:113–20.
Schirm E, Tobi H, de Jong-van den Berg LT. Identifying parents in pharmacy data: a tool for the continuous monitoring of drug exposure to unborn children. J Clin Epidemiol. 2004;57(7):737–41.
McCulloch DK. Initial management of blood glucose in adults with type 2 diabetes mellitus. UpToDate® 2017. https://www.uptodate.com/contents/initial-management-of-blood-glucose-in-adults-with-type-2-diabetes-mellitus. Accessed 31 Mar 2017.
McCulloch DK. Metformin in the treatment of adults with type 2 diabetes mellitus. UpToDate® 2017. https://www.uptodate.com/contents/metformin-in-the-treatment-of-adults-with-type-2-diabetes-mellitus. Accessed 31 Mar 2017.
The Metabolomics Innovation Centre. DrugBank. Muscarinic acetylcholine receptor M3. https://www.drugbank.ca/biodb/polypeptides/P20309. Accessed 31 Mar 2017.
Birdsall NJM, Brown DA, Buckley NJ, et al. Acetylcholine receptors (muscarinic): M3 receptor. IUPHAR/BPS guide to pharmacology. http://www.guidetopharmacology.org/GRAC/ObjectDisplayForward?objectId=15. Accessed 05 Aug 2015.
World Health Organization Collaborating Centre for Drug Statistics Methodology, Norwegian Institute of Public Health. DDD: definition and general considerations. http://www.whocc.no/ddd/definition_and_general_considera/. Accessed 8 May 2017.
Acknowledgements
The authors thank Jens Bos for support in database management and Jackie Senior for editing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. Open access was funded by the University of Groningen, Groningen, as part of the COMPACT agreement between Springer and the Association of Dutch Universities and Academy Institutes.
Conflicts of interest
Y.H. Tran, C.C.M. Schuiling-Veninga, J.E.H. Bergman, H. Groen, and B. Wilffert have no conflicts of interest.
Ethical approval
No formal consent is required for this type of study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Tran, YH., Schuiling-Veninga, C.C.M., Bergman, J.E.H. et al. Impact of Muscarinic M3 Receptor Antagonism on the Risk of Type 2 Diabetes in Antidepressant-Treated Patients: A Case-Controlled Study. CNS Drugs 31, 483–493 (2017). https://doi.org/10.1007/s40263-017-0436-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-017-0436-x