Abstract
Background and Objectives
Fixed-dose combination formulations where several drugs are included in one tablet are important for the implementation of many long-term multidrug therapies. The selection of optimal dose ratios and tablet content of a fixed-dose combination and the design of individualized dosing regimens is a complex task, requiring multiple simultaneous considerations.
Methods
In this work, a methodology for the rational design of a fixed-dose combination was developed and applied to the case of a three-drug pediatric anti-tuberculosis formulation individualized on body weight. The optimization methodology synthesizes information about the intended use population, the pharmacokinetic properties of the drugs, therapeutic targets, and practical constraints. A utility function is included to penalize deviations from the targets; a sequential estimation procedure was developed for stable estimation of break-points for individualized dosing. The suggested optimized pediatric anti-tuberculosis fixed-dose combination was compared with the recently launched World Health Organization-endorsed formulation.
Results
The optimized fixed-dose combination included 15, 36, and 16% higher amounts of rifampicin, isoniazid, and pyrazinamide, respectively. The optimized fixed-dose combination is expected to result in overall less deviation from the therapeutic targets based on adult exposure and substantially fewer children with underexposure (below half the target).
Conclusion
The development of this design tool can aid the implementation of evidence-based formulations, integrating available knowledge and practical considerations, to optimize drug exposures and thereby treatment outcomes.
Similar content being viewed by others
Development of a tool for the evidence-based design of combination tablets, integrating available knowledge on pharmacokinetics, population characteristics, and practical considerations. |
A pediatric anti-tuberculosis fixed-dose combination was designed as a motivating example, and compared with a World Health Organization-endorsed product currently in clinical trials. |
This tool can aid the medical community to move away from dosing schedules following the outdated constant milligram/kilogram principle, and instead strive for rational knowledge-based designs. |
1 Introduction
The combination of several drugs in a fixed-dose combination (FDC) formulation is known to increase compliance in long-term multi-drug therapy [1, 2]. Fixed-dose combinations can apart from reducing the pill burden, also simplify the prescription procedure and the distribution chain in the healthcare system [3]. It is also suggested that FDCs decrease the risk of resistance development in the treatment of infectious diseases by preventing monotherapy [3,4,5], but formulations can naturally not overcome inter-individual variability in pharmacokinetics, which may also drive resistance development [6]. Fixed-dose combinations are used in a range of disease areas, such as hypertension [7], diabetes mellitus [8], human immunodeficiecny virus [9], and tuberculosis (TB) [10]. Drawbacks of FDCs are potential issues with pharmaceutical formulations [11, 12], and decreased flexibility of dosing. It is a complex task to design FDCs; choosing the optimal amount of each compound in one FDC and selecting cut-off values for potential covariate-based individualized dosing demand multiple simultaneous considerations.
The goal of dose individualization is usually to obtain similar exposures, and thereby similar responses, across a diverse population. A common variable for the adjustment of dose to individual patients is their size generally described by body weight, and this is particularly important for children. The traditional approach, which remains widely used, is constant milligram/kilogram-based dosing [13]. However, because the relationship between drug clearance and body weight is not linear but rather allometric [13,14,15,16], this approach is known to lead to under-dosing of children [17,18,19,20]. It is also well established that developmental processes, e.g., maturation of liver enzymes, will affect the pharmacokinetics in infants and toddlers [14, 21]. The rational method for individualized doses is to consider the actual relationship between possible individualization variable(s) and the pharmacokinetic (PK) parameters determining the exposure [22, 23].
In this work, we present a method for evidence-based selection of drug content and corresponding individualized dosing for FDCs, using the existing knowledge of pharmacokinetics described by pharmacometric models, incorporating covariate relationships such as size and age. The work builds on earlier presented methods for dose individualization of single compounds where the optimal regimen is selected by minimizing a defined utility function [22, 24]. The methodology was here extended to encompass multiple drugs simultaneously, and the estimation procedure was refined.
We applied our method to the design of pediatric FDCs of the first-line anti-TB drugs. In 2015, one million children (aged <15 years) developed TB and, even though effective treatment exists, 210,000 died [25]. The intensive phase of first-line anti-TB treatment includes three or four drugs: rifampicin, isoniazid, and pyrazinamide with the addition of ethambutol in settings with high levels of isoniazid resistance and/or high human immunodeficiency virus prevalence [26]. The World Health Organization (WHO) recommends the use of FDCs in the treatment of TB [27], but until the end of 2015 there were no formulations designed to deliver the drugs according to WHO’s current milligram/kilogram dosing guidelines of the first-line anti-TB drugs in children [26, 28]. As an interim measure, the WHO provided advice on how to use the available formulations to dose children, but dosing was cumbersome [29]. Recently, a WHO-endorsed pediatric anti-TB FDC has been launched [30], and is currently being tested in the SHINE study investigating treatment shortening for children with non-severe, symptomatic but smear-negative pulmonary TB [31]. The drug content, ratios, and weight banding were selected to achieve milligram/kilogram doses of each drug close to the WHO recommendations with as little variability over the weight range as possible [30]. In the last section of this work, we compare the exposures expected with the suggested optimized FDC to those expected with the WHO-recommended FDC.
2 Methods
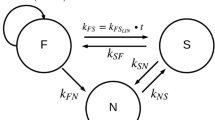
The components of the methodology for optimized FDC design are listed in information box 1 [22]. The main principle of the approach we propose is to simultaneously estimate the amount of each compound in one tablet and the values of the individualization variable (IV) at which the number of administered tablets should be changed [i.e., the break-points (BPs)]. This is done by minimizing a utility function accounting for the defined targets, PK models, intended use population, and constraints. Minimizing the utility function entails finding the drug amounts and BPs resulting in the overall lowest deviation in exposure from the target, where the importance of the deviation is weighted by the chosen penalty function. For the population of interest, a large (>10,000) dataset with representative covariates of importance for the PK models is needed. Based on the inter-individual variability predicted by the PK models, individual parameters defining the exposure of each drug can be simulated and included in the population dataset. This serves as the input to the FDC optimization procedure.
Estimation of BPs, which are discontinuous in nature, can be difficult and sensitive to initial estimates. The evaluated approaches to represent a BP are described in the Electronic Supplementary Material (ESM). Estimation and simulation were performed with the software NONMEM Version 7.3 (ICON Development Solutions, Ellicott City, MD, USA). Both gradient-based and expectation-maximization algorithms were evaluated [32]. R (R Foundation for Statistical Computing, Vienna, Austria) was used for data management, post-processing of results, and plotting [33].
To render the optimized FDC and individualization schedule practically feasible, the estimated optimal drug amounts were rounded to the closest 5 mg and the BPs to the closest kilogram. The optimized, the rounded optimized, and the WHO-recommended anti-TB pediatric FDCs were evaluated with box plots of exposures for each drug and dose group. The relative root mean square error (rRMSE) of the deviation (Δ) between target and individual exposures penalized by the utility function was calculated for each drug and dose group. Additionally, the proportion of underexposed patients, defined as having exposures below half of the target exposure, was determined for the different scenarios.
Information box 1. Components of the optimization methodology |
|---|
Population A description of the population intended to use the fixed-dose combination including relevant covariates and the covariance between them |
Pharmacokinetic models Population pharmacokinetic models of each compound describing the typical dose–concentration relationship, influence of covariates, and random inter-individual variability. Potential PK drug–drug interactions should be accounted for |
Therapeutic targets Pharmacokinetic targets, such as steady-state exposure associated with favorable treatment outcome. These could be determined with pharmacokinetic-pharmacodynamic modeling or selected based on clinical experience |
Individualization variable Covariate to be used for individualization, for example, body weight or creatinine clearance |
Utility function An equation describing how deviations from the therapeutic targets should be penalized. It may include both efficacy and safety aspects |
Practical constraints The number of break-points allowed in the individualization schedule, the unit of the individualization variable, and the maximal number of tablets in any dose group |
3 Results
3.1 Estimation of Break Points
A continuous logistic function (Eq. 1) was selected to mimic the discontinuous step of the BP (0 if IV < BP value, 1 if IV ≥ BP) [34].
A sequential estimation procedure with increasing steepness for the function (i.e., increasing value of γ) and a first-order, gradient-based estimation method proved successful for stable BP estimation. A generic code for a three-drug FDC using the steady-state area under the plasma concentration–time curve (AUC) as a target is provided in the ESM.
3.2 Conditions: Pediatric Anti-TB FDC
For the optimization of pediatric anti-TB FDCs, the following components were used.
3.2.1 Population
Children weighting between 3 and 25 kg. A dataset including 43,400 virtual children with age uniformly distributed between 0 and 18 years was constructed. Male/female sex was assigned with a 50/50 probability. An adjusted growth reference per sex and randomly generated z-scores for weight were used to simulate body weight. Details on the adjusted growth reference used for simulations of the realistic pediatric TB cohort are provided in the ESM. After exclusion of children outside the defined weight range (3–25 kg), 26,275 children remained in the optimization population. The simulated age-weight distribution was compared with reference datasets of children with TB and found to agree well.
3.2.2 Therapeutic Targets
For an infectious disease such as TB, therapeutic targets for children can generally be expected to be the same as in adults [35]. In this work, we used as targets the median AUC at steady state in adults receiving recommended doses. The values were obtained from previous simulations in a South African setting [36,37,38,39] and are listed in Table 1.
3.2.3 Population PK Models
The models for rifampicin, isoniazid, and pyrazinamide by Zvada et al. developed on a dataset including 76 South African children between 2.4 months and 11 years old were used [36]. The models for all three drugs include allometric scaling with body weight. The models for rifampicin and isoniazid also include maturation functions for clearance over post-menstrual age, reaching close to full maturation around an age of 2 years. Additionally, the isoniazid model included three sub-populations representing fast, intermediate, and slow acetylators.
3.2.4 Individualization Variable
Body weight was selected as the individualization variable because it is the most important determinant of exposure in children according to the selected PK models. It is also a readily available metric, making the individualization feasible in resource-limited settings.
3.2.5 Utility Function
The first-line TB drugs are generally safe with few exposure-related side effects [40, 41]. Underexposure of anti-infective agents should be avoided to ensure sufficient efficacy and prevent resistance development [42]. Therefore, a utility function penalizing exposures below the target heavier than exposures above the target was selected, minimizing the sum of the log-scale deviations (Δ) between the target and the individual exposures (Eq. 2).
3.2.6 Practical Constraints
To enable comparison with the WHO-recommended FDC, identical constraints were used: four dose groups, only whole tablets administered and one tablet to the first dose group.
3.3 Findings: Pediatric Anti-TB FDC
The tablet content and BPs for the resulting optimized FDC are described in Table 2, together with the rounded optimized FDC and the WHO-recommended FDC. The doses suggested by the optimization procedure are higher (+15 to +36%) than the doses in the WHO recommended for all three drugs. The BPs are similar, but with a 1-kg lower limit between the lightest groups suggested with the optimized FDC. The expected distributions of exposures for the three drugs with the rounded optimized and the WHO FDC designs are visualized in Fig. 1, together with the reference intervals for adults obtained from Zvada et al. [36].
Expected exposure [area under the plasma concentration–time curve (AUC) at steady state] for the three drugs in the simulated pediatric population with the World Health Organization (WHO)-recommended and optimized fixed-dose combination (FDC) dosing regimen. The boxes represent the 25th, 50th, and 75th percentiles, the whiskers represent the 2.5th and 97.5th percentiles. The horizontal lines represent the 5th, 50th, and 95th percentile of corresponding adult exposures as derived by Zvada et al. [36]
The rRMSE was calculated as per Eq. (3). The rRMSEs were generally lower for the optimized FDC compared with the WHO-recommended FDC for all three drugs, and the rounding did not worsen the rRMSEs notably (Fig. 2). The proportion of underexposed children, defined as AUC below half of the target, is expected to be lower with the optimized FDC compared with the WHO-recommended FDC for all drugs in all dose groups (Fig. 3).
4 Discussion
In this work, we have demonstrated a way to rationally design FDCs and choose an individualization schedule based on knowledge of exposure targets, pharmacokinetics, and the intended use population. In the current era with extensive information about PK properties for many compounds established and computational power being readily available, we and others [22, 23] argue that it should be the norm to strive for an evidence-based design rather than over-simplistically aiming for constant milligram/kilogram dosing.
Many extensions to the general framework presented here are possible. Instead of overall exposure, one can use any other PK metric as a target variable, e.g., maximal or minimal concentration, time above a certain threshold, in the case of antimicrobials, PK metrics adjusted for individual minimal inhibitory concentrations. The utility function can be expanded and/or adjusted to represent the exposure-response-safety profile of each drug. The penalty for deviating from a target can also be made dependable of individual characteristics, for example, one could imagine penalizing deviations in certain vulnerable populations harder. The utility function could be different for the different components of the FDC, or have the same definition but be weighted differentially according to the importance of each component.
The optimization approach taken here is utilitarian: it minimized the overall deviation from the target in the whole population. This may cause BPs to be selected such that the extreme dose groups, the first and the last, become small and thus get markedly worse exposures to improve the exposures for the large majority. In practice, this would generally not be acceptable from an ethical point of view. Furthermore, the relative increase in dose is biggest when going from one to two tablets, intrinsically leading to a larger spread of exposures around this BP. A simple remedy would be to allow the first dose group to start with two (or more) tables. Technically more demanding would be to incorporate in the utility function a measure of the relative bias between the different dose groups, which prevents the differences from becoming large. NONMEM was a convenient choice for the optimization procedure because population PK models used for the simulations of PK metrics often are implemented in this software. However, the code for the optimization procedure can readily be translated to e.g., Matlab or R.
The optimization of pediatric anti-TB FDCs, used as an example in this work, can be further refined. For example, instead of uniform ages, one could consider including epidemiological data on the age distribution of children with TB to generate a population following the observed pattern of higher prevalence in children under 5 years of age [43, 44]. However, given the utilitarian approach, doing this would intrinsically lead to a priority of the youngest children over the slightly older children, which in turn rises ethical questions regarding the fairness of prioritizing one population over another just because of their respective sizes. The population PK models used in the optimization procedure were all developed on data from South Africa [36], hence their appropriateness to adequately represent the global pediatric TB population is uncertain. For generalizable results, the optimization should preferably be performed with models developed on data from a range of high-burden countries, or alternatively using multiple models for each drug describing different populations to account for the global distribution of genetic polymorphisms in metabolizing enzymes. Therapeutic drug monitoring could be a useful strategy to confirm adequate drug exposure [45].
A specific limitation of the applied pyrazinamide model is the absence of the expected age-maturation function [36], leading to prediction of low exposures for the youngest age-group as demonstrated in Fig. 1. The sensitivity of the results to inclusion of such maturation function was evaluated by first estimating the typical shape of such a function using unpublished data from the Datic study (results not shown), and subsequently repeating the optimization procedure with the updated model. The estimates of optimal pyrazinamide dose and BPs differed only 3–6% from the estimate obtained in the original procedure. For isoniazid, the known global variability in the distribution of arylamine N-acetyltransferase 2 gene variations, which strongly impacts isoniazid clearance, is a complicating factor [46]. In South Africa, and in the model used for the optimization, the proportion of fast acetylators is relatively high seen on the global scale [36, 46]. When optimizing assuming such a distribution, the isoniazid dose becomes relatively higher and the risk of underexposures is minimized. Given that much higher isoniazid doses (>15 mg/kg) routinely are used in treatment of multi-drug resistant TB, we do not expect this to lead to general safety issues [47, 48]. However, slow acetylators may have a relatively increased risk of adverse drug reactions such as liver injury [49]. Exposure targets in adults are generally not well established for the first-line TB drugs, and the targets used in this work were derived from a single adult population. Given the large variability in reported exposures from different locations, and when using different drug formulation [50], this is a weakness.
Furthermore, using adult exposure targets for children may be debatable in the case of TB, as the disease manifestations may differ [51]. The practical limitations for the optimization, such as the number of dose levels, as well as considerations regarding the shape of the utility function, the targets, and the relative importance of the included drugs should be further discussed by stakeholders before a final recommendation for the design of pediatric anti-TB FDCs can be given. In the interim, the results presented here indicate that the newly launched pediatric FDC endorsed by the WHO may contain too low doses, given our current best knowledge of the pharmacokinetics of the first-line anti-TB drugs in adults and children. We recommend that the PK observations from the ongoing SHINE study are carefully assessed and compared with exposure targets.
5 Conclusions
Previous work striving for a rational FDC design has often focused on a posteriori evaluation of suggested designs using Monte Carlo simulations [52,53,54]. In this project, we have developed and tested a methodology to enable a priori optimization of both tablet content and BPs for individualization. The method is readily implementable, applicable for diverse exposure–response relationships, and in contrast to Monte Carlo simulations, it does not require testing of a wide range of scenarios. With the availability of this tool, we hope to aid the medical community to move away from over-simplified dosing schedules following the outdated constant milligram/kilogram principle, and instead strive for rational designs integrating available knowledge on pharmacokinetics, population characteristics, and practical considerations to optimize exposures and thereby treatment outcomes.
Change history
02 November 2019
In the online supplementary
02 November 2019
In the online supplementary
References
Bangalore S, Kamalakkannan G, Parkar S, Messerli FH. Fixed-dose combinations improve medication compliance: a meta-analysis. Am J Med. 2007;120:713–9.
Connor J, Rafter N, Rodgers A. Do fixed-dose combination pills or unit-of-use packaging improve adherence? A systematic review. Bull World Health Organ. 2004;82:935–9.
Blomberg B, Spinaci S, Fourie B, Laing R. The rationale for recommending fixed-dose combination tablets for treatment of tuberculosis. Bull World Health Organ. 2001;79:61–8.
Blanco JL, Montaner JSG, Marconi VC, Santoro MM, Campos-Loza AE, Shafer RW, et al. Lower prevalence of drug resistance mutations at first-line virological failure to first-line therapy with atripla vs. tenofovir + emtricitabine/lamivudine + efavirenz administered on a multiple tablet therapy. AIDS. 2014;28:2531–9.
Moulding TS, Le HQ, Rikleen D, Davidson P. Preventing drug-resistant tuberculosis with a fixed dose combination of isoniazid and rifampin. Int J Tuberc Lung Dis. 2004;8:743–8.
Srivastava S, Pasipanodya JG, Meek C, Leff R, Gumbo T. Multidrug-resistant tuberculosis not due to noncompliance but to between-patient pharmacokinetic variability. J Infect Dis. 2011;204:1951–9.
Jackson KC, Sheng X, Nelson RE, Keskinaslan A, Brixner DI. Adherence with multiple-combination antihypertensive pharmacotherapies in a US managed care database. Clin Ther. 2008;30:1558–63.
Melikian C, White TJ, Vanderplas A, Dezii CM, Chang E. Adherence to oral antidiabetic therapy in a managed care organization: a comparison of monotherapy, combination therapy, and fixed-dose combination therapy. Clin Ther. 2002;24:460–7.
Ramjan R, Calmy A, Vitoria M, Mills EJ, Hill A, Cooke G, et al. Systematic review and meta-analysis: patient and programme impact of fixed-dose combination antiretroviral therapy. Trop Med Int Health. 2014;19:501–13.
Albanna AS, Smith BM, Cowan D, Menzies D. Fixed-dose combination antituberculosis therapy: a systematic review and meta-analysis. Eur Respir J. 2013;42:721–32.
Laserson KF, Kenyon AS, Kenyon TA, Layloff T, Binkin NJ. Substandard tuberculosis drugs on the global market and their simple detection. Int J Tuberc Lung Dis. 2001;5:448–54.
Singh S, Mariappan TT, Shankar R, Sarda N, Singh B. A critical review of the probable reasons for the poor variable bioavailability of rifampicin from anti-tubercular fixed-dose combination (FDC) products, and the likely solutions to the problem. Int J Pharm. 2001;228:5–17.
Cella M, Knibbe C, Danhof M, Della Pasqua O. What is the right dose for children? Br J Clin Pharmacol. 2010;70:597–603.
Anderson BJ, Holford NHG. Mechanism-based concepts of size and maturity in pharmacokinetics. Annu Rev Pharmacol Toxicol. 2008;48:303–32.
Liu T, Ghafoori P, Gobburu JVS. Allometry is a reasonable choice in pediatric drug development. J Clin Pharmacol. 2017;57(4):469–75.
Mahmood I. Prediction of drug clearance in children from adults: a comparison of several allometric methods. Br J Clin Pharmacol. 2006;61:545–57.
Dorlo TPC, Huitema ADR, Beijnen JH, de Vries PJ. Optimal dosing of miltefosine in children and adults with visceral leishmaniasis. Antimicrob Agents Chemother. 2012;56:3864–72.
Tarning J, Zongo I, Somé FA, Rouamba N, Parikh S, Rosenthal PJ, et al. Population pharmacokinetics and pharmacodynamics of piperaquine in children with uncomplicated falciparum malaria. Clin Pharmacol Ther. 2012;91:497–505.
Walsh TJ, Driscoll T, Milligan PA, Wood ND, Schlamm H, Groll AH, et al. Pharmacokinetics, safety, and tolerability of voriconazole in immunocompromised children. Antimicrob Agents Chemother. 2010;54:4116–23.
Fillekes Q, Natukunda E, Balungi J, Kendall L, Bwakura-Dangarembizi M, Keishanyu R, et al. Pediatric underdosing of efavirenz: a pharmacokinetic study in Uganda. J Acquir Immune Defic Syndr. 1999;2011(58):392–8.
Johnson TN, Rostami-Hodjegan A, Tucker GT. Prediction of the clearance of eleven drugs and associated variability in neonates, infants and children. Clin Pharmacokinet. 2006;45:931–56.
Jönsson S, Karlsson MO. A rational approach for selection of optimal covariate-based dosing strategies. Clin Pharmacol Ther. 2003;73:7–19.
Vinks AA, Emoto C, Fukuda T. Modeling and simulation in pediatric drug therapy: application of pharmacometrics to define the right dose for children. Clin Pharmacol Ther. 2015;98:298–308.
Viberg A, Cars O, Karlsson MO, Jönsson S. Estimation of cefuroxime dosage using pharmacodynamic targets, MIC distributions, and minimization of a risk function. J Clin Pharmacol. 2008;48:1270–81.
World Health Organization. Global tuberculosis report 2016. WHO/HTM/TB/2016.13. Geneva: World Health Organization; 2016.
World Health Organization. Guidance for national tuberculosis programmes on the management of tuberculosis in children. WHO/HTM/TB/2006.371. Geneva: World Health Organization; 2014.
World Health Organization. The global plan to stop TB, 2011–2015. WHO/HTM/TB/2010.2. Geneva: World Health Organization; 2010.
World Health Organization. Rapid advice: treatment of tuberculosis in children. WHO/HTM/TB/2010.13. Geneva: World Health Organization; 2010.
World Health Organization. Dosing instructions for the use of currently available fixed-dose combination TB medicines for children. http://apps.who.int/medicinedocs/documents/s19927en/s19927en.pdf. 2009. Accessed 26 Jun 2017.
Graham SM, Grzemska M, Gie RP. The background and rationale for a new fixed-dose combination for first-line treatment of tuberculosis in children. Int J Tuberc Lung Dis. 2015;19(Suppl. 1):3–8.
SHINE, Shorter treatment for children with minimal TB, protocol version 1.1. http://www.ctu.mrc.ac.uk/research/documents/tb_protocols/shine_protocol. Accessed 26 Jun 2016.
Beal S, Sheiner LB, Boeckmann A, Bauer RJ. NONMEM user’s guides (1989–2013). Ellicott City: Icon Development Solutions; 2013.
R Core Team. R: A language and environment for statistical computing. Vienna; 2014. http://www.R-project.org. Accessed 26 Jun 2017.
Yngman G. Individualization of fixed-dose combination regimens: methodology and application to pediatric tuberculosis. Master thesis report; Uppsala University, Uppsala, Sweden; 2015.
Dunne J, Rodriguez WJ, Murphy MD, Beasley BN, Burckart GJ, Filie JD, et al. Extrapolation of adult data and other data in pediatric drug-development programs. Pediatrics. 2011;128:e1242–9.
Zvada SP, Denti P, Donald PR, Schaaf HS, Thee S, Seddon JA, et al. Population pharmacokinetics of rifampicin, pyrazinamide and isoniazid in children with tuberculosis: in silico evaluation of currently recommended doses. J Antimicrob Chemother. 2014;69:1339–49.
Wilkins JJ, Savic RM, Karlsson MO, Langdon G, McIlleron H, Pillai G, et al. Population pharmacokinetics of rifampin in pulmonary tuberculosis patients, including a semimechanistic model to describe variable absorption. Antimicrob Agents Chemother. 2008;52:2138–48.
Wilkins JJ, Langdon G, McIlleron H, Pillai G, Smith PJ, Simonsson USH. Variability in the population pharmacokinetics of isoniazid in South African tuberculosis patients. Br J Clin Pharmacol. 2011;72:51–62.
Wilkins JJ, Langdon G, McIlleron H, Pillai GC, Smith PJ, Simonsson USH. Variability in the population pharmacokinetics of pyrazinamide in South African tuberculosis patients. Eur J Clin Pharmacol. 2006;62:727–35.
Yee D, Valiquette C, Pelletier M, Parisien I, Rocher I, Menzies D. Incidence of serious side effects from first-line antituberculosis drugs among patients treated for active tuberculosis. Am J Respir Crit Care Med. 2003;167:1472–7.
Ormerod LP, Horsfield N. Frequency and type of reactions to antituberculosis drugs: observations in routine treatment. Tuber Lung Dis. 1996;77:37–42.
Gumbo T, Louie A, Deziel MR, Liu W, Parsons LM, Salfinger M, et al. Concentration-dependent Mycobacterium tuberculosis killing and prevention of resistance by rifampin. Antimicrob Agents Chemother. 2007;51:3781–8.
Donald PR. Childhood tuberculosis: the hidden epidemic. Int J Tuberc Lung Dis. 2004;8:627–9.
Seddon JA, Shingadia D. Epidemiology and disease burden of tuberculosis in children: a global perspective. Infect Drug Resist. 2014;7:153–65.
Alsultan A, Peloquin CA. Therapeutic drug monitoring in the treatment of tuberculosis: an update. Drugs. 2014;74:839–54.
Sabbagh A, Darlu P, Crouau-Roy B, Poloni ES. Arylamine N-acetyltransferase 2 (NAT2) genetic diversity and traditional subsistence: a worldwide population survey. PLoS One. 2011;6:e18507.
World Health Organization. Treatment guidelines for drugresistant tuberculosis, 2016 update. http://apps.who.int/iris/bitstream/10665/250125/1/9789241549639-eng.pdf?ua=1. Accessed 26 Jun 2017.
Katiyar SK, Bihari S, Prakash S, Mamtani M, Kulkarni H. A randomised controlled trial of high-dose isoniazid adjuvant therapy for multidrug-resistant tuberculosis. Int J Tuberc Lung Dis. 2008;12:139–45.
Azuma J, Ohno M, Kubota R, Yokota S, Nagai T, Tsuyuguchi K, et al. NAT2 genotype guided regimen reduces isoniazid-induced liver injury and early treatment failure in the 6-month four-drug standard treatment of tuberculosis: a randomized controlled trial for pharmacogenetics-based therapy. Eur J Clin Pharmacol. 2013;69:1091–101.
McIlleron H, Wash P, Burger A, Norman J, Folb PI, Smith P. Determinants of rifampin, isoniazid, pyrazinamide, and ethambutol pharmacokinetics in a cohort of tuberculosis patients. Antimicrob Agents Chemother. 2006;50:1170–7.
Burman WJ, Cotton MF, Gibb DM, Walker AS, Vernon AA, Donald PR. Ensuring the involvement of children in the evaluation of new tuberculosis treatment regimens. PLoS Med. 2008;5:e176.
Cella M, Kloprogge F, Danhof M, Della Pasqua O. Dosing rationale for fixed-dose combinations in children: shooting from the hip? Clin Pharmacol Ther. 2012;91:718–25.
Bouazza N, Foissac F, Fauchet F, Burger D, Kiechel J-R, Treluyer J-M, et al. Lopinavir/ritonavir plus lamivudine and abacavir or zidovudine dose ratios for paediatric fixed-dose combinations. Antivir Ther. 2015;20:225–33.
Bouazza N, Cressey TR, Foissac F, Bienczak A, Denti P, McIlleron H, et al. Optimization of the strength of the efavirenz/lamivudine/abacavir fixed-dose combination for paediatric patients. J Antimicrob Chemother. 2017;72:490–5.
Acknowledgements
The authors thank the Desmond Tutu TB Centre, Department of Paediatrics and Child Health, Stellenbosch University, South Africa, for sharing age-weight data used in the development of the simulation tool for a representative age-weight distribution in tuberculosis-infected children.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Elin M. Svensson, Gunnar Yngman, Paolo Denti, Helen McIlleron, Maria C Kjellsson, and Mats O. Karlsson have no conflicts of interest directly relevant to the content of this article.
Funding
This work was supported by the Swedish Research Council (Grant No. 521-2011-3442), the Swedish Foundation for International Cooperation in Research and Higher Education, STINT, jointly with the South African National Research Council, National Research Foundation [NRF] (Grant No. STINT: SA2015-6259, NRF: 101575), and the Innovative Medicines Initiative Joint Undertaking (http://www.imi.europa.eu) for the PreDiCT-TB consortium (Grant Agreement 115337), resources of which are composed of a financial contribution from the European Union’s Seventh Framework Programme (FP7/2007-2013) and EFPIA companies’ in-kind contribution. Helen McIlleron was supported in part by the South African National Research Council (Grant No. 90729). The Datic study from which age-weight data were used was supported by the National Institutes of Health (Bethesda, MD, USA) and Eunice Kennedy Shriver National Institute of Child Health and Human Development (Bethesda, MD, USA) (Grant No. R01HD069175).
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Svensson, E.M., Yngman, G., Denti, P. et al. Evidence-Based Design of Fixed-Dose Combinations: Principles and Application to Pediatric Anti-Tuberculosis Therapy. Clin Pharmacokinet 57, 591–599 (2018). https://doi.org/10.1007/s40262-017-0577-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-017-0577-6