Abstract
Background and Objective
Abnormalities in melatonin levels have been linked to delirium. This dysregulation may be offset with the use of ramelteon, a melatonin receptor agonist. The purpose of this study was to evaluate the role of ramelteon in decreasing the need for as-needed (PRN) use of antipsychotics in elderly patients with delirium.
Methods
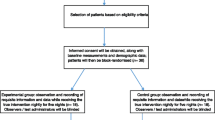
This was a single-center, retrospective study involving 488 patients who were placed on constant observation and received care by psychiatric service from May 2015 through October 2015. Of these patients, 125 patients were age 65 years or above, had a diagnosis of delirium, and had no standing orders for antipsychotics. These 125 patients were divided into the non-ramelteon group (who received no ramelteon and PRN antipsychotics) and the ramelteon group (who received ramelteon plus PRN antipsychotics). The use of PRN antipsychotics for agitation in each group was recorded.
Results
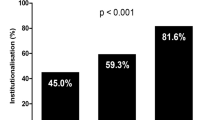
The ramelteon group had a lower incidence of PRN antipsychotic use compared to those not given ramelteon (60 vs. 80%, p value = 0.001). After adjustment for race, age, length of stay, and gender, patients in the non-ramelteon group were more likely to have been given antipsychotics compared to those in the ramelteon group (odds ratio = 4.3, p value = 0.002).
Conclusion
Ramelteon use in elderly patients with delirium may be associated with statistically significant reduction of PRN antipsychotic use for agitation.
Similar content being viewed by others
References
Inouye SK. Delirium in older persons. N Engl J Med. 2006;354(11):1157–65.
Hshieh TT, Yue J, Oh E, et al. Effectiveness of multicomponent nonpharmacological delirium interventions: a meta-analysis. JAMA Intern Med. 2015;175(4):512–20.
Conn DK, Madan R. Use of sleep-promoting medications in nursing home residents: risks versus benefits. Drugs Aging. 2006;23(4):271–87.
Worley LL, Kunkel EJ, Gitlin DF, et al. Constant observation practices in the general hospital setting: a national survey. Psychosomatics. 2000;41(4):301–10.
Young J, Inouye SK. Delirium in older people. BMJ. 2007;334(7598):842–6.
Flaherty JH, Gonzales JP, Dong B. Antipsychotics in the treatment of delirium in older hospitalized adults: a systematic review. J Am Geriatr Soc. 2011;59(Suppl 2):269.
Muench J, Hamer AM. Adverse effects of antipsychotic medications. Am Fam Physician. 2010;81(5):617–22.
Center for Drug Evaluation and Research. Drug safety and availability—information for healthcare professionals: conventional antipsychotics. US Food and Drug Administration Home Page. https://www.fda.gov/Drugs/DrugSafety/ucm124830.htm. Published 8 May 2013. Accessed 30 Mar 2017.
Martins S, Fernandes L. Delirium in elderly people: a review. Front Neurol. 2012;3:101.
Fong TG, Tulebaev SR, Inouye SK. Delirium in elderly adults: diagnosis, prevention and treatment. Nat Rev Neurol. 2009;5(4):210–20.
By the American Geriatrics Society 2015 Beers Criteria Update Expert Panel. American Geriatrics Society 2015 updated beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2015;63(11):2227–46.
Ramelteon (rozerem) for insomnia. Med Lett Drugs Ther. 2005;47(1221):89–91.
Dessap AM, Roche-Campo F, Launay JM, et al. Delirium and circadian rhythm of melatonin during weaning from mechanical ventilation: an ancillary study of a weaning trial. Chest. 2015;148(5):1231–41.
Furuya M, Miyaoka T, Yasuda H, et al. Ramelteon as adjunctive therapy for delirium referred to a consultation-liaison psychiatry service: a retrospective analysis. Int J Geriatr Psychiatry. 2015;30(9):994–5.
Furuya M, Miyaoka T, Yasuda H, et al. Marked improvement in delirium with ramelteon: five case reports. Psychogeriatrics. 2012;12(4):259–62.
Fitzgerald JM, Adamis D, Trzepacz PT, et al. Delirium: a disturbance of circadian integrity? Med Hypotheses. 2013;81(4):568–76.
Grover S, Sharma A, Aggarwal M, et al. Comparison of symptoms of delirium across various motoric subtypes. Psychiatry Clin Neurosci. 2014;68(4):283–91.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Financial support and disclosures
We have no financial disclosures for this study and no conflicts of interest.
Rights and permissions
About this article
Cite this article
Pinkhasov, A., James, S.A., Fazzari, M. et al. Role of Ramelteon in Reduction of As-Needed Antipsychotics in Elderly Patients with Delirium in a General Hospital Setting. Clin Drug Investig 37, 1137–1141 (2017). https://doi.org/10.1007/s40261-017-0573-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-017-0573-5