Abstract
Background
In 2018, the Government of India launched Ayushman Bharat Pradhan Mantri-Jan Aarogya Yojana (AB PM-JAY), a large tax-funded health insurance scheme. In this paper, we present findings of the Costing of Health Services in India (CHSI) study, describe the process of use of cost evidence for price-setting under AB PM-JAY, and estimate its fiscal impact.
Methods
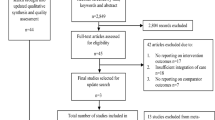
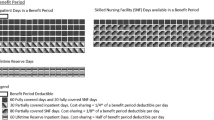
Reference costs were generated from the first phase of CHSI study, which sampled 11 tertiary public hospitals from 11 Indian states. Cost for Health Benefit Packages (HBPs) was estimated using mixed (top-down and bottom-up) micro-costing methods. The process adopted for price-setting under AB PM-JAY was observed. The cost of each HBP was compared with AB PM-JAY prices before and after the revision, and the budgetary impact of this revision in prices was estimated.
Findings
Following the CHSI study evidence and price consultations, 61% of AB PM-JAY HBP prices were increased while 18% saw a decline in the prices. In absolute terms, the mean increase in HBP price was ₹14,000 (₹450–₹1,65,000) and a mean decline of ₹6,356 (₹200–₹74,500) was observed. Nearly 42% of the total HBPs, in 2018, had a price that was less than 50% of the true cost, which declined to 20% in 2019. The evidence-informed revision of HBP prices is estimated to have a minimal fiscal impact (0.7%) on the AB PM-JAY claims pay-out.
Interpretation
Evidence-informed price-setting helped to reduce wide disparities in cost and price, as well as aligning incentives towards broader health system goals. Such strategic purchasing and price-setting requires the creation of systems of generating evidence on the cost of health services. Further research is recommended to develop a cost-function to study changes in cost with variations in time, region, prices, skill-mix and other factors.





Similar content being viewed by others
Change history
26 March 2021
A Correction to this paper has been published: https://doi.org/10.1007/s40258-021-00645-5
References
Home | Ayushman Bharat [Internet]. Pmjay.gov.in. 2020 [cited 3 January 2020]. https://www.pmjay.gov.in/. Accessed 3 Jan 2020.
Mathauer I, Dale E, Meessen B. Strategic purchasing for Universal Health Coverage: key policy issues and questions. A summary from expert and practitioners’ discussions Geneva: World Health Organization; 2017. Licence: CC BY-NC-SA 3.0 IGO
Barber SL, Lorenzoni L, Ong P. Price setting and price regulation in health care: lessons for advancing Universal Health Coverage. Geneva: World Health Organization, Organisation for Economic Co-operation and Development; 2019. Licence: CC BY-NC-SA 3.0 IGO
Kutzin J. A descriptive framework for country-level analysis of health care financing arrangements. Health Policy. 2001;56(3):171–204.
Figueras J, Robinson R, and Jakubowski E. Eds. Purchasing to improve health systems performance: drawing the lessons. Purchasing to imrpove health systems performance. Open University Pres; 2005. http://bit.ly/2ox0vUJ Cited 10 June 2017. Accessed 3 Jan 2020.
Tompkins CP, Altman SH, Eilat E. The precarious pricing system for hospital services. Health Aff (Millwood). 2006;25(1):45–56.
Journey from HBP 1.0 to HBP 2.0 [Internet]. Pmjay.gov.in. 2020 [cited 5 February 2020]. https://pmjay.gov.in/sites/default/files/2020-01/Journey-from-HBP-1.0-to-HBP-2.0.pdf
Private hospitals to get up to 40% higher than CGHS rates under Ayushman Bharat [Internet]. Businesstoday.in. 2020 [cited 3 January 2020]. https://www.businesstoday.in/current/economy-politics/ayushman-bharat-private-hospitals-cghs-rates-narendra-modi/story/279269.html
Prinja S, Singh MP, Guinness L, Rajsekar K, Bhargava B. Establishing reference costs for the health benefit packages under universal health coverage in India: Cost of Health Services in India (CHSI) Protocol. BMJ Open. 2020;10(7):e035170.
Prinja S, Brar S, Singh MP, et al. Process evaluation of the health system costing—experience from CHSI study in India. PLoS ONE. 2020;15(5):e0232873.
Drummond MF. Methods for the economic evaluation of health care programmes. 2nd ed. Oxford: Oxford Medical Publications; 1997.
Rupee to average 66.20 against dollar in 2017-18: Report [Internet]. Thehinduusinessline.com. 2020 [cited 3 January 2020]. https://www.thehindubusinessline.com/markets/forex/rupee-to-average-at-6620-against-dollar-in-201718-report/article9629444.ece. Accessed 26 Dec 2019.
Özaltın A, Cashin C. Joint learning network, 2019. [cited 1 Septamber 2020]. Jointlearning.org. http://www.jointlearningnetwork.org/uploads/files/resources/JLN_Costing_Toolkit_Interactive_FINAL.pdf. Accessed 1 Sept 2020.
Prinja S, Manchanda N, Mohan P, et al. Cost of neonatal intensive care delivered through district level public hospitals in India. Indian Pediatr. 2013;50(9):839–46.
Jain S, Banga K, Reddy A. Indian Hospital Sector: Modicare – Working towards a healthier India [Internet]. 2018 [cited 28 February 2020]. http://file:///Volumes/data/Papers/CHSI%20results%20paper/reference%20articles/SH-Hospitals-H2-1-September%202018.pdf. Accessed 28 Feb 2020.
Gupta A. Claims data for AB PM-JAY 2018 [Online]. E-mail to Shankar Prinja (shankarprinja@gmail.com) 17 December 2019 [cited 2020 February 5]
Waters HR, Hussey P. Pricing health services for purchasers—a review of methods and experiences. Health Policy. 2004;70(2):175–84 ((Review)).
Conteh L. Cost and unit cost calculations using step-down accounting. Health Policy Plan. 2004;19(2):127–35.
Mathauer I. Setting health insurance remuneration rates of private providers in Kenya: the role of costing, challenges and implications. Int J Health Plann Manag. 2010;26(1):e30–47.
Moens F. Design, implementation, and evaluation of a community financing scheme for hospital care in developing countries: a pre-paid health plan in the Bwamanda health zone. Zaire Soc Sci Med. 1990;30(12):1319–27.
Prinja S, Chauhan A, Angell B, Gupta I, Jan S. A systematic review of the state of economic evaluation for health care in India. Appl Health Econ Health Policy. 2015;13(6):595–613.
Chatterjee S, Laxminarayan R. Costs of surgical procedures in Indian hospitals. BMJ Open. 2013;3(6):e002844.
Chauhan A, Prinja S, Ghoshal S, et al. Cost of treatment for head and neck cancer in India. PLoS ONE. 2018;13(1):e0191132.
Prinja S, Bahuguna P, Duseja A, Kaur M, Chawla Y. Cost of intensive care treatment for liver disorders at tertiary care level in India. Pharmacoecon Open. 2017;2(2):179–90.
Kaur G, Prinja S, Malhotra P, et al. Cost of treatment of multiple myeloma in a public sector tertiary care hospital of North India. Indian J Hematol Blood Transfus. 2018;34(1):25–31.
Prinja S, Sharma YD, et al. Cost of treatment of valvular heart disease at a tertiary hospital in North India: policy implications. Pharmacoecon Open. 2019;3:391–402.
Prinja S, Balasubramanian D, Jeet G, et al. Cost of delivering secondary-level health care services through public sector district hospitals in India. Indian J Med Res. 2017;146(3):354–61.
Minimum Reqirements for Annual M.B.B.S. Admissions Regulations, 2020 [Internet]. Nmc.org.in. 2020 [cited 2 December 2020]. https://www.nmc.org.in/rules-regulations/minimum-requirements-for-annual-m-b-b-s-admissions-regulation2020. Accessed 2 Dec 2020.
Subgroup on Common IT Infrastructure for Health Insurance Claims Management [Internet]. Pmjay.gov.in. 2020 [cited 5 February 2020]. https://www.pmjay.gov.in/sites/default/files/2019-09/Sub%20Group%20on%20Common%20IT%20Infrastructure%20Report_11-09-19.pdf. Accessed 5 Feb 2020.
Prinja S, Chauhan A, Rajsekhar K, et al. Addressing the cost data gap for universal healthcare coverage in India: a call to action. Value Health Reg Issues. 2020;21:226–9.
Bahuguna P, Guinness L, Sharma S, et al. Estimating the unit costs of healthcare service delivery in India: addressing information gaps for price setting and health technology assessment. Appl Health Econ Health Policy. 2020. https://doi.org/10.1007/s40258-020-00566-9.
Prinja S, Selvaraj S, Muraleedharan V, Sundararaman T. National Health System Cost Database for India [Internet]. Healtheconomics.pgisph.in. 2019 [cited 24 May 2020]. https://www.healtheconomics.pgisph.in/costing_web/index.php?action=gen_secondary. Accessed 24 May 2020.
Acknowledgements
We thank Dr Lorna Guinness, Honorary Assistant Professor, Department of Global Health and Development, Imperial College, London for reviewing the manuscript and providing her input. We thank state data collection teams and data analysis team (Rajan Jaswal, Sachin Sharma and Sameer Sharma), Department of Community Medicine and School of Public Health, Postgraduate Institute of Medical Education and Research, Chandigarh, India. CHSI Study Group: Jyotsna Naik, Malkeet Singh, Himanshi Tomar, Rakesh Bahl, Amit Sachdeva, Sharminder Kaur, Sanjay Kumar, Setu Sinha, Varsha Singh, Avijit Hazra, Raghunath Misra, Divya Mehrotra, K. Narayanasamy, A. Chitra, Arun Gupta, Pankaj Bahuguna, Kusum Lata Gaur, Jai Prakash Pankaj, Dharmesh Kumar Sharma, Gajanan D. Velhal, Amit S. Bhondve, Prakash Patel, Amit C. Patel, Rajendra Joshi, Kondeti Madhavi, Pulaganti Madhusudana, Bhabagrahi Rath, Sashi Bhusan Biswal, Ankita Panigrahy.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Funding
The study was funded by the Department of Health Research, Ministry of Health and Family Welfare, India.
Conflicts of interest
None of the authors have any conflicts of interest to declare.
Ethical approval
The study was approved by the Institutional Ethics Committee (IEC) vide letter no. PGI/IEC/2018/00125A and Institutional Collaborative Committee (ICC) vide letter no. 79/30-Edu-13/111273 of Postgraduate Institute of Medical Education and Research, Chandigarh, India.
Consent to participate
Written informed consent was obtained from the participants.
Consent for publication
All the authors give their consent for the publication
Availability of data and material
All the cost information generated by the study is included in the paper and supplementary material. The code availability is not applicable.
Author’s contributions
Study Conception: Shankar Prinja, Balram Bhargava, Praveen Gedam. Development of data collection tools: Maninder Pal Singh, Oshima Sachin, CHSI Study Group. Data Collection: Maninder Pal Singh, Oshima Sachin, CHSI Study Group. Data Analysis: Maninder Pal Singh, Shankar Prinja. Data Interpretation: Shankar Prinja, Balram Bhargava, Praveen Gedam, Anu Nagar, Kavitha Rajsekar. Draft Manuscript: Maninder Pal Singh, Shankar Prinja. Critical contribution in revising manuscript: All Authors.
Additional information
CHSI Study Group: Jyotsna Naik1, Malkeet Singh1, Himanshi Tomar1, Rakesh Bahl5, Amit Sachdeva5, Sharminder Kaur5, Sanjay Kumar6, Setu Sinha6, Varsha Singh6, Avijit Hazra7, Raghunath Misra7, Divya Mehrotra8, K. Narayanasamy9, A. Chitra9, Arun Gupta3, Pankaj Bahuguna1, Kusum Lata Gaur10, Jai Prakash Pankaj10, Dharmesh Kumar Sharma10, Gajanan D. Velhal11, Amit S. Bhondve11, Prakash Patel12, Amit C. Patel12, Rajendra Joshi12, Kondeti Madhavi13, Pulaganti Madhusudana13, Bhabagrahi Rath14, Sashi Bhusan Biswal14, Ankita Panigrahy14.
The original online version of this article was revised: " The members of the CHSI Study Group Should be mentioned in article note on the first page.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Prinja, S., Singh, M.P., Rajsekar, K. et al. Translating Research to Policy: Setting Provider Payment Rates for Strategic Purchasing under India's National Publicly Financed Health Insurance Scheme. Appl Health Econ Health Policy 19, 353–370 (2021). https://doi.org/10.1007/s40258-020-00631-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-020-00631-3