Abstract
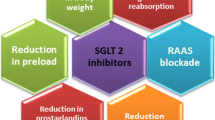
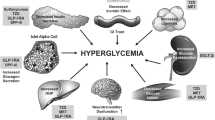
Cardiovascular disease (CVD) is the leading cause of morbidity and mortality in patients with type 2 diabetes mellitus (T2DM). Because of these associated risks, managing diabetes and CVD, including heart failure (HF), has become a joint effort to reduce the risk of adverse outcomes. Although many patients with T2DM are receiving preventive therapies for CVD, their residual risk remains high for atherosclerotic CVD (ASCVD). Recent data regarding the use of antidiabetic medications to prevent negative cardiovascular outcomes has revealed a positive association with reduced major adverse cardiovascular events (MACE). One class of medications, sodium-glucose cotransporter-2 (SGLT-2) inhibitors, are at the forefront of the cardiovascular outcomes prevention discussion. The clinical data presented in this review indicate the potential cardiovascular benefits of SGLT-2 inhibitors in patients with CVD and its potential value as a treatment option in preventing CVD in various patient populations.
Similar content being viewed by others
References
Wiviott SD, Raz I, Bonaca MP, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019;380(4):347–57.
Leiter LA, Cefalu WT, de Bruin TWA, Gause-Nilsoon I, Sugg J, Parikh SK. Dapagliflozin added to usual care in individuals with type 2 diabetes mellitus with preexisting cardiovascular disease: a 24-week, multicenter, randomized, double-blind, placebo-controlled study with a 28-week extension. J Am Geriatr Soc. 2014;62(7):1252–62.
Grundy SM, Benjamin IJ, Burke GL, et al. A Statement for healthcare professionals from the American Heart Association. Circulation. 1999; pp. 1134-1146.
Furtado RHM, Bonaca MP, Raz I, et al. Dapagliflozin and cardiovascular outcomes in patients with type 2 diabetes mellitus and previous myocardial infarction. Circulation. 2019;139(22):2516–27.
Schetharner G, Drexel H, Moshkovich E, et al. BMC endocrine disorders. 2019;19(1).
Schetharner G, Drexel H, Moshkovich E, et al. SGLT2 inhibitors in T2D and associated comorbidities—differentiating within the class. BMC Endocr Disord. 2019;19:64.
Brown AJ, Lang C, McCrimmon R, Struthers A. Does dapagliflozin regress left ventricular hypertrophy in patients with type 2 diabetes? A prospective, double-blind, randomised, placebo-controlled study. BMC Cardiovasc Disord. 2017;17(1):229.
Pereira MJ, Eriksson JW. Emerging Role of SGLT-2 inhibitors for the treatment of obesity. Drugs. 2019;79(3):219–30.
Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373(22):2117–28.
Zinman B, Inzucchi SE, Lachin JM, et al. Empagliflozin and cerebrovascular events in patients with type 2 diabetes mellitus at high cardiovascular ris. Stroke. 2017;48(5):1218–25.
Standards of Medical Care in Diabetes-2018. American Diabetes Association. 2018. https://diabetesed.net/wp-content/uploads/2017/12/2018-ADA-Standards-of-Care.pdf. Accessed 20 Dec 2019.
Verma S, Mazer CD, Fitchett D, et al. Empagliflozin reduces cardiovascular events, mortality and renal events in participants with type 2 diabetes after coronary artery bypass graft surgery: subanalysis of the EMPA-REG OUTCOME® randomised trial. Diabetologia. 2018;61(8):1712–23.
Wanner C, Lachin JM, Inzucchi SE, et al. Empagliflozin and clinical outcomes in patients with type 2 diabetes mellitus, established cardiovascular disease, and chronic kidney disease. Circulation. 2018;137(2):119–29.
EMPA-KIDNEY (The Study of Heart and Kidney Protection With Empagliflozin). ClinicalTrials.gov. 2018. https://clinicaltrials.gov/ct2/show/NCT03594110. Accessed 26 Oct 2019.
Study Tests Empagliflozin in Patients With Chronic Heart Failure With Reduced Ejection Fraction (HFrEF). The study looks at how far patients can walk in 6 minutes and at their heart failure symptoms. ClinicalTrials.gov. 2018. https://clinicaltrials.gov/ct2/show/NCT03448419. Accessed 26 Oct 2019.
This Study Tests Empagliflozin in Patients With Chronic Heart Failure With Preserved Ejection Fraction (HFpEF). The study looks at how far patients can walk in 6 minutes and at their heart failure symptoms. ClinicalTrials.gov. 2018. https://clinicaltrials.gov/ct2/show/NCT03057951. Accessed 26 Feb 2019.
EMPagliflozin outcomE tRial in Patients With chrOnic heaRt Failure With Preserved Ejection Fraction (EMPEROR-Preserved). ClinicalTrails.gov. 2017. https://clinicaltrials.gov/ct2/show/NCT03057951. Accessed 26 Oct 2019.
EMPagliflozin outcomE tRial in Patients With chrOnic heaRt Failure With Reduced Ejection Fraction (EMPEROR-Reduced). https://clinicaltrials.gov/ct2/show/NCT03057977. 2017. https://clinicaltrials.gov/ct2/show/NCT03057977. Accessed 26 Oct 2019.
INVOKANA® (canagliflozin) tablets. September 2019. http://www.janssenlabels.com/package-insert/product-monograph/prescribing-information/INVOKANA-pi.pdf. Accessed 20 Dec 2019.
Neal B, Perkovic V, Mahaffey KW, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377(7):644–57.
Zhou Z, Lindley RI, Radholm K, et al. Canagliflozin and stroke in type 2 diabetes mellitus. Stroke. 2019;50(2):396–404.
Radholm K, Figtree G, Perkovic V, et al. Canagliflozin and heart failure in type 2 diabetes mellitus. Circulation. 2018;138(5):458–68.
Sarnak MJ, Levey AS, Schoolwerth AC, et al. Kidney disease as a risk factor for development of cardiovascular disease. Circulation. 2003;108(17):2154–69.
Perkovic V, Jardine MJ, Neal B, et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med. 2019;380(24):2295–306.
Farxiga® (dapagliflozin tablets): US prescribing information. Princeton, NJ: Bristol-Myers Squibb, 2014.
Study to Evaluate the Effect of Dapagliflozin on the Incidence of Worsening Heart Failure or Cardiovascular Death in Patients With Chronic Heart Failure (DAPA-HF). ClinicalTrials.gov. 2017. https://clinicaltrials.gov/ct2/show/NCT03036124. Accessed 20 Dec 2019.
FARXIGA met primary endpoint in landmark Phase III DAPA-HF trial for the treatment of patients with heart failure. AstraZeneca. 2019. https://www.astrazeneca-us.com/content/az-us/media/press-releases/2019/farxiga-met-primary-endpoint-in-landmark-phase-iii-dapa-hf-trial-for-the-treatment-of-patients-with-heart-failure-08202019.html. Accessed 20 Dec 2019.
McMurray JJ, Solomon SD, Inzucchi SE, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019; p. 3396–3404.
Does Dapagliflozin Regress Left Ventricular Hypertrophy In Patients With Type 2 Diabetes? (DAPA-LVH). ClinicalTrails.gov. https://clinicaltrials.gov/ct2/show/NCT02956811. Accessed 20 Dec 2019.
Akerblom A, Oldgren J, Latva-Rasku A, et al. Effects of DAPAgliflozin on CARDiac substrate uptake, myocardial efficiency, and myocardial contractile work in type 2 diabetes patients-a description of the DAPACARD study. Upsala J Med Sci. 2019;124(1):59–64.
Dapagliflozin Effect on Symptoms and Biomarkers in Patients With Heart Failure (DEFINE-HF). ClincalTrials.gov. 2016. https://clinicaltrials.gov/ct2/show/NCT02653482. Accessed 20 Dec 2019.
A Study to Evaluate the Effect of Dapagliflozin on Renal Outcomes and Cardiovascular Mortality in Patients With Chronic Kidney Disease (Dapa-CKD). ClinicalTrials.gov. 2017. https://clinicaltrials.gov/ct2/show/NCT03036150. Accessed 20 Dec 2019.
Left Ventricular Functional Changes of Uncontrolled Diabetes by Dapagliflozin Treatment Trial (ELUCIDATE). ClinicalTrials.gov. 2019. https://clinicaltrials.gov/ct2/show/NCT03871621. Accessed 20 Dec 2019.
Dapagliflozin in PRESERVED Ejection Fraction Heart Failure (PRESERVED-HF). ClinicalTrials.gov. 2017. https://clinicaltrials.gov/ct2/show/NCT03030235. Accessed 20 Dec 2019.
Dapagliflozin Evaluation to Improve the LIVEs of Patients With PReserved Ejection Fraction Heart Failure. (DELIVER). ClinicalTrials.gob. 2018. https://clinicaltrials.gov/ct2/show/NCT03619213. Accessed 20 Dec 2019.
DETERMINE-preserved - Dapagliflozin Effect on Exercise Capacity Using a 6-minute Walk Test in Patients With Heart Failure With Preserved Ejection Fraction. ClinicalTrials.gov. 2019. https://clinicaltrials.gov/ct2/show/NCT03877224. Accessed 20 Dec 2019.
Highlights Of Prescribing Information-Steglatro. accessdata. 2017. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/209803s000lbl.pdf. Accessed 20 Dec 2019.
Cardiovascular Outcomes Following Ertugliflozin Treatment in Type 2 Diabetes Mellitus Participants With Vascular Disease, The VERTIS CV Study (MK-8835-004). ClinicalTrials.gov. 2013. https://clinicaltrials.gov/ct2/show/NCT01986881. Accessed 20 Dec 2019.
Cannon P, McGuire DK, Pratley R, et al. Design and baseline characteristics of the eValuation of ERTugliflozin efficacy and Safety CardioVascular outcomes trial (VERTIS-CV). Am Heart J. 2018;206:11–23.
Study of Safety and Efficacy Of Ertugliflozin (PF-04971729, MK-8835) In Participants With Type 2 Diabetes And Hypertension (MK-8835-042). ClinicalTrials.gov. 2010. http://clinicaltrials.gov/ct2/show/NCT01096667. Accessed 20 Dec 2019.
Amin NB, Wang X, Mitchell JR, Lee DS, Nucci G, Rusnak JM. Blood pressure-lowering effect of the sodium glucose co-transporter-2 inhibitor ertugliflozin, assessed via ambulatory blood pressure monitoring in patients with type 2 diabetes and hypertension. Diabetes Obe Metab J Pharmacol Therap. 2015;17(8):805–8.
ERtugliflozin triAl in DIabetes With Preserved or Reduced ejeCtion FrAcTion mEchanistic Evaluation in Heart Failure (ERADICATE-HF). ClinicalTrials.gov. 2018. http://clinicaltrials.gov/ct2/show/NCT03416270. Accessed 20 Dec 2019.
Effect of Ertugliflozin on Cardiac Function in Diabetes (ERTU-GLS). ClinicalTrials.gov. October 24, 2018. http://clinicaltrials.gov/ct2/show/NCT03717194. Accessed 20 Dec 2019.
Evaluating Metabolic Mechanisms of Ertugliflozin in Diabetes & Heart Failure (EMMED-HF). ClinicalTrials.gov. 2019. http://clinicaltrials.gov/ct2/show/NCT04071626. Accessed 20 Dec 2019.
Comparison of Pharmacodynamic Effects of Sotagliflozin and Empagliflozin in T2DM Patients With Mild to Moderate Hypertension. ClinicalTrials.gov. March 12, 2018. http://clinicaltrials.gov/ct2/show/NCT03462069. Accessed 20 Dec 2019.
Effect of Sotagliflozin on Cardiovascular Events in Patients With Type 2 Diabetes Post Worsening Heart Failure (SOLOIST-WHF Trial). ClinicalTrials.gov. 2018. http://clinicaltrials.gov/ct2/show/NCT03521934. Accessed 20 Dec 2019.
Effect of Sotagliflozin on Cardiovascular and Renal Events in Patients With Type 2 Diabetes and Moderate Renal Impairment Who Are at Cardiovascular Risk (SCORED). ClinicalTrials.gov. 2017. http://clinicaltrials.gov/ct2/show/NCT03315143. Accessed 20 Dec 2019.
Safety, Tolerability and Pharmacodynamic Activity of Sotagliflozin in Hemodynamically Stable Patients With Worsening Heart Failure. ClinicalTrials.gov. 2017. http://clinicaltrials.gov/ct2/show/NCT03292653. Accessed 20 Dec 2019.
American College of Cardiology. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. 2019. http://www.onlinejacc.org/content/accj/74/10/e177.full.pdf. Accessed 20 Dec 2019.
Kristensen SL, Rørth R, Jhund PS, et al. Cardiovascular, mortality, and kidney outcomes with GLP-1 receptor agonists in patients with type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. The Lancet. 2019;7(10):776–85.
Yuliya L, Petter B, Udell JA, Lovshin JA, Cherney DZ. Sodium glucose cotransporter-2 inhibition in heart failure. Circulation. 2017;136(17):1643–58.
Trujillo JM, Nuffer WA. Impact of sodium-glucose cotransporter 2 inhibitors on. Pharmacotherapy. 2017;37(4):481–91.
Rajeev SP, Wilding JP. SGLT2 inhibition and ketoacidosis—should we be concerned? Br J Diabetes. 2015;15(4):155–8.
Burke KR, Schumacher CA, Harpe SE. SGLT2 Inhibitors: a Systematic Review of Diabetic Ketoacidosis and Related Risk Factors in the Primary Literature. Pharmacotherapy. 2017;37(2):187–94.
Funding
No external funding was used in the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
Jessica Reid, Khyatiben Rana, Stephanie Niman, Mae Sheikh-Ali, Todd Lewis, Rushab R. Choksi, and Rebecca F. Goldfaden have no potential conflicts of interest that might be relevant to the contents of this manuscript.
Rights and permissions
About this article
Cite this article
Reid, J., Rana, K., Niman, S. et al. Sodium-Glucose Cotransporter-2 (SGLT-2) Inhibitors for Cardiovascular Disease Prevention. Am J Cardiovasc Drugs 20, 419–429 (2020). https://doi.org/10.1007/s40256-020-00397-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40256-020-00397-y