Abstract
Aims
Diabetic peripheral neuropathy affects up to 60% of individuals and often leads to foot ulceration and eventual amputation. When oral therapy has failed to achieve pain relief, the first line local treatment is the 5% lidocaine-medicated plaster which provides local relief. Capsaicin 8% patch is considered a promising topical treatment for diabetic peripheral neuropathy. The present study investigated the efficacy, safety and tolerability of capsaicin 8% patch vs 5% lidocaine patch treatments over 24 weeks in South Asian male diabetic patients with established peripheral diabetic neuropathy.
Methods
Analgesic effectiveness was assessed by observing any change in the Numeric Pain Rating Scale (NPRS) score, Brief Pain Inventory (BPI) for painful diabetic peripheral neuropathy (BPI-DPN question 4) and Patient Global Impression of Change (PGIC). All patients received 4% lidocaine gel/cream for 60 min prior to patch application. The trial was probably underpowered, taking into account the smaller than expected number of participants from the calculated 350 sample size required for the whole study. Two hundred ninety-one individuals were divided into three groups based on treatment regimen; Group LL (Lidocaine + Lidocaine), Group LP (Lidocaine + Placebo), Group LC (Lidocaine + Capsaicin). The treatment procedure was conducted once initially and then repeated once at 12 weeks. The patients were followed up on alternate weeks till 24 weeks after the initial treatment.
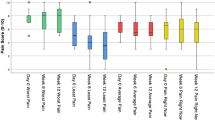
Results
Group LC experienced a more significant reduction in the average pain intensity (p < 0.05) during the last twenty-four hours. Group LC showed more significant reduction of pain compared to control (p < 0.01), a baseline score of 5.4 ± 1.2 dropped to 3.2 ± 1.5 by week 24 of treatment. The change in mean daily pain intensity was – 2.2 ± 1.5 [95% CI: −2.45, −1.5]. Group LL and LC experienced a significant overall improvement (slightly, much or very much) in the health status during the study. After the second week of the treatment, patient satisfaction scores were 2.1 ± 1.1 in Group LL which increased to 3.2 ± 1.2 by week 24 of treatment. The capsaicin 8% patch appears to be reasonably well tolerated since there were no discontinuations because of serious drug-related treatment emergent adverse event (TEAEs).
Conclusions
The aim of the present study was to assess the efficacy, safety and tolerability of the 8% capsaicin patch in patients with established painful diabetic neuropathy. There was a sustained treatment response to the initial and repeat treatment of the capsaicin 8% patch over the 24 weeks. The study population was very specific so further studies are required to investigate the generalizability of the results for patients experiencing painful diabetic neuropathy. The patch could be considered as an effective long-term treatment option in individuals with painful diabetic neuropathy, particularly those experiencing inadequate pain relief or side effects from systemic therapies.


Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author; N.H, upon reasonable request.
References
Aslam A, Singh J, Rajbhandari S. Pathogenesis of painful diabetic neuropathy. Pain Res Treat. 2014;2014:412041.
Albers JW, Pop-Busui R. Diabetic neuropathy: mechanisms, emerging treatments, and subtypes. Current Neurol Neurosci Reports. 2014;14(8):473–3.
Pop-Busui R, Boulton AJM, Feldman EL, Bril V, Freeman R, Malik RA, et al. Diabetic neuropathy: a position statement by the American Diabetes Association. Diabetes Care. 2017;40(1):136–54.
Tsuji M, et al. Painful diabetic neuropathy in Japanese diabetic patients is common but underrecognized. Pain Res Treat. 2013;2013:318352.
Mick G, Correa-Illanes G. Topical pain management with the 5% lidocaine medicated plaster--a review. Curr Med Res Opin. 2012;28(6):937–51.
de Leon-Casasola OA, Mayoral V. The topical 5% lidocaine medicated plaster in localized neuropathic pain: a reappraisal of the clinical evidence. J Pain Res. 2016;9:67–79.
Finnerup NB, Attal N, Haroutounian S, McNicol E, Baron R, Dworkin RH, et al. Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurol. 2015;14(2):162–73.
Martini C, Yassen A, Olofsen E, Passier P, Stoker M, Dahan A. Pharmacodynamic analysis of the analgesic effect of capsaicin 8% patch (Qutenza) in diabetic neuropathic pain patients: detection of distinct response groups. J Pain Res. 2012;5:51–9.
Simpson DM, Robinson-Papp J, van J, Stoker M, Jacobs H, Snijder RJ, et al. Capsaicin 8% patch in painful diabetic peripheral neuropathy: a randomized, double-blind. Placebo-Controlled Study J Pain. 2017;18(1):42–53.
Vinik AI, Perrot S, Vinik EJ, Pazdera L, Jacobs H, Stoker M, et al. Capsaicin 8% patch repeat treatment plus standard of care (SOC) versus SOC alone in painful diabetic peripheral neuropathy: a randomised, 52-week, open-label, safety study. BMC Neurol. 2016;16(1):251.
European Medicines Agency (2013) Summary of Product Characteristics: Qutenza 179 mg cutaneous patch . Available from: https://www.ema.europa.eu/en/medicines/human/EPAR/qutenza. Accessed on 12 Jan 2020.
FDA Center for Drug Evaluation and Research. Medical review: Qutenza. MD: Silver Spring; 2009.
Hayman M, Kam PCA. Capsaicin: a review of its pharmacology and clinical applications. Current Anaesthesia Critic Care. 2008;19(5–6):338–43.
Chen X, Zhang J, Wang X. Hormones in pain modulation and their clinical implications for pain control: a critical review. Hormones. 2016;15(3):313–20.
Blackburn-Munro G, Blackburn-Munro R. Pain in the brain: are hormones to blame? Trends Endocrinol Metab. 2003;14(1):20–7.
Berlin JA, Glasser SC, Ellenberg SS. Adverse event detection in drug development: recommendations and obligations beyond phase 3. Am J Public Health. 2008;98(8):1366–71.
Binu VS, Mayya SS, Dhar M. Some basic aspects of statistical methods and sample size determination in health science research. Ayu. 2014;35(2):119–23.
Erdfelder E, Faul F, Buchner A. GPOWER: a general power analysis program. Behav Res Methods Instrum Comput. 1996;28(1):1–11.
Jensen TS, et al. Tolerability of the capsaicin 8% patch following pretreatment with lidocaine or tramadol in patients with peripheral neuropathic pain: a multicentre, randomized, assessor-blinded study. European J Pain (London, England). 2014;18(9):1240–7.
Cleeland CS, Ryan KM. Pain assessment: global use of the brief pain inventory. Ann Acad Med Singap. 1994;23(2):129–38.
Perrot S, Lanteri-Minet M. Patients' global impression of change in the management of peripheral neuropathic pain: clinical relevance and correlations in daily practice. Eur J Pain. 2019;23:1117–28.
Nilsson ME, Koke SC. Defining treatment-emergent adverse events with the medical dictionary for regulatory activities (MedDRA). Drug Inform J. 2001;35(4):1289–99.
Hartemann A, Attal N, Bouhassira D, Dumont I, Gin H, Jeanne S, Said G, Richard JL. Working Group on the Diabetic Foot from the French speaking Society of Diabetology. Painful diabetic neuropathy: diagnosis and management. Diabetes Metab. 2011;37(5):377–88. https://doi.org/10.1016/j.diabet.2011.06.003.
Stanos SP, Galluzzi KE. Topical therapies in the management of chronic pain. Postgrad Med. 2013;125(4 Suppl 1):25–33.
Pickering G, et al. Localized neuropathic pain: an expert consensus on local treatments. Drug Des Devel Ther. 2017;11:2709–18.
Hartemann A. et al. Painful Diabet Neuropathy: Diagnosis Manag. 2011;37(5):377–88.
Snyder MJ, Gibbs LM, Lindsay TJ. Treating painful diabetic peripheral neuropathy: an update. Am Fam Physician. 2016;94(3):227–34.
Barbano RL, Herrmann DN, Hart-Gouleau S, Pennella-Vaughan J, Lodewick PA, Dworkin RH. Effectiveness, tolerability, and impact on quality of life of the 5% lidocaine patch in diabetic polyneuropathy. Arch Neurol. 2004;61(6):914–8.
van Nooten F, et al. Capsaicin 8% Patch Versus Oral Neuropathic Pain Medications for the Treatment of Painful Diabetic Peripheral Neuropathy: A Systematic Literature Review and Network Meta-analysis. Clin Ther. 2017;39(4):787–803.e18.
Ostrovsky DA. Single treatment with capsaicin 8% patch may reduce pain and sleep interference up to 12 weeks in patients with painful diabetic peripheral neuropathy. Explore (NY). 2017;13(5):351–3.
Uceyler N, Sommer C. High-dose capsaicin for the treatment of neuropathic pain: what we know and what we need to know. Pain Ther. 2014;3(2):73–84.
Burness CB, McCormack PL. Capsaicin 8% patch: a review in peripheral neuropathic pain. Drugs. 2016;76(1):123–34.
Haanpaa M, et al. Capsaicin 8% patch versus oral pregabalin in patients with peripheral neuropathic pain. Eur J Pain. 2016;20(2):316–28.
Hansson P, Jensen TS, Kvarstein G, Strömberg M. Pain-relieving effectiveness, quality of life and tolerability of repeated capsaicin 8% patch treatment of peripheral neuropathic pain in Scandinavian clinical practice. Eur J Pain. 2018;22(5):941–50.
Webster LR, Peppin JF, Murphy FT, Lu B, Tobias JK, Vanhove GF. Efficacy, safety, and tolerability of NGX-4010, capsaicin 8% patch, in an open-label study of patients with peripheral neuropathic pain. Diabetes Res Clin Pract. 2011;93(2):187–97.
Simpson DM, Gazda S, Brown S, Webster LR, Lu SP, Tobias JK, et al. Long-term safety of NGX-4010, a high-concentration capsaicin patch, in patients with peripheral neuropathic pain. J Pain Symptom Manag. 2010;39(6):1053–64.
Mankowski C, Poole CD, Ernault E, Thomas R, Berni E, Currie CJ, et al. Effectiveness of the capsaicin 8% patch in the management of peripheral neuropathic pain in European clinical practice: the ASCEND study. BMC Neurol. 2017;17(1):80.
Acknowledgments
We thank Dr. Fatima, Dr. Bilal and Dr. Zahra for their work and support.
Funding
The study received the hospital research grant approved by the Punjab Care Hospital Research Council [IAC-0457]. The funders did not have any role in the study design, execution, data collection or analysis and in the manuscript preparation or editing.
Author information
Authors and Affiliations
Contributions
N.H. and A.S.A.S, contributed to the design and implementation of the research. Z.K supervised the work and contributed in data collection and processing. F.J, A.H.I.A.A contributed to the analysis of the results. M.A and A.A.M contributed to the writing of the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest/competing interests
The authors all declare that there is conflict of interest. The research grant was not obtained from any pharmaceutical company or supplier and no author was a member of any study sponsor source.
Ethical approval
The study was approved by the Punjab Care hospital review board (Approval no. 38920), conducted in agreement with the ethical guidelines of the Declaration of Helsinki, Good Clinical Practice guidelines, and applicable regulatory requirement.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
All authors are in agreement to proceed for publication of this manuscript.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hussain, N., Said, A.S.A., Javaid, F.A. et al. The efficacy and safety profile of capsaicin 8% patch versus 5% Lidocaine patch in patients with diabetic peripheral neuropathic pain: a randomized, placebo-controlled study of south Asian male patients. J Diabetes Metab Disord 20, 271–278 (2021). https://doi.org/10.1007/s40200-021-00741-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-021-00741-2