Abstract
Purpose of Review
Pelvic floor dysfunction is an often overlooked cause of buttock pain in the athlete. Literature on pelvic floor dysfunction in athletes is limited, and therefore, it is frequently missed on evaluation and left untreated. This purpose of this article is to review the role that pelvic floor dysfunction plays in several musculoskeletal conditions experienced by athletes and to discuss pertinent history and physical examination findings that will help healthcare providers identify and treat athletes with pelvic floor dysfunction.
Recent Findings
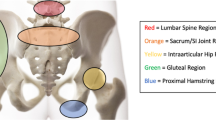
Recent studies show the prevalence of pelvic floor dysfunction in athletes is higher than one might expect. Structural changes in pelvic floor muscles have been identified in athletes, although the effect of these changes on pelvic floor function is not clear. Muscles of the pelvic floor are involved in controlling motion at the hip, sacroiliac joint and lumbar spine. Dysfunction in these muscles may contribute to a number of conditions that present with buttock pain.
Summary
It is important to recognize pelvic floor dysfunction as a potential cause of buttock pain in athletes, particularly in cases that have remained refractory to other conservative therapies.

Similar content being viewed by others
References
Eickmeyer SM. Anatomy and physiology of the pelvic floor. Phys Med Rehabil Clin N Am. 2017;28:455–60. https://doi.org/10.1016/j.pmr.2017.03.003.
Barber MD, Bremer RE, Thor KB, Dolber PC, Kuehl TJ, Coates KW. Innervation of the female levator ani muscles. Am J Obstet Gynecol. 2002;187:64–71.
Prather H, Spitznagle TM, Dugan SA. Recognizing and treating pelvic pain and pelvic floor dysfunction. Phys Med Rehabil Clin N Am. 2007;18:477–96, ix. https://doi.org/10.1016/j.pmr.2007.06.004.
Wallace K. Female pelvic floor functions, dysfunctions, and behavioral approaches to treatment. Clin Sports Med. 1994;13:459–81.
Prather H, Dugan S, Fitzgerald C, Hunt D. Review of anatomy, evaluation, and treatment of musculoskeletal pelvic floor pain in women. PM R. 2009;1:346–58. https://doi.org/10.1016/j.pmrj.2009.01.003.
Prather H. Pelvis and sacral dysfunction in sports and exercise. Phys Med Rehabil Clin N Am. 2000;11:805–36. viii
Bennis S, Hwang S. Office evaluation of pelvic pain. Phys Med Rehabil Clin N Am. 2017;28:461–76. https://doi.org/10.1016/j.pmr.2017.03.012.
Laycock J, Brown J, Cusack C, Green S, Jerwood D, Mann K, et al. Pelvic floor reeducation for stress incontinence: comparing three methods. Br J Commun Nurs. 2001;6:230–7. https://doi.org/10.12968/bjcn.2001.6.5.7083.
Khatri G, Khan A, Raval G, Chhabra A. Diagnostic evaluation of chronic pelvic pain. Phys Med Rehabil Clin N Am. 2017;28:477–500. https://doi.org/10.1016/j.pmr.2017.03.004.
Cho H-M, Park D-S, Kim DH, Nam H-S. Diagnosis of ilioinguinal nerve injury based on electromyography and ultrasonography: a case report. Ann Rehabil Med. 2017;41:705–8. https://doi.org/10.5535/arm.2017.41.4.705.
Roberts MM, Park TA. Pelvic floor function/dysfunction and electrodiagnostic evaluation. Phys Med Rehabil Clin N Am. 1998;9:831–51. vii
Casey EK, Temme K. Pelvic floor muscle function and urinary incontinence in the female athlete. Phys Sportsmed. 2017;45:399–407. https://doi.org/10.1080/00913847.2017.1372677.
Nygaard IE, Thompson FL, Svengalis SL, Albright JP. Urinary incontinence in elite nulliparous athletes. Obstet Gynecol. 1994;84:183–7.
Eliasson K, Larsson T, Mattsson E. Prevalence of stress incontinence in nulliparous elite trampolinists. Scand J Med Sci Sports. 2002;12:106–10.
Yi J, Tenfelde S, Tell D, Brincat C, Fitzgerald C. Triathlete risk of pelvic floor disorders, pelvic girdle pain, and female athlete triad. Female Pelvic Med Reconstr Surg. 2013;22:373–6. https://doi.org/10.1097/SPV.0000000000000296.
Kruger JA, Heap SW, Murphy BA, Dietz HP. Pelvic floor function in nulliparous women using three-dimensional ultrasound and magnetic resonance imaging. Obstet Gynecol. 2008;111:631–8. https://doi.org/10.1097/AOG.0b013e3181655dc2.
Roza TD, Brandão S, Oliveira D, Mascarenhas T, Parente M, Duarte JA, et al. Football practice and urinary incontinence: relation between morphology, function and biomechanics. J Biomech. 2015;48:1587–92. https://doi.org/10.1016/j.jbiomech.2015.03.013.
Borin LCMS, Nunes FR, Guirro ECO. Assessment of pelvic floor muscle pressure in female athletes. PM R. 2013;5:189–93. https://doi.org/10.1016/j.pmrj.2012.09.001.
Middlekauff ML, Egger MJ, Nygaard IE, Shaw JM. The impact of acute and chronic strenuous exercise on pelvic floor muscle strength and support in nulliparous healthy women. Am J Obstet Gynecol. 2016;215:316.e1–7. https://doi.org/10.1016/j.ajog.2016.02.031.
Leibovitch I, Mor Y. The vicious cycling: bicycling related urogenital disorders. Eur Urol. 2005;47:277–86; discussion 86-7. https://doi.org/10.1016/j.eururo.2004.10.024.
Papadopoulos EC, Khan SN. Piriformis syndrome and low back pain: a new classification and review of the literature. Orthop Clin N Am. 2004;35:65–71. https://doi.org/10.1016/S0030-5898(03)00105-6.
Menu P, Fouasson-Chaillou A, Dubois C, Dauty M. Piriformis syndrome diagnosis: on two professional cyclists. Ann Phys Rehabil Med. 2014;57:268–74. https://doi.org/10.1016/j.rehab.2014.02.006.
Kay J, de Sa D, Morrison L, Fejtek E, Simunovic N, Martin HD, et al. Surgical Management of Deep Gluteal Syndrome Causing Sciatic Nerve Entrapment: a systematic review. Arthroscopy. 2017;33:2263–78e1. https://doi.org/10.1016/jarthro201706.041.
Hopayian K, Song F, Riera R, Sambandan S. The clinical features of the piriformis syndrome: a systematic review. Eur Spine J. 2010;19:2095–109. https://doi.org/10.1007/s00586-010-1504-9.
Heiderscheit B, Evaluation MCS. Management of hip and pelvis injuries. Phys Med Rehabil Clin N Am. 2016;27:1–29. https://doi.org/10.1016/j.pmr.2015.08.003.
Foye PM. Coccydynia: tailbone pain. Phys Med Rehabil Clin N Am. 2017;28:539–49. https://doi.org/10.1016/j.pmr.2017.03.006.
Ryder I, Alexander J. Coccydynia: a woman's tail. Midwifery. 2000;16:155–60. https://doi.org/10.1054/midw.1999.0205.
Dampc B, Słowiński K. Coccygodynia pathogenesis, diagnostics and therapy. Review of the writing. Polski przeglad chirurgiczny. 2017;89:33–40. https://doi.org/10.5604/01.3001.0010.3909.
Demircay E, Kabatas S, Cansever T, Yilmaz C, Tuncay C, Altinors N. Radiofrequency thermocoagulation of ganglion impar in the management of coccydynia: preliminary results. Turk Neurosurg. 2010;20:328–33. https://doi.org/10.5137/1019-5149.JTN.2852-09.0.
Finsen V. Corticosteroid injection for coccygodynia. Tidsskrift for den Norske laegeforening: tidsskrift for praktisk medicin, ny raekke. 2001;121:2832–3.
Maigne JY, Chatellier G. Comparison of three manual coccydynia treatments: a pilot study. Spine. 2001;26:E479–83. discussion E84
Scott KM, Fisher LW, Bernstein IH, Bradley MH. The treatment of chronic coccydynia and postcoccygectomy pain with pelvic floor physical therapy. PM R. 2017;9:367–76. https://doi.org/10.1016/j.pmrj.2016.08.007.
Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat. 2012;221:537–67. https://doi.org/10.1111/j.1469-7580.2012.01564.x.
Peebles R, Jonas CE. Sacroiliac joint dysfunction in the athlete: diagnosis and management. Curr Sports Med Rep. 2017;16(5):336–42. https://doi.org/10.1249/JSR.0000000000000410.
Fortin JD, Washington WJ, Falco FJ. Three pathways between the sacroiliac joint and neural structures. AJNR Am J Neuroradiol. 1999;20(8):1429–34.
Bharucha AE, Lee TH. Anorectal and pelvic pain. Mayo Clin Proc. 2016;91:1471–86. https://doi.org/10.1016/j.mayocp.2016.08.011.
Rao SS, Bharucha AE, Chiarioni G, Felt-Bersma R, Knowles C, Malcolm A, et al. Functional anorectal disorders. Gastroenterology. 2016;150:1430–1442.e4. https://doi.org/10.1053/j.gastro.2016.02.009.
Montenegro ML, Mateus-Vasconcelos EC, Rosa e Silva JC, Nogueira AA, Dos Reis FJ, Poli Neto OB. Importance of pelvic muscle tenderness evaluation in women with chronic pelvic pain. Pain Med (Malden, Mass). 2010;11:224–8. https://doi.org/10.1111/j.1526-4637.2009.00758.x.
Gyang A, Hartman M, Lamvu G. Musculoskeletal causes of chronic pelvic pain: what a gynecologist should know. Obstet Gynecol. 2013;121:645–50. https://doi.org/10.1097/AOG.0b013e318283ffea.
Kotarinos R. Myofascial pelvic pain. Curr Pain Headache Rep. 2012;16:433–8. https://doi.org/10.1007/s11916-012-0277-8.
Spitznagle TM, Robinson CM. Myofascial pelvic pain. Obstet Gynecol Clin N Am. 2014;41:409–32. https://doi.org/10.1016/j.ogc.2014.04.003.
Bonder JH, Chi M, Rispoli L. Myofascial pelvic pain and related disorders. Phys Med Rehabil Clin N Am. 2017;28:501–15. https://doi.org/10.1016/j.pmr.2017.03.005.
Sikdar S, Shah JP, Gebreab T, Yen R-H, Gilliams E, Danoff J, et al. Novel applications of ultrasound technology to visualize and characterize myofascial trigger points and surrounding soft tissue. Arch Phys Med Rehabil. 2009;90:1829–38. https://doi.org/10.1016/j.apmr.2009.04.015.
Turo D, Otto P, Shah JP, Heimur J, Gebreab T, Zaazhoa M, et al. Ultrasonic characterization of the upper trapezius muscle in patients with chronic neck pain. Ultrason Imaging. 2013;35:173–87. https://doi.org/10.1177/0161734612472408.
Chen Q, Basford J, An K-N. Ability of magnetic resonance elastography to assess taut bands. Clin Biomech (Bristol, Avon). 2008;23:623–9. https://doi.org/10.1016/j.clinbiomech.2007.12.002.
Chen Q, Wang H-J, Gay RE, Thompson JM, Manduca A, An K-N, et al. Quantification of myofascial taut bands. Arch Phys Med Rehabil. 2016;97:67–73. https://doi.org/10.1016/j.apmr.2015.09.019.
Itza F, Zarza D, Salinas J, Teba F, Ximenez C. Turn-amplitude analysis as a diagnostic test for myofascial syndrome in patients with chronic pelvic pain. Pain Res Manag. 2015;20:96–100.
Moldwin RM, Fariello JY. Myofascial trigger points of the pelvic floor: associations with urological pain syndromes and treatment strategies including injection therapy. Curr Urol Rep. 2013;14:409–17. https://doi.org/10.1007/s11934-013-0360-7.
FitzGerald MP, Kotarinos R. Rehabilitation of the short pelvic floor. II: Treatment of the patient with the short pelvic floor. Int Urogynecol J Pelvic Floor Dysfunct. 2003;14:269–75; discussion 75. https://doi.org/10.1007/s00192-003-1050-7.
Elkins N, Hunt J, Scott KM. Neurogenic Pelvic Pain. Phys Med Rehabil Clin N Am. 2017;28:551–69. https://doi.org/10.1016/j.pmr.2017.03.007.
Labat J-J, Robert R, Delavierre D, Sibert L, Rigaud J. Symptomatic approach to chronic neuropathic somatic pelvic and perineal pain. Progres en urologie. 2010;20:973–81. https://doi.org/10.1016/j.purol.2010.08.062.
Antolak SJ, Hough DM, Pawlina W, Spinner RJ. Anatomical basis of chronic pelvic pain syndrome: the ischial spine and pudendal nerve entrapment. Med Hypotheses. 2002;59:349–53.
Benson JT, Griffis K. Pudendal neuralgia, a severe pain syndrome. Am J Obstet Gynecol. 2005;192:1663–8. https://doi.org/10.1016/j.ajog.2005.01.051.
Stav K, Dwyer PL, Roberts L. Pudendal neuralgia. Fact or fiction? Obstet Gynecol Surv. 2009;64:190–9.
Filler AG. Diagnosis and treatment of pudendal nerve entrapment syndrome subtypes: imaging, injections, and minimal access surgery. Neurosurg Focus. 2009;26:E9. https://doi.org/10.3171/FOC.2009.26.2.E9.
Labat JJ, Riant T, Lassaux A, Rioult B, Rabischong B, Khalfallah M, et al. Adding corticosteroids to the pudendal nerve block for pudendal neuralgia: a randomised, double-blind, controlled trial. BJOG. 2017;124:251–60. https://doi.org/10.1111/1471-0528.14222.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Sports Medicine Rehabilitation
Rights and permissions
About this article
Cite this article
Yuan, X., Bevelaqua, AC. Buttock Pain in the Athlete: the Role of Pelvic Floor Dysfunction. Curr Phys Med Rehabil Rep 6, 147–155 (2018). https://doi.org/10.1007/s40141-018-0188-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40141-018-0188-7