Abstract
Anesthetic management during cardiopulmonary bypass (CPB) is challenging in many aspects. Evidence of mortality reduction due to the use of volatile agents during cardiac surgery has led to their increased use in CPB. Partly because of the difficulty to administer volatile agents during CPB, total intravenous anesthesia (TIVA) has become the most popular technique used by cardiac anesthetists throughout this critical period. The aim of this review is to provide an overview of volatile agents’ administration to ensure maintenance of adequate depth of anesthesia during CPB and weighting risks and benefits of this technique compared to TIVA.





Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Nordén I. The influence of anaesthetics on systemic vascular resistance during cardiopulmonary bypass. Scand J Thorac Cardiovasc Surg. 1974;8:81–7.
Landoni G, Rodseth RN, Santini F, et al. Randomized evidence for reduction of perioperative mortality. J Cardiothorac Vasc Anesth. 2012;26:764–72.
De Hert SG, Vander Linden PJ, Cromheecke S, et al. Cardioprotective properties of sevoflurane in patients undergoing coronary surgery with cardiopulmonary bypass are related to the modalities of its administration. Anesthesiology. 2004;101:299–310.
Nussmeier NA, Moskowitz GJ, Weiskopf RB, et al. In vitro anesthetic washin and washout via bubble oxygenators: influence of anesthetic solubility and rates of carrier gas inflow and pump blood flow. Anesth Analg. 1988;67:982–7.
•• McMullan V, Alston RP, Tyrrell J. Volatile anaesthesia during cardiopulmonary bypass. Perfusion. 2015;30(1):6–16. Published in 2015, a complete review of administering and ensuring anesthesia with VAA during CPB.
Langbein T, Sonntag H, Trapp D, et al. Volatile anaesthetics and the atmosphere: atmospheric life times and atmospheric effects of halothane, enflurane, isoflurane, desflurane and sevoflurane. Br J Anaesth. 1999;82:66–73.
Yasny JS, White J. Environmental implications of anesthetic gases. Anesth Prog. 2012;59:154–8.
Nigro Neto C, Arnoni R, Rida BS, Landoni G, Tardelli MA. Randomized trial on the effect of sevoflurane on polypropylene membrane oxygenator performance. J Cardiothorac Vasc Anesth. 2013;27(5):903–7.
•• Nigro Neto C, De Simone F, Cassara L, Silva CGS, Cardoso TAAM, Carco F, et al. Tricks, tips, and literature review on the adapted vaporize system to deliver volatile agents during cardiopulmonary bypass. Ann Card Anaesth. 2016;19(2):240–4. A review examining technical aspects of correct adaptation of vaporizers to CPB circuits.
Lim HS, Cho SH, Kim DK, et al. Isoflurane cracks the polycarbonate connector of extra-corporeal circuit: a case report. Korean J Anesth. 2010;58:304–6.
Nigro Neto C, Landoni G, Cassarà L, De Simone F, Zangrillo A, Tardelli MA. Use of volatile anesthetics during cardiopulmonary bypass: a systematic review of adverse events. J Cardiothorac Vasc Anesth. 2014;28(1):84–9.
Nitzschke R, Wilgusch J, Kersten JF, Trepte CJ, Haas SA, Reuter DA, et al. Changes in sevoflurane plasma concentration with delivery through the oxygenator during on-pump cardiac surgery. Br J Anaesth. 2013;110:957–65.
•• Landoni G, Pisano A, Lomivorotov V, Alvaro G, Hajjar L, Paternoster G, Nigro Neto C et al: Randomized evidence for reduction of perioperative mortality: an updated consensus process. J Cardiothorac Vasc Anesth. 2016 pii: S1053–0770(16)30281–6. Summary of a web-based international consensus conference comprising clinicians from 61 countries.
•• Likhvantsev VV, Landoni G, Levikov DI, Grebenchikov OA, Skripkin YV, Cherpakov RA. Sevoflurane versus total intravenous anesthesia for isolated coronary artery bypass surgery with cardiopulmonary bypass: a randomized trial. J Cardiothorac Vasc Anesth. 2016;30(5):1221–7. The largest randomized controlled trial comparing VAA and TIVA in cardiac surgery.
Schmid E, Krajewski S, Bachmann D, Kurz J, Wendel HP, Rosenberger P, et al. The volatile anesthetic sevoflurane inhibits activation of neutrophil granulocytes during simulated extracorporeal circulation. Int Immunopharmacol. 2012;14(2):202–8.
Medtronic. Medtronic manual. User manual: medtronic affinity fusion oxygenator. 2012.
Boiano JM, Steege AL. Precautionary practices for administering anesthetic gases: a survey of physician anesthesiologists, nurse anesthetists and anesthesiologist assistants. J Occup Environ Hyg. 2016;13(10).
Byhahn C, Wilke HJ, Westphal K. Occupational exposure to volatile anaesthetics epidemiology and approaches to reducing the problem. Mol Diag Ther. 2001;15:197.
Mierdl S, Byhahn C, Abdel-Rahman U, et al. Occupational exposure to inhalational anaesthetics during cardiac surgery on cardiopulmonary bypass. Ann Thorac Surg. 2003;75:1924–8.
Blokker-Veldhuis MJ, Rutten PM, De Hert SG. Occupational exposure to sevoflurane during cardiopulmonary bypass. Perfusion. 2011;26:383–9.
• Nigro Neto C, Landoni G, Tardelli MA. A novel anti-pollution filter for volatile agents during cardiopulmonary bypass: preliminary tests. J Cardiothorac Vasc Anesth. 2017. A successful step towards a new scavenging system, proving ex-vivo efficiency of an activated charcoal filter.
Schoen J, Husemann L, Tiemeyer C, et al. Cognitive function after sevoflurane-vs propofol-based anaesthesia for on-pump cardiac surgery: a randomized controlled trial. Br J Anaesth. 2011;106(6):840–50.
Alston RP, Anes FR, Tierney C, et al. Isoflurane and hypothermic cardiopulmonary bypass: vasodilation without metabolic effects. J Cardiothorac Vasc Anesth. 1992;6:700–4.
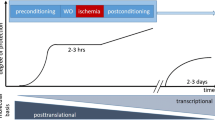
Hausenloy DJ, Boston-Griffiths E, Yellon DM. Cardioprotection during cardiac surgery. Cardiovasc Res. 2012;94:253–65.
Heusch G. Cardioprotection: chances and challenges of its translation to the clinic. Lancet. 2013;381:166–75.
Hillis LD, Smith PK, Anderson JL, et al. 2011 ACCF/AHA guideline for coronary artery bypass graft surgery: Executive Summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2011;124:2610–42.
Fleisher LA, Beckman JA, Brown KA, et al. ACC/AHA 2007 Guidelines on perioperative cardiovascular evaluation and care for noncardiac surgery: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery): developed in collaboration with the American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Rhythm Society, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, and Society for Vascular Surgery. Circulation. 2007;116:1971–96.
Bantel C, Maze M, Trapp S. Neuronal preconditioning by inhalational anesthetics: evidence for the role of plasmalemmal adenosine triphosphate-sensitive potassium channels. Anesthesiology. 2009;110(5):986–95.
Freiermuth D, Mets B, Bolliger D, Reuthebuch O, Doebele T, Scholz M, et al. Sevoflurane and isoflurane—pharmacokinetics, hemodynamic stability, and cardioprotective effects during cardiopulmonary bypass. J Cardiothorac Vasc Anesth. 2016;30(6):1494–501.
Kawamura T, Kadosaki M, Nara N, Kaise A, Suzuki H, Endo S, et al. Effects of sevoflurane on cytokine balance in patients undergoing coronary artery bypass graft surgery. J Cardiothorac Vasc Anesth. 2006;20(4):503–8.
Rödig G, Keyl C, Wiesner G, Philipp A, Hobbhahn J. Effects of sevoflurane and isoflurane on systemic vascular resistance: use of cardiopulmonary bypass as a study model. Br J Anaesth. 1996;76(1):9–12.
• Güçlü ÇY, Ünver S, Aydinli B, Kazanci D, Dilber E, Özgök A. The effect of sevoflurane vs. TIVA on cerebral oxygen saturation during cardiopulmonary bypass—randomized trial. Adv Clin Exp Med. 2014;23(6):919–24. The primary randomized trial comparing the effects of sevoflurane vs TIVA on cerebral protection during CPB.
Smith S, Scarth E, Sasada M. Drugs in anaesthesia and intensive care. 4th ed. Oxford: Oxford University Press; 2011.
Borisov KY, Moroz VV, Grebenchikov OA, et al. Effect of propofol on sevoflurane-induced myocardial preconditioning in the experiment. Gen Reanimatol. 2013;IX:30–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Caetano Nigro Neto, Giovanni Landoni, Francisco José Lucena Bezerra, Thiago Maranhão, Carlos Gustavo, and Adriene Stahlschmidt declare they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
The original version of this article was revised: The original version of this article unfortunately contained a mistake in the Author group section. ‘Thiago Augusto Almeida Maranhão Cardoso’ should be ‘Thiago Augusto Azevedo Maranhão Cardoso.’
This article is part of the Topical Collection on Cardiovascular Anesthesia
Rights and permissions
About this article
Cite this article
Nigro Neto, C., Landoni, G., Bezerra, F.J.L. et al. Anesthesia Management During Cardiopulmonary Bypass: Volatile vs. Intravenous Drugs. Curr Anesthesiol Rep 7, 299–305 (2017). https://doi.org/10.1007/s40140-017-0222-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40140-017-0222-9