Abstract
Purpose of Review
Bilateral vocal fold immobility is a challenging life-threatening problem involving multiple treatment options and nuanced clinical decision making. We aim to provide relevant background on the etiology, diagnosis, and management of bilateral vocal fold movement impairment (BVFMI).
Recent Findings
Over the last 20 years, the management of bilateral vocal fold immobility has advanced significantly with the addition of multiple endoscopic approaches as well as procedures with the goal of returning dynamic function to the larynx, among them: selective reinnervation. Chemodenervation has also demonstrated promising results as a temporizing procedure in appropriately selected patients with BVFMI.
Summary
Tracheostomy remains the mainstay of emergent treatment for airway obstruction secondary to bilateral vocal fold immobility. However, recent advances in endoscopic approaches allow for avoidance of tracheostomy in many patients. Developments in dynamic procedures with the aim of restoring laryngeal function allow for adequate airway management while maintaining voice quality and limiting aspiration risk.
Similar content being viewed by others
Introduction
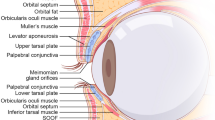
Vocal fold function is crucial for survival. Impairment can result in dysphagia, aspiration, and most notably airway obstruction particularly when both vocal folds are involved [1]. Awake laryngoscopy provides a key tool for the assessment of vocal fold function and mobility. Decreased mobility is often labeled as paralysis or paresis, but these labels specifically refer to a lower motor neuron dysfunction contributing to absent or abnormal vocal fold mobility. In reality, vocal fold movement is much more complex, and motion impairment may occur due to dysfunctional innervation resulting in laryngeal synkinesis and not complete denervation [2]. As a result, a better term to describe vocal fold “paralysis” is “vocal fold movement impairment.”
Bilateral vocal fold movement impairment (BVFMI) can be life threatening especially if the onset is acute. Initial management frequently consists of intubation or a tracheostomy to secure the airway [3]. Sometimes the voice is normal or near normal, though significant dyspnea and even overt biphasic stridor can occur. The problem can begin suddenly, such as on extubation after thyroidectomy, or it can develop insidiously [4]. An overview of the problem of BVFMI will be given, with emphasis on the variety of treatment options for management of BVFMI from infant to adult.
Etiologies (Table 1)
The most common causes of BVFMI differ between adults and children. Adults often present with new onset vocal fold immobility most commonly secondary to surgical trauma. Previous reviews have demonstrated 25–58% of BVFMI cases occur following surgery. Thyroidectomy is the most common surgery to result in BVFMI with parathyroid surgery being the second most common surgical procedure. Malignancy is the second most common etiology of acquired BVFMI ranging from 7 to 17% of cases [1, 5,6,7]. Intubation is also a common factor contributing to BVFMI and is thought to contribute to 2–18% of cases. A central nervous system disease or tumor can also result in bilateral vocal fold paralysis. Other important factors to consider in adults should include non-surgical trauma, rheumatoid arthritis, other autoimmune diseases, radiation therapy, and infection. Finally, when a cause cannot be identified, idiopathic bilateral vocal fold immobility occurs in 3–13% of cases [1, 6,7,8].
Unlike adults, congenital BVFMI is most commonly related to an underlying central nervous system (CNS) disorder. The most common CNS abnormality contributing to bilateral vocal fold paralysis is an Arnold-Chiari malformation [9]. Central neural degenerative disease including syringomyelia and syringobulbia is also associated with BVFMI [10, 11]. Additional CNS causes of vocal fold immobility include leukodystrophy, encephalocele, hydrocephalus, and cerebral or nuclear dysgenesis [12, 13]. Peripheral disorders such as congenital myasthenia gravis have also been implicated in congenital BVFMI although this is much more likely to occur in older children and adults [14, 15].
Similar to adults, surgical trauma in children can contribute to vocal fold immobility. Any procedure with close proximity to the recurrent laryngeal nerve has the added risk of vocal fold paralysis. Surgical trauma in infants generally results in unilateral immobility, but patients undergoing tracheoesophageal fistula (TEF) repair, especially H-type TEF, are at risk of developing bilateral vocal fold immobility [16]. Blunt trauma resulting in closed head injuries, especially involving the posterior fossa, can also contribute to bilateral vocal fold immobility [17].
Metabolic and toxic etiologies should also be considered in the differential for BVFMI. Bilateral vocal fold immobility has been associated with hypokalemia as well as organophosphate poisoning [18, 19]. Additionally, vocal fold immobility, both unilateral and bilateral, has been described as an adverse effect of vincristine with a dose-related response that resolves slowly after discontinuation of the medication [20].
Although rare, a variety of genetic syndromes associated with familial vocal fold paralysis have been described [21,22,23,24]. Hsu et al. reviewed the literature and found a number of genetic syndromes associated with bilateral neonatal and adult onset vocal fold immobility. Most notably a specific balanced translocation between chromosomes 5 and 14 is associated with an autosomal dominant inheritance of neonatal BVFMI [25]. A separate report of 21 cases of familial BVFMI identified a variety of inheritance patterns including autosomal dominant, X-linked dominant, and X-linked recessive [24]. Additionally, conditions such as 22q11 deletion or Robinow syndromes have also been associated with congenital BVFMI [26].
Bilateral vocal fold immobility has also been associated with inflammatory conditions related to underlying infections and granulomatous diseases. There are reports of patients infected with polio, tuberculosis, cytomegalovirus, West Nile virus, and herpes simplex virus presenting with bilateral vocal fold immobility [27,28,29,30,31]. Although Guillain-Barré syndrome rarely affects laryngeal function, it has been associated with bilateral vocal fold immobility when laryngeal function is compromised [6, 32].
Presentation and Diagnostic Evaluation
The most common manifestation of bilateral vocal fold paralysis is stridor [6]. These patients typically present with respiratory distress [33••]. In addition to considerable airway obstruction, BVFMI presents with symptoms common in unilateral vocal fold immobility such as ineffective cough, aspiration, recurrent pneumonia, reactive airway disease, and feeding difficulties [34••, 35]. Voice and cry may be fairly normal in children with BVFMI [36]. In a study by Jabbour examining 102 pediatric patients with BVFMI, 40% presented with dysphagia, and 51% required a gastrostomy tube [37].
Diagnosis is made by performing a thorough history and physical exam. First, a proper description of the effort of breathing including stridor should be completed. Second, speech and swallowing difficulties are evaluated. Any history of prior intubation or other surgical interventions should be documented. Associated medical conditions or congenital anomalies, such as neurologic disorders or congenital heart disease, must be investigated. Early diagnosis can be made by fiberoptic examination of the larynx, but a significant proportion of the children will need immediate intubation after birth due to intense respiratory distress [38]. Therefore, evaluation of the airway may require examination under general anesthesia with spontaneous ventilation [39]. Microlaryngoscopy should consist of visual inspection as well as palpation of the arytenoid to rule out cricoarytenoid fixation and close evaluation of the posterior glottis to rule out stenosis. Grading of the posterior glottic stenosis can be performed using the Bogdasarian classification [40]. Diagnosis can occasionally require laryngeal EMG. If volitional activity is present, late spontaneous recovery is possible and can be anticipated [41••].
Management
Management of BVFMI requires a multidisciplinary approach including intensivists, skilled otolaryngologists, and speech-language pathologists. The primary treatment is to provide a safe airway that does not compromise the patient’s life. The main decision is the need for tracheotomy. On average 19.2–74% of BVFMI patients will require a surgical airway [37, 38, 42, 43]. However, some small case series describe a 0% need for tracheotomy [44, 45], and other small series show a 90–100% need for a tracheotomy [13, 41••]. This range reflects much variation in provider’s management of BVFMI.
Improvements in neonatal care, the assessment and monitoring of apnea, and use of nasal CPAP or high-flow air by nasal cannula may be helpful in decreasing the need for tracheotomies in children. These tools might help providers “buy time” since spontaneous recovery has been shown to occur in 50–65% of pediatric patients [38, 42, 43]. This recovery can occur in as little as 5 months to more than 3 years after the initial diagnosis or birth [46, 47]. However, if patients are unable to remain extubated, then a tracheotomy may be warranted [38].
The evaluation of BVFMI usually involves neurological assessment, imaging studies [48], and swallowing studies [49]. Oral feeding can exacerbate obstruction and airway symptoms in these patients. A nasogastric (NG) tube can help relieve these symptoms; one study reported 73% of BVFMI require NG tube feeding [38]. Gastrostomy tube feedings can also be necessary to relieve patients from the need of prolonged NG feeding. Jabbour and colleagues showed that 51% of patients with BVFMI required insertion of gastrostomy tubes [37].
Many centers believe that after 1 year, a chance for spontaneous recovery is low, and a procedure that can help decannulation should be offered [45, 46, 50]. Other centers recommend waiting several years, for possible spontaneous recovery, before an irreversible procedure is attempted [16, 39]. Berkowitz suggested that patients with congenital BVFMI can have spontaneous recovery in their second quinquennium of life and can eventually be decannulated if they have a tracheostomy in place [47]. This might also depend on the etiology of injury with higher rate of spontaneous recovery in central neurologic injury and lowest rate in iatrogenic injuries [46]. A study on 102 patients by Funk showed that idiopathic causes for BVFMI demonstrated higher rates of resolution compared to patients with a neurogenic etiology (46.7% vs 14.3%) [51].
Patients that cannot be decannulated and who do not have spontaneous resolution of VFP have several options to have an improved airway patency. These options are divided into “static”, “chemical”, and “dynamic” approaches. Static procedures involve laryngeal framework surgery either by resection of tissue [33••, 52,53,54, 55••]. Laryngeal chemodenervation, another form of managing BVFMI, is performed by targeting the thyroarytenoid muscle [56] or the cricothyroid muscle using botulinum A injections [57]. Dynamic procedures include laryngeal reanimation procedures (e.g., reinnervation) and functional electrical stimulation.
Static Procedures
Static procedures improve airway patency by enlarging the glottic aperture. This can be accomplished either by excising laryngeal tissue, fixation techniques, or enlargement of glottic circumferential area. Multiple procedures can be employed simultaneously. The expected consequence of static procedures is a decline in voice quality in volume and roughness of the voice in a compromise for a larger glottic airway.
Cordotomy
Cordotomy with or without arytenoidectomy has been described in adults from 1983 using the carbon dioxide (CO2) laser [58]. Children have a smaller larynx, where the balance between voice and airway patency is very delicate and harder to predict. Cordotomy has been described in children with high success regarding airway, but voice outcomes have not been prospectively assessed. The procedure consists of an incision in the posterior third of the true vocal fold laterally to the thyroid cartilage [59]. Studies demonstrated 89 to 100% of patients treated with cordotomy were ultimately decannulated or avoided tracheotomy altogether [59, 60]. However, some patients require multiple revisions due to persistent symptoms of dyspnea. The voice is expected to be adversely affected; however, the degree of dysphonia and the effect on quality of life have not been prospectively addressed.
Arytenoidectomy
Endoscopic laser arytenoidectomy is another alternative and has a similarly high rate of success. The procedure consists of vaporization of the medial part of the arytenoid with preservation of the posterior-lateral mucosal wall [61]. In a study by Aubrey, 75% of patients were able to be decannulated at a mean of 2 months postoperatively. One of these patients required a cordotomy for recurrence of dyspnea. Out of the 17 patients treated, 5 had postoperative dyspnea, 3 improved with voice therapy, and 2 required vocal fold augmentation [61]. Another study showed success in treating 6 patients with arytenoidectomy without postoperative speech impairment [62].
Arytenoid Lateralization
Endoscopic percutaneous suture lateralization for bilateral vocal fold immobility has also been described in the literature and is recently gaining popularity especially in neonatal BVFMI [63]. Multiple methods can be used to perform this procedure including the use of ultrasound to guide suture placement [64]. Sztanó and colleagues demonstrated a 3/3 success rate with a greater than 3-year follow-up [65••]. Montague had a 5/5 success rate after excluding 1 patient that expired due to seizures. However, 1 patient had aspiration and had resolution of symptoms after suture removal [66].
Endoscopic Anterior-Posterior Cricoid Split
Another static method to enlarge the airway is the endoscopic anterior-posterior cricoid split. In this method, the posterior cricoid is incised first using a laryngeal knife or CO2 laser. The anterior cricoid is then incised through a mucosal incision made with a sharp sickle knife while exercising caution to avoid injury to the anterior commissure [33••]. Rutter demonstrated a 74% success rate overall with only 3 of 19 patients requiring tracheotomy following anterior-posterior cricoid split. Another more recent study on 6 patients showed a 50% success with the rest of the patients requiring tracheotomy [55••]. The procedure was reported to “not affect the voice” [33••] though voice outcomes were not measured or documented in either study.
Posterior Cricoid Cartilage Graft
Posterior cricoid cartilage graft has been performed for BVFMI by widening the posterior glottis [67]. A rib cartilage is harvested, carved, and placed in position after performing a posterior cricoid. This procedure has mixed results overall. A few studies demonstrated that 100% of patients were either decannulated or were able to avoid a tracheotomy [67,68,69]. In contrast, a study by Dahl showed a 2/7 rate of decannulation in patients with BVFMI [70••]. However, Dahl argues that this low rate of decannulation could be due to the possibility that each institution might have different protocols for decannulation [70••]. The potential for adverse voice outcomes after posterior cricoid graft laryngoplasty has documented from numerous retrospective studies. A breathy weak voice ensues from posterior glottis incompetence when the graft displaces the arytenoids too widely. Compensatory supraglottal phonation may develop. Cricoid reduction laryngoplasty to remediate this problem has been recently reported. [71]
Laryngeal Chemodenervation
Cohen first described the use of botulinum toxin for treatment of BVFMI in a canine model in the 1980s. Injection of the cricothyroid muscle was found to relax the tension of the true vocal fold resulting in lateralization with improvement of airway obstruction [57, 72]. Smith et al. later described the use of botulinum toxin injections to the thyroarytenoid muscle to treat 10 pediatric patients with BVFMI. In this study, 4 patients experienced improvement in airway obstruction sufficient enough to either avoid tracheostomy or facilitate decannulation. Of the 6 patients with no improvement, four had significant central nervous system comorbidities [73].
A more recent study described injection of onabotulinum toxin A into the cricothyroid muscle of 6 pediatric patients with BVFMI. All patients experienced improvement in airway obstruction within days of injection. Five patients avoided tracheostomy, and the 6th was successfully following treatment [74].
Lewis and Woo also described their experience using botulinum toxin injection in patients with BVFMI and underlying laryngeal synkinesis following iatrogenic injury [75••]. After injection of the TA and/or PCA, 5 of 8 patients experienced adequate improvement in dyspnea. Two patients were successfully decannulated following injections. Overall, botulinum toxin injection appears to be less effective than other treatments but can certainly provide benefit in appropriately selected patients. The obvious downside of this treatment option is the need for repeat injections to maintain results.
Reanimation Techniques
Laryngeal Reinnervation
While static procedures are successful approaches to managing the airway and ultimately can help with decannulation in patients with BVFMI, these procedures often result in worsening phonation and increased aspiration. In contrast, laryngeal reinnervation provides an alternative approach with the goal of improving both abduction and adduction of the bilateral vocal folds. Additionally, these procedures have the added benefit of being entirely extralaryngeal so there are no mucosal incision or changes to the laryngeal framework ultimately limiting the risk of laryngeal scarring and/or intraluminal granulation formation.
During the 1970s and 1980s, Tucker studied laryngeal reinnervation by ansa cervicalis nerve-muscle pedicle transfer to the posterior cricoarytenoid muscle in 202 patients with BVFMI. He reported long-term success in 74% of patients undergoing the procedure although only 50% of tracheostomy dependent children were ultimately decannulated [76, 77]. In 1998, Zheng et al. demonstrated in a canine model superior outcomes in reinnervation with the nerve suture technique (compared with direct nerve implant into muscle and nerve-muscle pedicle) in which the nerve graft is approximated to the adductor branch of the RLN using an epineural stitch with 11–0 nylon suture [78].
After several experiments, J.P. Marie developed a procedure consisting of bilateral selective reinnervation of the adductor and abductor muscles of the larynx [79]. From these, the necessity to use phrenic nerve roots to drive reinnervated inspiratory muscles was documented [80]. The paralyzed posterior cricoarytenoid (PCA) abductor muscles are reinnervated by grafting with the greater auricular nerve (GAN) Y-graft from a rootlet of the phrenic nerve directly implanting to each lateral PCA belly. The adductor muscles of the larynx on each side are reinnervated by the thyrohyoid nerve via a GAN jump graft and connected to the main RLN trunk. To date, long-term follow-up has been achieved in more than 80 adult patients, since 2013 (JP Marie, unpublished results). A recent study by Lee, Mardion, Smith, and Marie demonstrated promising outcomes in 8 pediatric patients with bilateral vocal fold paralysis [34••]. The median age at time of reinnervation was approximately 9 years. Six of the eight patients required preoperative tracheostomy for airway management. Long-term follow-up demonstrated decannulation of all patients with an average time to decannulation of just under 1 year after surgery. Vocal fold abduction on inspiration was observed in 7 patients, and the 8th patient demonstrated clinical improvement in respiratory function although no visible movement was noted on flexible laryngoscopy [34••]. This study demonstrates great promise for treatment of BVFMI with selective laryngeal reinnervation.
A group in China described success with a similar selective laryngeal reinnervation technique [81••]. The operation entails dissecting out the damaged RLNs and grafting the upper root of the right phrenic nerve to the common trunk of the RLN bilaterally. The branch to the interarytenoid muscle on each side is divided. Next, the thyroid branch of the hypoglossal nerve is anastomosed to the adductor branches of the RLNs on both sides. The group reported results on 7 patients with BVFMI post-thyroidectomy confirmed by EMG. In 6 of the 7 patients, there was return of function to both vocal folds, and at least one vocal fold demonstrated moderate to maximal movement. The 7th patient exhibited no movement on one side and minimal movement on the contralateral side. PFTs were also significantly improved and within the normal reference values 3 months after surgery.
Laryngeal Pacing
Given the previous success with implantable devices such as cardiac pacemakers, cochlear implants, and even hypoglossal nerve stimulators, recent studies have investigated the use of implantable devices in laryngeal pacing for treatment of BVFMI. In this surgery, the device electrode is implanted into the PCA muscle, and stimulation of abduction is confirmed intraoperatively. The implantable device is then placed in a subcutaneous pocket overlying the sternum [82••, 83]. A study by Zealear and colleagues evaluated 7 patients who underwent implantation of a laryngeal pacing device. Five patients had significant improvement particularly in their peak inspiratory flow measures at follow-up. Four patients met criteria for decannulation. Of the 2 failures, 1 patient had an infection of the implant requiring removal, and the other did not exhibit stimulated abduction after surgery [83]. More recently, Mueller reported results of a different implantable device in 9 adult patients with BVFMI [82••]. Of the 7 adult patients completing the study, a significant improvement in peak inspiratory and peak expiratory function was noted. There was no change in voice or swallowing parameters.
Although initial outcomes of laryngeal pacing are promising, there are a few notable disadvantages. First, the surgery requires an implantable device with the possibility of infection, extrusion, and failure. Second, the device does not have an inspiratory sensor and is not synchronized with the patient’s inspiratory effort. Programming is possible, but ultimately the patient must learn to adjust their respiratory rate to the programmed stimulus cycle [82••, 83]. Regardless, this approach shows considerable promise and will likely continue to improve with technological advances.
Conclusion (Figure 1)
BVFMI is a life-threatening disease especially in the pediatric population. Although a thorough history and physical exam are crucial in arriving at the appropriate diagnosis, securing the airway is the primary goal of the caring team. A multidisciplinary approach is vital in the long-term course of this disease. Breathing, swallowing, and speech are the three pillars that need to be balanced in order to improve the quality of life of the patients.
Treatment should be tailored according to each patient but also to the experience of the otorhinolaryngologist. As patients may experience spontaneous recovery, a trial of conservative treatment can be planned initially. When conservative measures fail, static procedures that are less vocally impairing or chemodenervation procedures can be tried. Additionally, some patients might require multiple procedures. Dynamic interventions provide promising alternatives to tracheostomy and static procedure. At this time, laryngeal reinnervation (in children and adults) and laryngeal pacing (in adults) provide excellent alternatives to more traditional techniques. When it is apparent that a surgical procedure with long-term improvement in airway is necessary, we first consider if the patient is a candidate for bilateral selective reinnervation. If not, or if laryngeal reinnervation is unsuccessful, then a long-term static procedure can be employed, such as a posterior cricoid cartilage graft. With continued research and further advances, the reinnervation and pacing approaches might be the preferred treatment options with the ability to optimize the 3 pillars of laryngeal function.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Rosenthal LHS, Benninger MS, Deeb RH. Vocal fold immobility: a longitudinal analysis of etiology over 20 years. Laryngoscope. 2007;117:1864–70.
Crumley RL. Laryngeal synkinesis: its significance to the laryngologist. The Annals of Otology, Rhinology, and Laryngology. 1989;98:87–92.
Tucker HM. Vocal cord paralysis--1979: etiology and management. Laryngoscope. 1980;90:585–90.
Hillel AD, Benninger M, Blitzer A, Crumley R, Flint P, Kashima HK, et al. Evaluation and management of bilateral vocal cord immobility. Otolaryngol Head Neck Surg. 1999;121:760–5.
Benninger MS, Hanick A, Hicks DM. Cricothyroid muscle botulinum toxin injection to improve airway for bilateral recurrent laryngeal nerve paralysis, a case series. J Voice. 2016;30:96–9.
Holinger LD, Holinger PC, Holinger PH. Etiology of bilateral abductor vocal cord paralysis: a review of 389 cases. Ann Otol Rhinol Laryngol. 1976;85:428–36.
Maisel RH, Ogura JH. Evaluation and treatment of vocal cord paralysis. Laryngoscope. 1974;84:302–16.
Benninger MS, Gillen JB, Altaian JS. Changing etiology of vocal fold immobility. Laryngoscope. 1998;108:1346–50.
Grundfast KM, Harley E. Vocal cord paralysis. Otolaryngol Clin N Am. 1989;22:569–97.
Willis WH, Weaver DF. Syringomyelia with bilateral vocal cord paralysis. Report of a case Arch Otolaryngol. 1968;87:468–70.
Zager EL, Ojemann RG, Poletti CE. Acute presentations of syringomyelia. Report of three cases. J Neurosurg. 1990;72:133–8.
Cavanagh F. Vocal palsies in children. J Laryngol Otol. 1955;69:399–418.
Gentile RD, Miller RH, Woodson GE. Vocal cord paralysis in children 1 year of age and younger. Ann Otol Rhinol Laryngol. 1986;95:622–5.
Stuart WD. The otolaryngologic aspects of myasthenia gravis. Laryngoscope. 1965;75:112–21.
Fairley JW, Hughes M. Acute stridor due to bilateral vocal fold paralysis as a presenting sign of myasthenia gravis. J Laryngol Otol. 1992;106:737–8.
Cohen SR, Geller KA, Birns JW, Thompson JW. Laryngeal paralysis in children: a long-term retrospective study. Ann Otol Rhinol Laryngol. 1982;91:417–24.
Pfenninger J. Bilateral vocal cord paralysis after severe blunt head injury--a cause of failed extubation. Crit Care Med. 1987;15:701–2.
Aiuto LA, Pavlakis SG, Boxer RA. Life-threatening organophosphate-induced delayed polyneuropathy in a child after accidental chlorpyrifos ingestion. J Pediatr. 1993;122:658–60.
Moralee SJ, Reilly PG. Metabolic stridor: bilateral vocal cord abductor paralysis secondary to hypokalaemia? J Laryngol Otol. 1992;106:56–7.
Annino DJ Jr, MacArthur CJ, Friedman EM. Vincristine-induced recurrent laryngeal nerve paralysis. Laryngoscope. 1992;102:1260–2.
Amir I, Crow YJ, Morar P. Adult-onset familial vocal fold paralysis. Ear Nose Throat J. 2015;94:E1–3.
Hsu AK, Rosow DE, Wallerstein RJ, April MM. Familial congenital bilateral vocal fold paralysis: a novel gene translocation. Int J Pediatr Otorhinolaryngol. 2015;79:323–7.
Rosen CA, Thomas JP, Anderson D. Bilateral vocal fold paralysis caused by familial hypokalemic periodic paralysis. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 1999;120:785–6.
Raza SA, Mahendran S, Rahman N, Williams RG. Familial vocal fold paralysis. J Laryngol Otol. 2002;116:1047–9.
Hsu AK, Rosow DE, Wallerstein RJ, April MM. Familial congenital bilateral vocal fold paralysis: a novel gene translocation. Int J Pediatr Otorhinolaryngol. 2015;79:323–7.
Berkowitz RG. Congenital bilateral adductor vocal cord paralysis. The Annals of otology, rhinology, and laryngology. 2003;112:764–7.
Cannon S, Ritter FN. Vocal cord paralysis in postpoliomyelitis syndrome. Laryngoscope. 1987;97:981–3.
Dupuch V, Saroul N, Aumeran C, Pastourel R, Mom T, Gilain L. Bilateral vocal cord abductor paralysis associated with primary herpes simplex infection: a case report. Eur Ann Otorhinolaryngol Head Neck Dis. 2012;129:272–4.
Rennie CE, Pai I, Selvadurai D. Tuberculosis presenting as bilateral vocal fold palsy: case report and review of otolaryngological manifestations of tuberculosis. J Laryngol Otol. 2011;125:1079–82.
Steele NP, Myssiorek D. West Nile virus induced vocal fold paralysis. Laryngoscope. 2006;116:494–6.
Ueha R, Nito T, Goto T, Sato T, Ushiku T, Yamasoba T. Bilateral vocal cord immobility resulting from cytomegalovirus pharyngitis: a case report. J Infect Chemother. 2018;24:142–6.
Panosian MS, Quatela VC. Guillain-Barre syndrome presenting as acute bilateral vocal cord paralysis. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 1993;108:171–3.
Rutter MJ, Hart CK, Alarcon A, et al. Endoscopic anterior-posterior cricoid split for pediatric bilateral vocal fold paralysis. Laryngoscope. 2018;128:257–63 This is a retrospective multiinstitutional study that looks at 19 patients that underwent an endoscopic anterior-posterior cricoid split for BVFIM 74% were considered a surgical success by either decanulation or avoided tracheotomy.
Lee JW, Bon-Mardion N, Smith ME, Marie JP. Bilateral selective laryngeal reinnervation for bilateral vocal fold paralysis in children. JAMA Otolaryngol Head Neck Surg. 2020;146:401–7 This case series describes the outcomes of 8 pediatric patients undergoing bilatearl selective laryngeal reinnervation demonstrating succesful decannulation in all cases and improvement of voice quality in most patients post-operatively.
Sedaghat S, Tapia M, Fredes F, Rojas P. Endoscopic management of bilateral vocal fold paralysis in newborns and infants. Int J Pediatr Otorhinolaryngol. 2017;97:13–7.
Li Y, Garrett G, Zealear D. Current treatment options for bilateral vocal fold paralysis: a state-of-the-art review. Clin Exp Otorhinolaryngol. 2017;10:203–12.
Jabbour J, Martin T, Beste D, Robey T. Pediatric vocal fold immobility: natural history and the need for long-term follow-up. JAMA Otolaryngol Head Neck Surg. 2014;140:428–33.
Lesnik M, Thierry B, Blanchard M, Glynn F, Denoyelle F, Couloigner V, et al. Idiopathic bilateral vocal cord paralysis in infants: case series and literature review. Laryngoscope. 2015;125:1724–8.
Rosin DF, Handler SD, Potsic WP, Wetmore RF, Tom LW. Vocal cord paralysis in children. Laryngoscope. 1990;100:1174–9.
Bogdasarian RS, Olson NR. Posterior glottic laryngeal stenosis. Otolaryngol Head Neck Surg. 1980;88:765–72.
Giotakis AI, Pototschnig C. Prognosis of congenital idiopathic abductor laryngeal paralysis with laryngeal electromyography. Laryngoscope. 2020;130:E252–7 This retrospective study discussed the long term prognostic implication of EMG analysis for BVFIM. Where all patients that had volitional activity had late recovery.
Miyamoto RC, Parikh SR, Gellad W, Licameli GR. Bilateral congenital vocal cord paralysis: a 16-year institutional review. Otolaryngol Head Neck Surg. 2005;133:241–5.
de Gaudemar I, Roudaire M, Francois M, Narcy P. Outcome of laryngeal paralysis in neonates: a long term retrospective study of 113 cases. Int J Pediatr Otorhinolaryngol. 1996;34:101–10.
Murty GE, Shinkwin C, Gibbin KP. Bilateral vocal fold paralysis in infants: tracheostomy or not? J Laryngol Otol. 1994;108:329–31.
Zbar RI, Smith RJ. Vocal fold paralysis in infants twelve months of age and younger. Otolaryngol Head Neck Surg. 1996;114:18–21.
Daya H, Hosni A, Bejar-Solar I, Evans JNG, Bailey CM. Pediatric vocal fold paralysis: a long-term retrospective study. Arch Otolaryngol Head Neck Surg. 2000;126:21–5.
Berkowitz RG. Natural history of tracheostomy-dependent idiopathic congenital bilateral vocal fold paralysis. Otolaryngol Head Neck Surg. 2007;136:649–52.
Bluestone CD, Delerme AN, Samuelson GH. Airway obstruction due to vocal cord paralysis in infants with hydrocephalus and meningomyelocele. Ann Otol Rhinol Laryngol. 1972;81:778–83.
Hsu J, Tibbetts KM, Wu D, Nassar M, Tan M. Swallowing function in pediatric patients with bilateral vocal fold immobility. Int J Pediatr Otorhinolaryngol. 2017;93:37–41.
Hartnick CJ, Brigger MT, Willging JP, et al. Surgery for pediatric vocal cord paralysis: a retrospective review. Ann Otol Rhinol Laryngol. 2003;112:1–6.
Funk RT, Jabbour J, Robey T. Factors associated with tracheotomy and decannulation in pediatric bilateral vocal fold immobility. Int J Pediatr Otorhinolaryngol. 2015;79:895–9.
Narcy P, Contencin P, Viala P. Surgical treatment for laryngeal paralysis in infants and children. Ann Otol Rhinol Laryngol. 1990;99:124–8.
Mathur NN, Kumar S, Bothra R. Simple method of vocal cord lateralization in bilateral abductor cord paralysis in paediatric patients. Int J Pediatr Otorhinolaryngol. 2004;68:15–20.
Inglis AF Jr, Perkins JA, Manning SC, Mouzakes J. Endoscopic posterior cricoid split and rib grafting in 10 children. Laryngoscope. 2003;113:2004–9.
Windsor AM, Jacobs I. Endoscopic anterior-posterior cricoid split to avoid tracheostomy in infants with bilateral vocal fold paralysis. Int J Pediatr Otorhinolaryngol. 2020;138:110325 This retrospective study evaluates 6 patients that have BVFMI in infants. an endoscopic antero-posterior cricoid split was performed and 50% of patients were able to avoid tracheostomy.
Smith ME, Park AH, Muntz HR, Gray SD. Airway augmentation and maintenance through laryngeal chemodenervation in children with impaired vocal fold mobility. Arch Otolaryngol Head Neck Surg. 2007;133:610–2.
Cohen SR, Thompson JW. Use of botulinum toxin to lateralize true vocal cords: a biochemical method to relieve bilateral abductor vocal cord paralysis. Ann Otol Rhinol Laryngol. 1987;96:534–41.
Eskew JR, Bailey BJ. Laser arytenoidectomy for bilateral vocal cord paralysis. Otolaryngol Head Neck Surg. 1983;91:294–8.
Lagier A, Nicollas R, Sanjuan M, Benoit L, Triglia JM. Laser cordotomy for the treatment of bilateral vocal cord paralysis in infants. Int J Pediatr Otorhinolaryngol. 2009;73:9–13.
Friedman EM, de Jong AL, Sulek M. Pediatric bilateral vocal fold immobility: the role of carbon dioxide laser posterior transverse partial cordectomy. Ann Otol Rhinol Laryngol. 2001;110:723–8.
Aubry K, Leboulanger N, Harris R, Genty E, Denoyelle F, Garabedian EN. Laser arytenoidectomy in the management of bilateral vocal cord paralysis in children. Int J Pediatr Otorhinolaryngol. 2010;74:451–5.
Worley G, Bajaj Y, Cavalli L, Hartley B. Laser arytenoidectomy in children with bilateral vocal fold immobility. J Laryngol Otol. 2007;121:25–7.
Madani S, Bach A, Matievics V, Erdélyi E, Sztanó B, Szegesdi I, et al. A new solution for neonatal bilateral vocal cord paralysis: endoscopic arytenoid abduction lateropexy. Laryngoscope. 2017;127:1608–14.
Puricelli MD, Peterson J, Kanotra SP. Ultrasound-guided suture lateralization in pediatric bilateral vocal fold immobility. Laryngoscope. 2020;130:E941–4.
Sztano B, Bach A, Matievics V, et al. Endoscopic arytenoid abduction lateropexy for the treatment of neonatal bilateral vocal cord paralysis - long-term results. Int J Pediatr Otorhinolaryngol. 2019;119:147–50 This is a retrospective study that evaluates long term results of arytenoid abduction lateropexy. 3 patients after >3 years voice swallowing and airway patency were very satisfactory.
Montague GL, Bly RA, Nadaraja GS, Conrad DE, Parikh SR, Chan DK. Endoscopic percutaneous suture lateralization for neonatal bilateral vocal fold immobility. Int J Pediatr Otorhinolaryngol. 2018;108:120–4.
Gray SD, Kelly SM, Dove H. Arytenoid separation for impaired pediatric vocal fold mobility. Ann Otol Rhinol Laryngol. 1994;103:510–5.
Thakkar K, Gerber ME. Endoscopic posterior costal cartilage graft placement for acute management of pediatric bilateral vocal fold paralysis without tracheostomy. Int J Pediatr Otorhinolaryngol. 2008;72:1555–8.
Provenzano MJ, Hulstein SL, Solomon DH, Bauman NM, Manaligod JM, Kacmarynski DSF, et al. Pediatric endoscopic airway management with posterior cricoid rib grafting. Laryngoscope. 2011;121:1062–6.
Dahl JP, Purcell PL, Parikh SR, Inglis AF Jr. Endoscopic posterior cricoid split with costal cartilage graft: a fifteen-year experience. Laryngoscope. 2017;127:252–7 This is a retrospective study that evaluates endoscopic posterior cricoid split with cartilage graft placement for multiple eitiologies. They describe a 28.6% success rate in patients with BVFIM.
Bliss M, Houtz D, Smith ME. Cricoid reduction laryngoplasty for treatment of dysphonia after pediatric laryngotracheal reconstruction. Int J Pediatr Otorhinolaryngol. 2015 Jan;79(1):80–2.
Cohen SR, Thompson JW, Camilon FS Jr. Botulinum toxin for relief of bilateral abductor paralysis of the larynx: histologic study in an animal model. Ann Otol Rhinol Laryngol. 1989;98:213–6.
Smith ME, Park AH, Muntz HR, Gray SD. Airway augmentation and maintenance through laryngeal chemodenervation in children with impaired vocal fold mobility. Arch Otolaryngol Head Neck Surg. 2007;133:610–2.
Daniel SJ, Cardona I. Cricothyroid onabotulinum toxin A injection to avert tracheostomy in bilateral vocal fold paralysis. JAMA Otolaryngol Head Neck Surg. 2014;140:867–9.
Lewis S, Woo P. Botulinum toxin in management of synkinesis in patients with unilateral and bilateral vocal fold paralysis. Laryngoscope. 2018;128:447–50 This study reviews the use of botulinum toxin injection to the thyroarytenoid +/− the posterior cricoarytenoid muscles in 8 patients with BVFMI demonstrating significant improvement and avoidance of surgery in 5 patients.
Tucker HM. Human laryngeal reinnervation: long-term experience with the nerve-muscle pedicle technique. Laryngoscope. 1978;88:598–604.
Tucker HM. Long-term results of nerve-muscle pedicle reinnervation for laryngeal paralysis. Ann Otol Rhinol Laryngol. 1989;98:674–6.
Zheng H, Zhou S, Chen S, Li Z, Cuan Y. An experimental comparison of different kinds of laryngeal muscle reinnervation. Otolaryngol Head Neck Surg. 1998;119:540–7.
Marie JP, Dehesdin D, Ducastelle T, Senant J. Selective reinnervation of the abductor and adductor muscles of the canine larynx after recurrent nerve paralysis. Ann Otol Rhinol Laryngol. 1989;98:530–6.
Marie JP, Lerosey Y, Dehesdin D, Jin O, Tadíe M, Andrieu-Guitrancourt J. Experimental reinnervation of a strap muscle with a few roots of the phrenic nerve in rabbits. Ann Otol Rhinol Laryngol. 1999;108:1004–11.
Li M, Zheng H, Chen S, et al. Selective reinnervation using phrenic nerve and hypoglossal nerve for bilateral vocal fold paralysis. The Laryngoscope. 2019;129:2669–73 Study of 7 patients undergoing novel selective laryngeal reinnervation technique with all 7 patients gaining some movement, and 6 of the seven gaining moderate to maximal movment on at least one side.
Mueller AH, Hagen R, Foerster G, et al. Laryngeal pacing via an implantable stimulator for the rehabilitation of subjects suffering from bilateral vocal fold paralysis: a prospective first-in-human study. Laryngoscope. 2016;126:1810–6 This case series describes the procedure and outcomes for placement of a novel laryngeal pacemaker system in 9 adult patients demonstrating the efficacy and safety of laryngeal pacing.
Zealear DL, Billante CR, Courey MS, Netterville JL, Paniello RC, Sanders I, et al. Reanimation of the paralyzed human larynx with an implantable electrical stimulation device. Laryngoscope. 2003;113:1149–56.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on PEDIATRIC OTOLARYNGOLOGY: Pediatric Airway and Voice
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dunya, G., Orb, Q.T., Smith, M.E. et al. A Review of Treatment of Bilateral Vocal Fold Movement Impairment. Curr Otorhinolaryngol Rep 9, 7–15 (2021). https://doi.org/10.1007/s40136-020-00320-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40136-020-00320-8