Abstract
Purpose of Review
Compared with high-income countries, healthcare disparities and inequities are more evident in low, lower-middle, and upper-middle-income countries with poorer housing and nutrition conditions. At least 20% of Latin America and the Caribbean are low and lower-middle-income countries. Despite the majority of the other countries being upper-middle income, the United Nations Children’s Fund had classified all the regions as “less developed,” with limited access to health care for the most vulnerable, the children. Latin America and the Caribbean regions represent an extensive territory with communication limitations and an unstable socio-political and economic environment. After considering the vast population affected by poverty worldwide and the long-term impact of kidney disease starting in childhood, it is crucial to better understand and analyze the multifactorial limiting conditions in accessing specialized care such as pediatric nephrology in disadvantaged areas.
Recent Findings
Constraints in accessing basic healthcare in rural areas make it impossible to receive specialized pediatric nephrology care including dialysis and transplantation. Disturbingly, incidence and prevalence figures of acute kidney injury, chronic and end-stage kidney disease in some Latin American and the Caribbean countries are unknown, and these conditions still represent a death sentence for underprivileged populations. However, the monumental efforts of the dedicated healthcare providers and stakeholders that pioneered the actions in the past 50 years have shown remarkable progress in developing pediatric nephology services across the continent.
Summary
In this review, we compile some of the latest evidence about the care of children and adolescents with kidney conditions in Latin America and the Caribbean, along with the experiences from the field in the care of these patients facing adverse conditions. We also highlight recommendations to address inequities and disparities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adverse socio-political and economic conditions are a common denominator in low, lower-middle (LMIC) and upper-middle-income countries [1]. Latin America and the Caribbean (LAC) is comprised of twenty-one Spanish, Portuguese, and Francophone-speaking countries and thirteen independent Caribbean islands with a total population exceeding 665 million people. LAC is 5th in children/adolescent/young adult mortality, reporting 14.4 deaths per 1000 people ages 5–24 years, and has the lowest mortality rate decrease in the past 10 years worldwide [2]. LAC was among the world’s most vulnerable regions during the COVID-19 pandemic with the highest increase in population suffering poverty in the globe [3]. The extreme poverty rate increased from 13.1 to 13.8% between 2020 and 2021, representing an increase from 81 to 86 million people affected [4•]. Inequitable access to healthcare and nutrition shows a devastating contrast to highly resourced countries.
Chronic kidney disease (CKD) has a significant burden in regions with increased poverty, accounting for 63% of the diagnosed population worldwide [5]. The Global Burden of Disease Study described increasing CKD incidence/prevalence among adults in LAC, specifically in Nicaragua, El Salvador, Honduras, and Mexico [5]. The age-standardized CKD disability-adjusted life-years showed that younger patients had less access to healthcare and quality of care in impoverished countries [5]. Of greater concern is that CKD registries in LAC are scarce, limiting analysis and the development of strategic plans. The pediatric peritoneal dialysis network registry showed that mortality rates were higher in low and LMIC compared to the high income, explaining ~ 50% of the variability by the socio-economic disparities. [6•]
Since the 1960s, pioneers of pediatric nephrology in LAC have developed programs, despite economic and socio-political conditions placing serious limitations on access to essential needs. Specialized pediatric nephrology services are not a priority for most of the LAC governments. Difficulties accessing scientific and technological advances, essential diagnostic tools, and treatments like kidney replacement therapies and transplantation overwhelm local professionals. Other relevant factors that impact delivery/continuation of treatment and patient outcomes are culture, religious beliefs, parent’s education/literacy level, and the absence of healthcare transition/self-management programs.
While substantial progress has been made, much remains to be done. The pediatric nephrology community came together in the form of “Asociación Latinomericana de Nefrología Pediátrica” (ALANEPE [Latin American Pediatric Nephrology Association]) [7] which works to overcome shared challenges and improve networking. In the following review, we describe experiences of the pediatric nephrology field in the co-authors’ regions, highlighting the strategies that have generated favorable results in disadvantaged areas. We also propose strategies to continue advancing pediatric nephrology care toward equity, justice, and inclusion in healthcare, academics, and research in low-resourced regions.
Health Equity and Disparities in Latin America and Caribbean—the Needs and Coverage
Social determinants of health impact 30–55% of health outcomes worldwide. It is well known that health and illness follow a social gradient; therefore, the lower the socioeconomic status, the worse the overall health. However, health disparity is a particular type of health difference closely linked with economic, social, or environmental disadvantage [8]. Pursuing health equity means striving for the highest possible standard of health for all people, giving special attention to the needs of those at most significant risk of poor health based on social conditions [9]. In a vast region like LAC, multiple scenarios with different development stages of the pediatric nephrology field are faced, creating a special challenge to develop strategies that meet the needs.
A Brief Overview of the Current Situation in Some LAC Regions
Patients with end-stage kidney disease face significant inequities in access and quality of care in many LAC countries. Even more concerning is the ongoing poor availability of phosphate binders, growth hormone, dialysis, or transplantation. Differences among the healthcare systems of multiple Caribbean countries carry an immense disparity. For instance, Jamaica and Dominican Republic have a universal health insurance. However, the healthcare is free only at public institutions. Nevertheless, Dominican Republic is an upper-middle-income country with a more robust economy due to its tourism compared to other islands like Haiti, a low-income country. In fact, Dominican Republic accounts for six pediatric nephrologists and has access to neonatal continuous kidney replacement therapy machines, as does Puerto Rico. Haiti only has two pediatric nephrologists and even though this country provides free healthcare, there is a severe scarcity of diagnostic services, therapeutic procedures, drug access, prenatal ultrasound, and basic immunosuppressive drugs are seldom available. Shockingly, not all the pediatric patients can be offered dialysis treatment and pediatric kidney transplantation is just a dream for most children.
The Transplant Journey for a Pediatric Patient in Peru
Kidney transplantation planning and long-term follow-up are funded by government institutions in Peru. Close to 70% of the population obtains medical care from the Ministry of Health System, and 30.1% is in poverty [1]. There are 33 pediatric nephrologists, with a ratio of 1/320,000 per young habitant and is mostly concentrated in Lima, representing three times less specialized care availability in comparison with other countries like Canada [10]. Pediatric kidney transplantation is only available in the capital city, with only three active centers now since the COVID-19 pandemic led to the fourth one’s closure. Peru’s regulations allow both living-related or deceased donor transplants; however, it has a meager deceased-donor pool availability, 0.5–2 per million habitants, [11] affected primarily by cultural and religious beliefs, making access to transplantation more challenging.
By way of example, a child on peritoneal dialysis from a southern Peruvian state needed to travel to Lima by bus for 20 h for monthly assessments losing at least 3 days of school/parent work time. The patient was coincidentally in Lima when the team received an En-bloc allograft offer matching. The immediate postoperative course was complicated by anastomosis bleeding requiring urgent surgical reintervention, followed by delayed graft function. After 3 years the graft function was stable, but these unpredictable situations imposed a disruption of their quality of life and an economic burden.
Strategies to Improve Healthcare Coverage Specialized in Pediatric Nephrology in LAC
Assistance of Non-governmental Organizations
Foundations and non-profit organizations created and directed by the nephrologists, patients’ families, and members of the community have proved to be successful in LAC [12•]. Donations are used to support patient services, including equipment, disposable supplies, medications, diagnostic tests, transportation, personnel salaries, and the infrastructure of the clinical facilities. Some families may receive support for their living expenses. In some countries, these organizations represent the major or only source of funds to finance the healthcare needs of children with CKD. A remarkable example is the Jamaica Kidney Kids Foundation (JKKF) that has provided dialysis consumables to the University Hospital of the West Indies for children with CKD since 2013. JKKF and its partners pay for laboratory/imaging studies and kidney biopsies.
Since 1999, a 5-bed pediatric nephrology service was created at one of the tertiary hospitals in Guatemala, Hospital Roosevelt. One of the co-authors listed in this publication (RL-M) led the efforts after completing a fellowship funded by the ISN at the University of Utah (UoU), guided by professors from the same institution. The sustained collaborations between Guatemala and the UoU led to further collaborations. By 2003, a pediatric renal dietitian, a child life specialist, and a pediatric urologist also received UoU training via the ISN Sister Renal Center Program. Later on, a local organization was legally established called “Fundación para el Niño Enfermo Renal” (FUNDANIER [Foundation for Children with Kidney Disease, Guatemala City, Guatemala]), devoted to the care of children with CKD [13]. In 2006, FUNDANIER led an agreement with the Ministry of Health, facilitating universal access of Guatemalan children to kidney replacement therapy, including transplant. By 2010, FUNDANIER became the national referral center for pediatric kidney care [14] and had developed a national registry of pediatric kidney patients, publishing their results. [15]
The Sister Centers Model
An outstanding sister center model is from Nicaragua. In 2000, a collaborative project between the pediatric nephrology units of Milan, Italy, and Managua established free pediatric nephrology services in Nicaragua to hospitalized children. The supporting center in Italy has provided guidance for infrastructure, information technology, and education for healthcare professionals. Services ranging from prevention programs in rural areas to kidney replacement therapies have been developed overtime. The project is funded from a partnership between the Italian private charity “Rene e Bambino Nel Mondo” and the Italian government for international collaboration managed by the Nicaraguan Ministry of Health.
In Cali, Colombia, the Fundación Valle del Lili established a collaboration with Boston’s Children Hospital, supported by the ISN Sister Renal Center Program. The pediatric nephrology center in Cali provides services to children with kidney diseases including dialysis and transplantation. Over the course of 7 years, the program has performed educational courses, participated in research activities, and published manuscripts. Additionally, Fundación Valle del Lili established one of the most successful healthcare transition programs from pediatric to adult care in South America, supported by the University of North Carolina, Chapel Hill, Self-management, and Transition to Adulthood with Treatment (STARx) program. The STARx program has developed free access translated, back-translated and validated transition assessment tools in eight languages through networking with ten countries [16]. The Spanish translation and validation in collaboration with the Hospital Infantil de México Federico Gómez, Hospital General de Mexico Eduardo Liceaga, and the Universidad Panamericana. [17]
In 2018, FUNDANIER was granted the first IPNA Sister Center Award in Central America, supported by the pediatric nephrology program at the University of Puerto Rico. The faculty at University of Puerto Rico has provided support for educational activities, webinars, clinical consultation, and mentorship for the physicians in FUNDANIER. The educational experiences include clinical rotations at University of Puerto Rico for fellows and faculty from Guatemala. FUNDANIER has established collaboration with other non-profit organizations including Bridges of Life, supporting massive screenings, equipment, and educational activities in rural areas of Guatemala.
The Role of Local Associations and Leadership
The development of pediatric nephrology has had awe-inspiring growth from two local pediatric nephrology services that functioned in the 1960s. The first one at the Hospital Infantil de Mexico Federico Gomez, and the second one at the Ricardo Gutierrez Hospital of Buenos Aires, Argentina. Over the years, services have been developed throughout the continent, and, with greater or lesser complexity, the dissemination of pediatric nephrology has been more successful, creating the need for societies to become organized and join efforts. Some societies opt to depend on international pediatric societies, or local adult nephrology societies, while a third model develops and independent local society. The development of a local association allows greater communication to create strategies for teaching and awareness campaign. The most active local societies are in Argentina, Chile, Brazil, and Colombia. ALANEPE was created in Buenos Aires and structured into three representative regions [7, 18]. This brought notable progress improving communications among countries and in a short time, ALANEPE had representatives on the international associations allowing for further networking and collaborations.
Epidemiology of Pediatric Kidney Disease in Latin America and the Caribbean—Registry Issues
Efforts for Data Collection and Registries in Latin America and the Caribbean
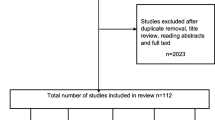
Several LAC centers participate in some global registries by IPNA, the International Pediatric Peritoneal Dialysis Registry, and the Longitudinal Monitoring Dialysis Outcomes (MONDO) registry, on its pediatric component (PICCOLO MONDO) [19]. Unfortunately, these registries have incomplete data from low-resourced countries. According to an IPNA survey and systematic literature review, only five countries in LAC reported/had evidence of a national registry (Colombia, Venezuela, Brazil, Argentina, and Uruguay) [20]. The development of local registries in the LAC has been challenging due to lack of infrastructure, expertise, and technological support to develop reliable databases. Yet, in 2004, ALANEPE established a regional registry for pediatric kidney transplants the “Registro Latinoamericano de Trasplante Pediátrico” (RELATREP) [21]. Since its initiation, and according to the last 2018 report, over ~ 4700 children receive treatment in 70 pediatric transplant centers from 18 LAC countries, representing the most successful effort to collect transplant data in LAC children [21]. Sustainability of the longitudinal follow-up and automating data handling using advanced software are some of the issues to address to perform more active epidemiological and analytical approaches using this registry.
Strategies to Develop Registries for Children and Adolescents With CKD in Low-Resourced Countries
Patient registries can provide information on clinical practice, patient outcomes, safety, and comparative effectiveness. The USA National Committee on Vital and Health Statistics describes registries as “an organized system for the collection, storage, retrieval, analysis, and dissemination of information on individual persons who have either a particular disease, a condition (i.e., a risk factor) that predisposes to the occurrence of a health-related event, or prior exposure to substances (or circumstances) known or suspected to cause adverse health effects.” The purposes of patient registries include the description disease natural history, measuring quality of care or improving patient outcomes, among others [22]. Developing reliable national registries in disadvantaged areas will provide data autonomy to determine disease burden and the strategies to mitigate it with local budgets. Strategies to build a registry must take into consideration the local, state, regional, or national legal and regulatory implications. Particular attention must be placed in protecting patient privacy. The host(s) of international registries must set up rules of culturally concordant informed consent, data entry, ownership, and reporting. [23]
International networking to create sustainable international registries that include low-resourced countries national registries should be a priority. Technology, structure, and expertise from regions in the world with ongoing registries must be shared and implemented in low-resourced countries to determine kidney disease prevalence. An example of international collaboration is the “Red de Enfermedad de Kawasaki en América Latina” (Latin American Kawasaki Disease Network), a partnership between the University of California San Diego and The Sociedad Latin-American de Infectología Pediátrica, having autonomy and ownership of the registry in LAC [24]. Another remarkable example of an international registry with active inclusion of low-resourced countries is the “SWEET Registry” that includes data in children and adolescents with any type of diabetes from around the world and utilizes a software already translated into eight different languages. [25]
Fellowship and Mentorship Programs in Disadvantaged Areas
Healthcare distribution inequalities are due to the restricted pediatric nephrology specialized professionals available in the different regions and many challenging scenarios. Most healthcare systems in LAC have centralized specialized care and extensive rural regions have little access to these services. Local and trained professionals who return to their regions face limited resources and cannot practice what they have learned. Frequently, the limited vacancies in the urban centers increase the risk of professional emigration “brain drain.” Nevertheless, building local capacities that better understand the relevance and needs of the region is still the most suitable strategy for coverage [26]. The development of fellowship programs in some LAC has been achieved through local and international resources. Twelve of the 34 LAC countries had reported having a pediatric nephrology training program. The largest pediatric nephrology fellowship programs are in Mexico, Argentina, Chile, and Brazil. IPNA, ALANEPE, and the ISN have sponsored many educational activities held in LAC, creating kidney disease awareness in children and resulting in collaboration between different countries. Efforts continue to cross borders to train young doctors and nurses in the field. [27]
Addressing Workforce and Training Needs—the Role of an Academic Strategy and Mentorship
Taking advantage of all available resources seems to be the key to success. As many programs have little or no support from their local government, it becomes critical to identify resources from non-governmental organizations. Through their fellowship programs, ISN and IPNA have played a key role in LAC providing support for training pediatric nephrologists. These programs provide support for living expenses for 6–12 months to complete fellowships. Since the beginning of the IPNA Fellowship Program, thirty-three physicians from LAC have trained in specialized centers and returned to their hometown. For instance, the JKKF, IPNA, and ISN fellowship programs have provided support to train three pediatric nephrologists expanding the workforce. Furthermore, Jamaica has completed three teaching courses for pediatricians across the island in the diagnosis and management of CKD a collaboration between IPNA and Jamaica Kidney Kids Foundation (JKKF). To date, six centers in five different countries (Guatemala, Colombia, Brazil, Chile, and Argentina) are certified as regional training centers by the IPNA Fellowship Program.
In LAC, mentorship is scarce due to the lack of resources, overwhelming clinical work, and fewer academic centers than in developed regions. ISN, IPNA, and Saving Young Lives (SYL) have developed different international mentorship programs engaging healthcare providers from low-resourced countries. Undoubtedly, mentors’ guidance optimizes efforts and actions toward the mentees’ career goals [28•]. Mentorship can be delivered in multiple ways. Formal mentorship is the guidance relationship between the mentor and mentee through an academic institution/association’s program, where both parties develop a specific plan. However, informal mentorship is usually based on trust, shared interests, and mutual reciprocity. In a sponsorship relationship, the senior faculty brings networking career opportunities and actively invites the trainee/junior faculty to participate in their academic circle. Awareness of all the possible mentorship relationships is crucial to improve the development of pediatric nephrology professionals and patient care in disadvantaged regions.
A successful mentor–mentee relationship that evolved to an international collaboration with a public health impact was the developed between RL-M (co-author of this publication) from Guatemala and Dr. Richard Siegler from Utah University. Doctor Siegler committed and engaged with his mentee on the long-term up for the development of a local sustainable pediatric nephrology division with dialysis and transplantation. Furthermore, the academic mentorship resulted in a pediatric nephrology training center with the aid of the Universidad San Carlos de Guatemala and the ISN Ambassador program. In 2021, FUNDANIER was selected one of the Regional Trainings Centers in Pediatric Nephrology and related disciplines with the goal of becoming a supporting center for other emerging centers in Central America.
Challenges to academic growth in professionals practicing in disadvantaged areas are also associated with language barriers and limited access to the most updated evidence in the field. Most LAC countries have poor or no access to indexed scientific journals through their universities, limiting academic competencies and research capabilities. Strategies for equitable educational opportunities worldwide need to be optimized. A call to action for publishing houses to develop access to their publications is warranted. Early efforts, including translating high-impact publications to languages other than English, have been suggested to facilitate knowledge dissemination and improve clinical practice in all regions of the world. [29]
Ethical Implications of Practicing Pediatric Nephrology in Disadvantaged Regions
In disadvantaged regions, healthcare workers face different challenges in providing care to patients. For instance, in Haiti, despite limited available specialized nephrology care, they are hampered by insufficient and unpredictable resources, placing them at moral distress having to choose which patient is going benefit more with a kidney replacement therapy. Physicians must make heartbreaking choices between life and death when it comes to acute kidney injury and/or end-stage kidney disease, imposing a utilitarian approach. On the other hand, those who receive kidney replacement therapy still face substantial challenges due to the lack of laboratory and dialysis supplies/equipment, or specialized drugs. Because of this, parents often decide to go to traditional medicine or turn to religious beliefs, worsening the prognosis and increasing mortality. In the most disadvantaged regions in LAC, there is no local ethical board dedicated to guide the challenging clinical practice with complex ethical dilemmas. The providers lacking an ethics board for clinical practice are exposed to great distress and moral injury.
Creating local ethical committees to guide and support the physicians and ancillary team members facing these demanding situations may be one of the steps to decrease this psychological and emotional burden. However, local efforts are focused on solving essential primary needs such as medical supplies. An international support network handled virtually can be developed to assist physician’s practice and wellness. Advocacy is also necessary to support the patients and their families in such situations.
Research Programs, Communication, and Networking
Research Programs Dedicated to Pediatric Nephrology in LAC
Medical research in under-resourced settings is a big challenge as the limited resources are dedicated to clinical needs. In most LAC countries, research is not a big government priority. Nonetheless, LAC researchers have produced remarkable research over time, overcoming multiple constraints and developing local research laboratories in the most prominent academic centers. Unfortunately, they are very few, considering the LAC pediatric population. International collaborations have allowed an increase in research productivity by developing studies in areas without local research programs. However, building local capacities is crucial for autonomy and continuity. Increased local research will generate data for greater government awareness and access to national funding. Supporting local research in under-resourced settings is key to characterizing the most vulnerable populations affected with kidney disease, accounting for specific risk factors and social determinants of health. Equity in healthcare access is having an active initiative in medical research that includes patients from disadvantaged regions. Inclusivity of a more diverse population will secure equity in access to the latest scientific and technological advances for all patients and their families.
Communication Strategies to Improve Knowledge Dissemination and Networking
Latin American Archives of Pediatric Nephrology—a Regional Journal
In 2000, a co-author of this publication and ALANEPE’s co-founder (RE) proposed creating an official journal representing the association and the first “Archivos Latinoamericanos de Nefrología Pediátrica” issue was published a year later. The publication included works by pioneers Drs. Carlos Gianantonio, Gustavo Gordillo, Bernardo Rodriguez Iturbe, and Juan Rodriguez Soriano. Initially, only review articles were authorized by IPNA; however, thanks to Dr. Vera Koch’s advocacy, a former ALANEPE president, in 2015 IPNA allowed original research to be published as well. To date, more than sixty issues have been published uninterruptedly in 21 years, with minimal economic resources, thanks to RE tireless efforts. This regional journal has allowed dissemination of local research, improved communication between countries, and supporting academic growth.
Social Media, the New Way to Communicate Academics and Science
The devastating COVID-19 pandemic demonstrated the feasibility of virtual resources to communicate. Social media platforms have been instrumental in the growth of the ALANEPE community, facilitating communications within countries and internationally, knowledge dissemination, and access to academic materials. The most popular social media platforms like Twitter, Inc.®, Instagram, Inc.®, and Facebook, Inc.® are free and easy to access from mobile devices, becoming the preferred media to connect professionally within the medical and scientific field. Social media provides an excellent advantage for under-resourced settings since it allows access to academic activities and networking. After creating the “ALANEPE Redes” group in 2019 (@Alanepe1), handled by trainees and junior faculty volunteers, ALANEPE had at least doubled the number of members, ran a virtual conference, and provided numerous academic spaces to interact/connect with worldwide experts. The communication in social media has raised awareness of the LAC challenges in practicing pediatric nephrology. It has also instrumented networking within and beyond the pediatric nephrology field. Creating and actively managing an official account with enthusiastic and motivated volunteers is critical to facilitating exchanges. Additionally, social media data generation and analytics provide valuable information about academic interactions to inform practice and possible interventions, as shown by Madariaga et al., on their recent publication on gender equity. [30•]
In conclusion, social media platforms are an accessible and affordable communication tool for under-resourced regions to connect professionally worldwide and endorse academic growth.
Conclusions
Over time, Latin America and the Caribbean have shown tremendous progress in developing pediatric nephrology programs. However, much work remains to be done in several countries to address ongoing health inequities and disparities. Different strategies have worked to successfully provide nephrology care to children, adolescents, and young adults and committed local organizations/associations facilitating services and agreements are key to achieve progress. Long-term communication, networking, and compassionate partnerships with more developed countries are crucial to build and sustain pediatric nephrology services in Latin America and the Caribbean. Mentorship and academic activities are essential to keep providers updated and increase workforce capacity. Access to information about the latest technological, scientific, and research advances is part of providing pediatric nephrology care with equity in the most disadvantaged areas. Initiatives engaging local healthcare professionals to answer their clinical research questions should be a global priority. Funding the creation of national registries in unprivileged regions investing in advanced software that facilitate data linkage to international and global registries should be considered by international societies. The development of regional clinical research is part of data generation with an equity lens, allowing the inclusion of underrepresented groups in international studies, accounting for socioeconomic determinants of health and local risk factors. Easy-to-use communication tools such as social media platforms (e.g., @IPNA_PedNeph, @ASPNeph, @CAPNeph, @ESPNSciety, @EspnYpnn, @ASianPNA, @AfricanAFRAN, @ISNkidneycare, @SLANH_, @ASNkidney, @GlomCon, @NephJC), have proven to be fast-spreading tools for knowledge dissemination and networking. Engaging professionals from the most unprivileged areas around the globe to communicate/share responsibly through social media channels will facilitate the creation of new partnership agreements (Table 1).
As inhabitants of the world, the care of children, adolescents, and young adults with kidney disease in disadvantaged regions is a world-shared responsibility. The authors of this review call for increasing networking, collaborations, and continuous international partnership to mitigate the health inequities and disparities in Latin America, the Caribbean, and other regions of the globe (Fig. 1).
Proposed strategic model to address disparities and inequalities in pediatric nephrology care in Latin America and the Caribbean. The figure shows a linked cycle to address the need for more equitable pediatric nephrology care in Latin America and the Caribbean. Each cycle element is closely related to the other to have a continuous and sustainable energy. The outer circle demonstrates the crucial intervention of international initiatives to feed the cycle and keep it working. The dynamic correlation between local and international elements should be revised constantly to update according to needs and progression. LAC, Latin America and the Caribbean
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
The World Bank - IBRD-IDA. Understanding poverty. online. Published 2022. https://www.worldbank.org/en/understanding-poverty
UNICEF, Data. Mortality among children, adolescents and youth aged 5–24. Monitoring the situation of children and women. Published 2021. https://data.unicef.org/topic/child-survival/child-and-youth-mortality-age-5-24/
Lakner C, Mahler DG, Negre M, Prydz EB. How much does reducing inequality matter for global poverty? J Econ Inequal. 2022;20(3):559–85. https://doi.org/10.1007/s10888-021-09510-w.
• Arenas de Mesa A, Trucco D, Atuesta B, et al. Social panorama of Latin America. (Barcena A, Cimoli M, Garcia-Buchaca R, et al., eds.). United Nations publication; 2022.https://repositorio.cepal.org/bitstream/handle/11362/47719/1/S2100654_en.pdfThis online publication is a detailed, thorough description and analysis of the socio-economical situation in Latin America and the Caribbean, showing the impact of the COVID-19 pandemic and the disparities to address in healthcare access.
Xie Y, Bowe B, Mokdad AH, et al. Analysis of the Global Burden of Disease study highlights the global, regional, and national trends of chronic kidney disease epidemiology from 1990 to 2016. Kidney Int. 2018;94(3):567–81. https://doi.org/10.1016/j.kint.2018.04.011.
• Ploos van Amstel S, Noordzij M, Borzych-Duzalka D, et al. Mortality in children treated with maintenance peritoneal dialysis: findings from the International Pediatric Peritoneal Dialysis Network Registry. Am J Kidney Dis. 2021;78(3):380–390. https://doi.org/10.1053/j.ajkd.2020.11.031. This is a large multicenter cohort study of the outcomes in the pediatric population receiving peritoneal dialysis. The authors included different regions of the world, including Latin America, and demonstrated a high impact on mortality when in low-income countries.
Asociacion Latinoamericana de Nefrologia Pediatrica. Quienes Somos? Historia, December 2020. ALANEPE.org website. https://www.alanepe.org/quienes-somos/historia/#. Accessed 7 Jan 2023.
Schillinger D. The intersections between social determinants of health, health literacy, and health disparities. Stud Health Technol Inform. 2020;269:22–41. https://doi.org/10.3233/SHTI200020.
Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep. 2014;129(SUPPL. 2):19–31. https://doi.org/10.1177/00333549141291s206.
Satlin LM, Andreoli SP, Schnaper HW. Pediatric nephrology around the world – North America. In: Avner E, Harmon W, Niaudet P, Yoshikawa N, editors. Pediatric Nephrology. Springer, Berlin, Heidelberg; 2009. https://doi.org/10.1007/978-3-540-76341-3_81.
DIGOT. Informe Gestión de la Dirección General de Donaciones Trasplantes y Banco de Sangre (DIGDOT). Ministerio de Salud Perú. Published 2022. https://www.gob.pe/21088-ministerio-de-salud-direccion-general-de-donaciones-trasplantes-y-banco-de-sangre-digdot
• Banerjee S, Kamath N, Antwi S, Bonilla-Felix M. Paediatric nephrology in under-resourced areas. Pediatr Nephrol. 2022;37(5):959–72. https://doi.org/10.1007/s00467-021-05059-y. In this publication, the authors explored advances in improving pediatric nephrology care in under-resourced areas using a literature search, questionnaires to the leading international association’s members and personal communications.
Lou-Meda R. ESRD in Guatemala and a model for preventive strategies: outlook of the Guatemalan foundation for children with kidney diseases. Ren Fail. 2006;28(8):689–91. https://doi.org/10.1080/08860220600938258.
Lou-Meda R. Comprehensive approach to pediatric kidney diseases in Guatemala: Foundation for Children with Kidney Diseases (FUNDANIER). Clin Nephrol. 2015;83:82–4. https://doi.org/10.5414/CNP83S082.
Cerón A, Fort MP, Morine CM, Lou-Meda R. Chronic kidney disease among children in Guatemala. Rev Panam Salud Publica/Pan Am J Public Heal. 2014;36(6):376–82.
Ferris MED-G de. UNC STARx Program. University of North Carolina, Chapel Hill. https://www.med.unc.edu/transition
Cantú-Quintanilla G, Ferris M, Otero A, et al. Validation of the UNC TRxANSITION ScaleTMVersion 3 among mexican adolescents with chronic kidney disease. J Pediatr Nurs Nurs Care Child Fam. 2016;30(5):e71–81. https://doi.org/10.1016/j.pedn.2015.06.011.
Koch V, Orta N, Exeni R. ALANEPE. In: Avner E, Harmon W, Niaudet P, Yoshikawa N, Emma F, Goldstein S, editors. Pediatric Nephrology. Springer, Berlin, Heidelberg; 2016. https://doi.org/10.1007/978-3-662-43596-0_70.
Hussein R, Alvarez-Elías AC, Topping A, et al. A cross-sectional study of growth and metabolic bone disease in a pediatric global cohort undergoing chronic hemodialysis. J Pediatr. 2018;202:171-178.e3. https://doi.org/10.1016/j.jpeds.2018.07.033.
van Ploos AS, Noordzij M, Warady BA, et al. Renal replacement therapy for children throughout the world: the need for a global registry. Pediatr Nephrol. 2018;33(5):863–71. https://doi.org/10.1007/s00467-017-3863-5.
Asociación Latinoamericana de Nefrología Pediátrica (ALANEPE). Sociedad de Trasplantes de Latinoamérica y Caribe (STALYC). Registro Latinoamericano de Trasplante Renal Pediátrico (RELATREP). Reporte 2018. Arch larinoamericanos Nefrol pediátrica. 2020;20(1):34–48.
The National Committee on Vital Health Statistics. Office of the Assistant Secretary for Planning and Evaluation. Published 2022. https://ncvhs.hhs.gov/?_ga=2.121158797.409626640.1669007751-183531000.1669007750
Rockville. Patient registries. In: Gliklich R, Dreyer N, Leavy M, eds. Registries for evaluating patient outcomes: a user’s guide. 3rd ed. Agency for Healthcare Research and Quality (US); 2014. https://www.ncbi.nlm.nih.gov/books/NBK208643/
Moreno E, Garcia SD, Bainto E, et al. Presentation and outcomes of Kawasaki disease in Latin American infants younger than 6 months of age: a multinational multicenter study of the REKAMLATINA Network. Front Pediatr. 2020;8(July):2–8. https://doi.org/10.3389/fped.2020.00384.
Cardona-Hernandez R, Schwandt A, Alkandari H, et al. Glycemic outcome associated with insulin pump and glucose sensor use in children and adolescents with type 1 diabetes Data from the international pediatric registry SWEET. Diabetes Care. 2021;44(5):1176–84. https://doi.org/10.2337/dc20-1674.
Harris DCH, Dupuis S, Couser WG, Feehally J. Training nephrologists from developing countries: does it have a positive impact? Kidney Int Suppl. 2012;2(3):275–8. https://doi.org/10.1038/kisup.2012.32.
Braveman P. What are health disparities and health equity? We need to be clear. Public Health Rep. 2014;129(SUPPL. 2):5–8. https://doi.org/10.1177/00333549141291s203.
• Vasylyeva TL, Díaz-González de Ferris ME, Hains DS, et al. Developing a research mentorship program: the American Society of Pediatric Nephrology’s experience. Front Pediatr. 2019;7(APR):1–8. https://doi.org/10.3389/fped.2019.00155. In this article, the authors described the development of a research mentorship program at the American Society of Pediatric Nephrology. They also shared results from mentor-mentee relationships built through their matching strategy.
Pakenham-Walsh N. Improving the availability of health research in languages other than English. Lancet Glob Heal. 2018;6(12):e1282. https://doi.org/10.1016/S2214-109X(18)30384-X.
• Madariaga HM, Sieberg CB, Vela X, Kwon K, Lerma EV, Desai T. Gender interactions on Twitter and medical education: how is nephrology doing? Nephrol Dial Transplant. 2022;37(5):923–7. https://doi.org/10.1093/ndt/gfab058. In this publication, the authors evidenced, using social media data, gender disparities in nephrology academia, demonstrating the usefulness of social media tools for communications and assessing equity.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Author Maria Ferris has received consultant honoraria from George Clinical CRO and ProKidney; all the other authors have non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Alvarez-Elías, A.C., Lou-Meda, R., Exeni, R. et al. Addressing Health Inequities and Disparities in Children With Kidney Disease in Disadvantaged Areas: the Latin American and Caribbean Experience. Curr Pediatr Rep 11, 40–49 (2023). https://doi.org/10.1007/s40124-023-00287-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40124-023-00287-2