Abstract
Purpose of Review
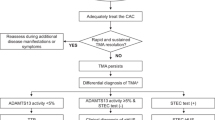
This review aims to examine the current definitions of primary and secondary hemolytic uremic syndromes. Specifically, it seeks to determine which external conditions can result in secondary Thrombotic microangiopathy (TMA), which can trigger cases of primary atypical uremic syndromes (aHUS), and the role of complement in the pathogenesis of TMA spectrum disorders.
Recent Findings
Building on the growing insight about the pathogenic role of dysregulation of the alternative complement pathway in primary aHUS, the successful use of complement-blocking treatment in cases of thrombotic microangiopathy with coexisting conditions (secondary TMA), along with the identification of complement mutations in some of these cases, indicates a so far possibly under-appreciated pathogenic role for complement in diagnoses within the TMA spectrum.
Summary
Uncontrolled complement activity and pro-thrombotic environments represent a unifying pathogenic mechanism in aHUS and the TMA spectrum disorders and point towards shared diagnostic and therapeutic pathways.

Similar content being viewed by others
Abbreviations
- ADAMTS13:
-
A disintegrin and metalloproteinase with a thrombospondin type 1 motif member 13
- AP:
-
Alternative pathway (complement system)
- aHUS:
-
Atypical hemolytic uremic syndrome
- CMV:
-
Cytomegaloviruses
- CP:
-
Classical pathway (complement system)
- DEAP-HUS:
-
Deficiency of CFHR plasma proteins and autoantibody-positive form of _______hemolytic uremic syndrome
- DGKE:
-
Diacylglycerol kinase epsilon
- ESRD:
-
End-stage renal disease
- FB:
-
Factor B
- FH:
-
Factor H
- FHR:
-
Factor H–related protein
- FI:
-
Factor I
- HELLP:
-
Hemolysis, elevated liver enzymes, and low platelet count
- HSCT:
-
Hematopoietic stem cell transplantation
- HUS:
-
Hemolytic uremic syndrome
- INF2:
-
Inverted formin-2
- LP:
-
Lectin pathway (complement system)
- MAC:
-
Membrane attack complex
- MAHA:
-
Microangiopathic hemolytic anemia
- MBL:
-
Mannose-binding lectin
- MCP:
-
Membrane cofactor protein (CD46)
- SCR:
-
Short consensus repeat
- STEC-HUS/eHUS:
-
Shiga toxin–producing E. coli mediated HUS
- Stx:
-
Shiga toxin
- THBD:
-
Thrombomodulin (CD141)
- TMA:
-
Thrombotic microangiopathy
- TTP:
-
Thrombotic thrombocytopenic purpura
References
George JN, Nester CM. Syndromes of thrombotic microangiopathy. N Engl J Med. 2014;371(7):654–66.
Noris M, Remuzzi G. Hemolytic uremic syndrome. J Am Soc Nephrol. 2005;16(4):1035–50.
Kavanagh D, Goodship TH, Richards A. Atypical hemolytic uremic syndrome. Semin Nephrol. 2013;33(6):508–30.
Mayer CL, Leibowitz CS, Kurosawa S, Stearns-Kurosawa DJ. Shiga toxins and the pathophysiology of hemolytic uremic syndrome in humans and animals. Toxins. 2012;4(11):1261–87.
Walport MJ. Complement. First of two parts. N Engl J Med. 2001;344(14):1058–66.
Keating GM. Eculizumab: a review of its use in atypical haemolytic uraemic syndrome. Drugs. 2013;73(18):2053–66.
Schaefer F, Ardissino G, Ariceta G, Fakhouri F, Scully M, Isbel N, et al. Clinical and genetic predictors of atypical hemolytic uremic syndrome phenotype and outcome. Kidney Int. 2018;94(2):408–18.
Noris M, Caprioli J, Bresin E, Mossali C, Pianetti G, Gamba S, et al. Relative role of genetic complement abnormalities in sporadic and familial aHUS and their impact on clinical phenotype. Clinical journal of the American Society of Nephrology : CJASN. 2010;5(10):1844–59.
Brocklebank V, Wood KM, Kavanagh D. Thrombotic microangiopathy and the kidney. Clin J Am Soc Nephrol. 2018;13(2):300–17.
Legendre CM, Licht C, Muus P, Greenbaum LA, Babu S, Bedrosian C, et al. Terminal complement inhibitor eculizumab in atypical hemolytic-uremic syndrome. N Engl J Med. 2013;368(23):2169–81.
Riedl M, Fakhouri F, Le Quintrec M, Noone DG, Jungraithmayr TC, Fremeaux-Bacchi V, et al. Spectrum of complement-mediated thrombotic microangiopathies: pathogenetic insights identifying novel treatment approaches. Semin Thromb Hemost. 2014;40(4):444–64.
Sarma JV, Ward PA. The complement system. Cell Tissue Res. 2011;343(1):227–35.
Kavanagh D, Goodship T. Genetics and complement in atypical HUS. Pediatr Nephrol. 2010;25(12):2431–42.
Ferreira VP, Pangburn MK, Cortes C. Complement control protein factor H: the good, the bad, and the inadequate. Mol Immunol. 2010;47(13):2187–97.
Stahl AL, Vaziri-Sani F, Heinen S, Kristoffersson AC, Gydell KH, Raafat R, et al. Factor H dysfunction in patients with atypical hemolytic uremic syndrome contributes to complement deposition on platelets and their activation. Blood. 2008;111(11):5307–15.
Noris M, Remuzzi G. Atypical hemolytic-uremic syndrome. N Engl J Med. 2009;361(17):1676–87.
Atkinson JP, Goodship THJ. Complement factor H and the hemolytic uremic syndrome. J Exp Med. 2007;204:1245–8.
Maga TK, Nishimura CJ, Weaver AE, Frees KL, Smith RJ. Mutations in alternative pathway complement proteins in American patients with atypical hemolytic uremic syndrome. Hum Mutat. 2010;31(6):E1445–60.
Richards A, Kathryn Liszewski M, Kavanagh D, Fang CJ, Moulton E, Fremeaux-Bacchi V, et al. Implications of the initial mutations in membrane cofactor protein (MCP; CD46) leading to atypical hemolytic uremic syndrome. Mol Immunol. 2007;44(1–3):111–22.
Schramm EC, Roumenina LT, Rybkine T, Chauvet S, Vieira-Martins P, Hue C, et al. Mapping interactions between complement C3 and regulators using mutations in atypical hemolytic uremic syndrome. Blood. 2015;125(15):2359–69.
Kavanagh D, Pappworth IY, Anderson H, Hayes CM, Moore I, Hunze EM, et al. Factor I autoantibodies in patients with atypical hemolytic uremic syndrome: disease-associated or an epiphenomenon? Clin J Am Soc Nephrol. 2012;7(3):417–26.
Noone D, Waters A, Pluthero FG, Geary DF, Kirschfink M, Zipfel PF, et al. Successful treatment of DEAP-HUS with eculizumab. Pediatr Nephrol. 2014;29(5):841–51.
Weiler H, Isermann BH. Thrombomodulin. J Thromb Haemost. 2003;1(7):1515–24.
Delvaeye M, DeVriese A, Moons M, Esmon N, Esmon C, Conway EM. Regulation of complement activation by thrombomodulin. Blood: American Society of Hematology; 2009. p. 5127.
Bu F, Maga T, Meyer NC, Wang K, Thomas CP, Nester CM, et al. Comprehensive genetic analysis of complement and coagulation genes in atypical hemolytic uremic syndrome. J Am Soc Nephrol. 2014;25(1):55–64.
Lemaire M, Fremeaux-Bacchi V, Schaefer F, Choi M, Tang WH, Le Quintrec M, et al. Recessive mutations in DGKE cause atypical hemolytic-uremic syndrome. Nat Genet. 2013;45(5):531–6.
Hofer J, Janecke AR, Zimmerhackl LB, Riedl M, Rosales A, Giner T, et al. Complement factor H-related protein 1 deficiency and factor H antibodies in pediatric patients with atypical hemolytic uremic syndrome. Clin J Am Soc Nephrol. 2013;8(3):407–15.
Hofer J, Giner T, Jozsi M. Complement factor H-antibody-associated hemolytic uremic syndrome: pathogenesis, clinical presentation, and treatment. Semin Thromb Hemost. 2014;40(4):431–43.
Zipfel PF, Mache C, Muller D, Licht C, Wigger M, Skerka C. DEAP-HUS: deficiency of CFHR plasma proteins and autoantibody-positive form of hemolytic uremic syndrome. Pediatr Nephrol. 2010;25(10):2009–19.
Marinozzi MC, Vergoz L, Rybkine T, Ngo S, Bettoni S, Pashov A, et al. Complement factor B mutations in atypical hemolytic uremic syndrome—disease-relevant or benign? J Am Soc Nephrol. 2014;25(9):2053–65.
Sinha A, Gulati A, Saini S, Blanc C, Gupta A, Gurjar BS, et al. Prompt plasma exchanges and immunosuppressive treatment improves the outcomes of anti-factor H autoantibody-associated hemolytic uremic syndrome in children. Kidney Int. 2014;85(5):1151–60.
Azukaitis K, Simkova E, Majid MA, Galiano M, Benz K, Amann K, et al. The phenotypic spectrum of nephropathies associated with mutations in diacylglycerol kinase epsilon. J Am Soc Nephrol. 2017;28(10):3066–75.
Challis RC, Ring T, Xu Y, Wong EKS, Flossmann O, Roberts ISD, et al. Thrombotic microangiopathy in inverted formin 2–mediated renal disease. J Am Soc Nephrol. 2017;28:1084–91.
Loirat C, Fakhouri F, Ariceta G, Besbas N, Bitzan M, Bjerre A, et al. An international consensus approach to the management of atypical hemolytic uremic syndrome in children. Pediatr Nephrol. 2016;31(1):15–39.
Spinale JM, Ruebner RL, Kaplan BS, Copelovitch L. Update on Streptococcus pneumoniae associated hemolytic uremic syndrome. Curr Opin Pediatr. 2013;25(2):203–8.
Watanabe T. Renal complications of seasonal and pandemic influenza A virus infections. Eur J Pediatr. 2013;172(1):15–22.
Freist M, Garrouste C, Szlavik N, Coppo P, Lautrette A, Heng AE. Efficacy of eculizumab in an adult patient with HIV-associated hemolytic uremic syndrome: a case report. Medicine. 2017;96(51):e9358.
Saab KR, Elhadad S, Copertino D, Laurence J. Thrombotic microangiopathy in the setting of HIV infection: a case report and review of the differential diagnosis and therapy. AIDS Patient Care STDs. 2016;30(8):359–64.
Jin A, Boroujerdi-Rad L, Shah G, Chen JL. Thrombotic microangiopathy and human immunodeficiency virus in the era of eculizumab. Clin Kidney J. 2016;9(4):576–9.
van Hoeve K, Vandermeulen C, Van Ranst M, Levtchenko E, van den Heuvel L, Mekahli D. Occurrence of atypical HUS associated with influenza B. Eur J Pediatr. 2017;176(4):449–54.
Mittal N, Hartemayer R, Jandeska S, Giordano L. Steroid responsive atypical hemolytic uremic syndrome triggered by influenza B infection. J Pediatr Hematol Oncol. 2018.
Kobbe R, Schild R, Christner M, Oh J, Loos S, Kemper MJ. Case report - atypical hemolytic uremic syndrome triggered by influenza B. BMC Nephrol. 2017;18(1):96.
Brocklebank V, Wong EKS, Fielding R, Goodship THJ, Kavanagh D. Atypical haemolytic uraemic syndrome associated with a CD46 mutation triggered by Shigella flexneri. Clin Kidney J. 2014;7(3):286–8.
Miklaszewska M, Zachwieja K, Drozdz D, Pallinger E, Takacs B, Szilagyi A, et al. Hemolytic uremic syndrome with mycoplasma pneumoniae infection and membrane cofactor protein mutation - case report. Przegl Lek. 2016;73(11):862–4.
Omura T, Watanabe E, Otsuka Y, Yoshida Y, Kato H, Nangaku M, et al. Complete remission of thrombotic microangiopathy after treatment with eculizumab in a patient with non-Shiga toxin-associated bacterial enteritis: a case report. Medicine. 2016;95(27):e4104.
Lee MD, Tzen CY, Lin CC, Huang FY, Liu HC, Tsai JD. Hemolytic uremic syndrome caused by enteroviral infection. Pediatr Neonatol. 2013;54(3):207–10.
Java A, Edwards A, Rossi A, Pandey R, Gaut J, Delos Santos R, et al. Cytomegalovirus-induced thrombotic microangiopathy after renal transplant successfully treated with eculizumab: case report and review of the literature. Transpl Int. 2015;28(9):1121–5.
Fraga-Rodriguez GM, Brio-Sanagustin S, Turon-Vinas E, Dixon BP, Carreras-Gonzalez E. Eculizumab in a child with atypical haemolytic uraemic syndrome and haemophagocytic lymphohistiocytosis triggered by cytomegalovirus infection. BMJ Case Rep. 2017.
Mathur P, Hollowoa B, Lala N, Thanendrarajan S, Matin A, Kothari A, et al. Enterococcus raffinosus infection with atypical hemolytic uremic syndrome in a multiple myeloma patient after autologous stem cell transplant. Hematol Rep. 2017;9(3):7094.
Inglis JM, Barbara JA, Juneja R, Milton C, Passaris G, Li JYZ. Atypical haemolytic uraemic syndrome associated with Clostridium difficile infection successfully treated with eculizumab. Case Rep Nephrol. 2018;2018:1759138.
Condom P, Mansuy JM, Decramer S, Izopet J, Mengelle C. Atypical hemolytic uremic syndrome triggered by varicella infection. IDCases. 2017;9:89–90.
Buyon JP. Systemic lupus erythematosus. In: Klipper J, Stone J, Crofford L, White P, editors. Primer on the rheumatic diseases. Springer: Springer; 2008. p. 303–38.
de Holanda MI, Porto LC, Wagner T, Christiani LF, Palma LMP. Use of eculizumab in a systemic lupus erythemathosus patient presenting thrombotic microangiopathy and heterozygous deletion in CFHR1-CFHR3. A case report and systematic review. Clin Rheumatol. 2017;36(12):2859–67.
Bermea RS, Sharma N, Cohen K, Liarski VM. Use of eculizumab in atypical hemolytic uremic syndrome, complicating systemic lupus erythematosus. Journal of clinical rheumatology : practical reports on rheumatic & musculoskeletal diseases. 2016;22(6):320–3.
El-Husseini A, Hannan S, Awad A, Jennings S, Cornea V, Sawaya BP. Thrombotic microangiopathy in systemic lupus erythematosus: efficacy of eculizumab. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2015;65(1):127–30.
Raufi AG, Scott S, Darwish O, Harley K, Kahlon K, Desai S, et al. Atypical hemolytic uremic syndrome secondary to lupus nephritis. Responsive to Eculizumab Hematology reports. 2016;8(3):6625.
Attar RZ, Ramel EI, Safdar OY, Desoky S. A case of patient with renal lupus with an initial presentation of hemolytic uremic syndrome triggered by streptococcal infection. Clinical case reports. 2018;6(4):712–8.
Ono M, Ohashi N, Namikawa A, Katahashi N, Ishigaki S, Tsuji N, et al. A rare case of lupus nephritis presenting as thrombotic microangiopathy with diffuse pseudotubulization possibly caused by atypical hemolytic uremic syndrome. Intern Med. 2018;57(11):1617–23.
Coppo R, Peruzzi L, Amore A, Martino S, Vergano L, Lastauka I, et al. Dramatic effects of eculizumab in a child with diffuse proliferative lupus nephritis resistant to conventional therapy. Pediatr Nephrol. 2015;30(1):167–72.
Weitz IC. Thrombotic microangiopathy in cancer. Thromb Res. 2018;164(Suppl 1):S103–s5.
Sussman TA, Abazeed M, McCrae K, Khorana AA. RNA sequencing approached to identify novel biomarkers for venous thromboembolism (VTE) in lung cancer. Blood: Am Soc Hematol; 2017. p. 554.
Krisinger MJ, Goebeler V, Lu Z, Meixner SC, Myles T, Pryzdial EL, et al. Thrombin generates previously unidentified C5 products that support the terminal complement activation pathway. Blood. 2012;120(8):1717–25.
Krishnappa V, Gupta M, Shah H, Das A, Tanphaichitr N, Novak R, et al. The use of eculizumab in gemcitabine induced thrombotic microangiopathy. BMC Nephrol. 2018;19(1):9.
Eremina V, Jefferson JA, Kowalewska J, Hochster H, Haas M, Weisstuch J, et al. VEGF inhibition and renal thrombotic microangiopathy. N Engl J Med. 2008;358(11):1129–36.
Blake-Haskins JA, Lechleider RJ, Kreitman RJ. Thrombotic microangiopathy with targeted cancer agents. Clin Cancer Res. 2011;17(18):5858–66.
Allison SJ. VEGF–complement interactions.
Quinn CT. Minireview: clinical severity in sickle cell disease: the challenges of definition and prognostication. Exp Biol Med (Maywood). 2016;241(7):679–88.
Chudwin DS, Korenblit AD, Kingzette M, Artrip S, Rao S. Increased activation of the alternative complement pathway in sickle cell disease. Clin Immunol Immunopathol. 1985;37(1):93–7.
Gavriilaki E, Mainou M, Christodoulou I, Koravou EE, Paleta A, Touloumenidou T, et al. In vitro evidence of complement activation in patients with sickle cell disease. Haematologica. 2017;102:e481–e2.
Johnston RB Jr. Increased susceptibility to infection in sickle cell disease: review of its occurrence and possible causes. South Med J. 1974;67(11):1342–8.
Mold C, Tamerius JD, Phillips G Jr. Complement activation during painful crisis in sickle cell anemia. Clin Immunol Immunopathol. 1995;76(3 Pt 1):314–20.
Barrett-Connor E. Bacterial infection and sickle cell anemia. An analysis of 250 infections in 166 patients and a review of the literature. Medicine. 1971;50(2):97–112.
Frimat M, Tabarin F, Dimitrov JD, Poitou C, Halbwachs-Mecarelli L, Fremeaux-Bacchi V, et al. Complement activation by heme as a secondary hit for atypical hemolytic uremic syndrome. Blood. 2013;122(2):282–92.
Chonat S, Chandrakasan S, Kalinyak KA, Ingala D, Gruppo R, Kalfa TA. Atypical haemolytic uraemic syndrome in a patient with sickle cell disease, successfully treated with eculizumab. Br J Haematol. 2016;175(4):744–7.
Chen M, Zhuang J, Yang J, Wang D, Yang Q. Atypical hemolytic uremic syndrome induced by CblC subtype of methylmalonic academia: a case report and literature review. Medicine. 2017;96(43):e8284.
Adrovic A, Canpolat N, Caliskan S, Sever L, Kiykim E, Agbas A, et al. Cobalamin C defect-hemolytic uremic syndrome caused by new mutation in MMACHC. Pediatr Int. 2016;58(8):763–5.
Barlas UK, Kihtir HS, Goknar N, Ersoy M, Akcay N, Sevketoglu E. Hemolytic uremic syndrome with dual caution in an infant: cobalamin C defect and complement dysregulation successfully treated with eculizumab. Pediatr Nephrol. 2018;33(6):1093–6.
Ardissino G, Perrone M, Tel F, Testa S, Morrone A, Possenti I, et al. Late onset cobalamin disorder and hemolytic uremic syndrome: a rare cause of nephrotic syndrome. Case Rep Pediatr. 2017;2017:2794060.
Navarro D, Azevedo A, Sequeira S, Ferreira AC, Carvalho F, Fidalgo T, et al. Atypical adult-onset methylmalonic acidemia and homocystinuria presenting as hemolytic uremic syndrome. CEN Case Rep. 2018;7(1):73–6.
Zhu Z, Chen H, Gill R, Wang J, Spitalewitz S, Gotlieb V. Diabetic ketoacidosis presenting with atypical hemolytic uremic syndrome associated with a variant of complement factor B in an adult: a case report. J Med Case Rep. 2016;10:38.
Williams CR, Gooch JL. Calcineurin inhibitors and immunosuppression - a tale of two isoforms. Expert Rev Mol Med. 2012;14:e14.
Trimarchi HM, Truong LD, Brennan S, Gonzalez JM, Suki WN. FK506-associated thrombotic microangiopathy: report of two cases and review of the literature. Transplantation. 1999;67(4):539–44.
Merola J, Yoo PS, Schaub J, Smith JD, Rodriguez-Davalos MI, Tichy E, et al. Belatacept and eculizumab for treatment of calcineurin inhibitor-induced thrombotic microangiopathy after kidney transplantation: case report. Transplant Proc. 2016;48(9):3106–8.
Renner B, Klawitter J, Goldberg R, McCullough JW, Ferreira VP, Cooper JE, et al. Cyclosporine induces endothelial cell release of complement-activating microparticles. J Am Soc Nephrol. 2013;24(11):1849–62.
Ikeda T, Okumi M, Unagami K, Kanzawa T, Sawada A, Kawanishi K, et al. Two cases of kidney transplantation-associated thrombotic microangiopathy successfully treated with eculizumab. Nephrology (Carlton). 2016;21(Suppl 1):35–40.
Shochet L, Kanellis J, Simpson I, Ta J, Mulley W. De novo thrombotic microangiopathy following simultaneous pancreas and kidney transplantation managed with eculizumab. Nephrology (Carlton). 2017;22(Suppl 1):23–7.
Gray JM, Ameduri RK. Tacrolimus-associated hemolytic uremic syndrome in a pediatric heart transplant recipient. Pediatr Transplant. 2016;20(6):866–7.
Vardas PN, Hashmi ZA, Hadi MA. Identification and management of atypical hemolytic uremic syndrome immediately post-heart transplantation. J Card Surg. 2015;30(4):373–5.
Le Quintrec M, Lionet A, Kamar N, Karras A, Barbier S, Buchler M, et al. Complement mutation-associated de novo thrombotic microangiopathy following kidney transplantation. Am J Transplant. 2008;8(8):1694–701.
Garg N, Rennke HG, Pavlakis M, Zandi-Nejad K. De novo thrombotic microangiopathy after kidney transplantation. Transplant Rev (Orlando). 2018;32(1):58–68.
Jodele S, Licht C, Goebel J, Dixon BP, Zhang K, Sivakumaran TA, et al. Abnormalities in the alternative pathway of complement in children with hematopoietic stem cell transplant-associated thrombotic microangiopathy. Blood. 2013;122(12):2003–7.
Jodele S, Fukuda T, Vinks A, Mizuno K, Laskin BL, Goebel J, et al. Eculizumab therapy in children with severe hematopoietic stem cell transplantation–associated thrombotic microangiopathy. Biol Blood Marrow Transplant. 2014;20(4):518–25.
Jodele S, Zhang K, Zou F, Laskin B, Dandoy CE, Myers KC, et al. The genetic fingerprint of susceptibility for transplant-associated thrombotic microangiopathy. Blood. 2016;127(8):989–96.
Hasegawa D, Saito A, Nino N, Uemura S, Takafuji S, Yokoi T, et al. Successful treatment of transplantation-associated atypical hemolytic uremic syndrome with eculizumab. J Pediatr Hematol Oncol. 2018;40(1):e41–e4.
Dashe JS, Ramin SM, Cunningham FG. The long-term consequences of thrombotic microangiopathy (thrombotic thrombocytopenic purpura and hemolytic uremic syndrome) in pregnancy. Obstet Gynecol. 1998;91(5 Pt 1):662–8.
Bruel A, Kavanagh D, Noris M, Delmas Y, Wong EKS, Bresin E, et al. Hemolytic uremic syndrome in pregnancy and postpartum. Clin J Am Soc Nephrol. 2017;12(8):1237–47.
Saad AF, Roman J, Wyble A, Pacheco LD. Pregnancy-associated atypical hemolytic-uremic syndrome. AJP Rep. 2016;6(1):e125–8.
Fakhouri F, Roumenina L, Provot F, Sallee M, Caillard S, Couzi L, et al. Pregnancy-associated hemolytic uremic syndrome revisited in the era of complement gene mutations. J Am Soc Nephrol. 2010;21(5):859–67.
Huerta A, Arjona E, Portoles J, Lopez-Sanchez P, Rabasco C, Espinosa M, et al. A retrospective study of pregnancy-associated atypical hemolytic uremic syndrome. Kidney Int. 2018;93(2):450–9.
Chua J, Paizis K, He SZ, Mount P. Suspected atypical haemolytic uraemic syndrome in two post-partum patients with foetal-death in utero responding to eculizumab. Nephrology (Carlton). 2017;22(Suppl 1):18–22.
Gately R, San A, Kurtkoti J, Parnham A. Life-threatening pregnancy-associated atypical haemolytic uraemic syndrome and its response to eculizumab. Nephrology (Carlton). 2017;22(Suppl 1):32–5.
Baghli S, Abendroth C, Farooq U, Schaub JA. Atypical presentation of pregnancy-related hemolytic uremic syndrome. Am J Kidney Dis. 2018;72:451–6.
Saad AF, Roman J, Wyble A, Pacheco LD.
Andries G, Karass M, Yandrapalli S, Linder K, Liu D, Nelson J, et al. Atypical hemolytic uremic syndrome in first trimester pregnancy successfully treated with eculizumab. Exp Hematol Oncol. 2017;6:4.
Timmermans S, Abdul-Hamid MA, Vanderlocht J, Damoiseaux J, Reutelingsperger CP, van Paassen P. Patients with hypertension-associated thrombotic microangiopathy may present with complement abnormalities. Kidney Int. 2017;91(6):1420–5.
Nzerue C, Oluwole K, Adejorin D, Paueksakon P, Fremont R, Akatue R, et al. Malignant hypertension with thrombotic microangiopathy and persistent acute kidney injury (AKI). Clin Kidney J. 2014;7(6):586–9.
Zhang B, Xing C, Yu X, Sun B, Zhao X, Qian J. Renal thrombotic microangiopathies induced by severe hypertension. Hypertens Res. 2008;31(3):479–83.
Thind G, Kailasam K. Malignant hypertension as a rare cause of thrombotic microangiopathy. BMJ Case Rep. 2017.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Renal
Rights and permissions
About this article
Cite this article
Jacobs, E., Ortiz, C. & Licht, C. The Role of Complement in the Pathogenesis of HUS and the TMA Spectrum Disorders. Curr Pediatr Rep 7, 1–11 (2019). https://doi.org/10.1007/s40124-019-00186-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40124-019-00186-5