Abstract
Introduction
To evaluate the expected impact of the Algeria national immunization program (NIP) and potential impact for a Tunisia NIP, this study assessed the public health and economic value of vaccination, through a cost-effectiveness analysis, for a PCV13 or PCV10 NIP, compared with no vaccination.
Methods
A decision-analytic model was programmed in Microsoft Excel™ and adapted to evaluate the clinical and economic outcomes of PCV vaccination. Assuming a steady state, the model estimated invasive pneumococcal disease (IPD; bacteremia and meningitis), all-cause pneumonia (inpatient and outpatient), and all-cause otitis media cases as well as the associated costs from a payer perspective. The base case scenario assumed direct effects for both PCVs and indirect effects (against IPD) for PCV13 only.
Results
In Algeria, compared with no vaccination program, PCV13 would save 2177 lives and avoid nearly 349,000 cases of IPD, pneumonia, and AOM at a highly cost-effective value of $308 per QALY. In Tunisia, PCV13 would save 308 lives and avoid 1305 cases of IPD, 4833 cases of pneumonia, and 54,957 cases of AOM at a highly cost-effective value of $848 per QALY. PCV10 prevented 1224 deaths and 270,483 cases of disease in Algeria and prevented 172 deaths and 56,610 cases in Tunisia. PCV10 was cost-effective in both Algeria at $731/QALY and in Tunisia at $1366/QALY.
Conclusion
The ongoing NIP in Algeria is projected to reduce the impact and economic toll of pneumococcal disease in Algeria. If an NIP were also introduced in Tunisia, a commensurate impact would be expected. PCV NIPs are highly cost-effective, highly impactful public health interventions.
Funding
Pfizer.
Similar content being viewed by others
Introduction
Streptococcus pneumoniae (S. pneumoniae) is a common gram-positive bacterium with more than 95 serotypes, often colonizing the nasopharynx of healthy infants. S. pneumoniae can spread across the mucosa to cause non-invasive diseases, and occasionally the bacteria cross the mucosal barrier to cause invasive disease. Non-invasive disease is represented mainly by pneumonia (lung infection) and otitis media (OM, middle ear infection). Invasive pneumococcal disease (IPD) occurs if the bacteria enter the bloodstream (bacteremia/septicemia) or travel via the bloodstream to seed other sterile sites (meningitis, septic arthritis, and osteomyelitis). Both invasive and non-invasive pneumococcal diseases present a substantial health and economic burden worldwide.
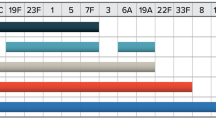
A seven-valent pneumococcal polysaccharide-protein conjugate vaccine (Prevenar®, PCV7) was licensed in February 2000 in the USA and subsequently recommended for routine immunization of all infants beginning at 2 months of age, with additional recommendations provided for the immunization of older infants and children at an increased risk of pneumococcal disease [1]. PCV7 offered protection against the seven serotypes responsible for a high proportion of disease worldwide (4, 6B, 9 V, 14, 18C, 19F, and 23F). Four years after PCV7 implementation in the USA, surveillance results indicated a 20% decrease in all-cause OM visit rates [2], a 52.4% decrease in all-cause pneumonia hospitalizations [3], and a 39% decrease in cases of all-cause pneumonia [4] in children < 2 years. Subsequently, the next generation of PCVs, the 10- (PCV10) and 13-valent (PCV13) vaccines, was introduced (Supplementary Table 1) and offered greater serotype coverage against disease caused by an additional three (1, 5, and 7F) and six (1, 3, 5, 6A, 7F, and 19A) serotypes, respectively, that were not covered in PCV7 [5, 6]. Now, 7 years since their introductions, real-word effectiveness studies indicate further effects for PCV10 [7, 8] and PCV13 [9,10,11,12] on invasive and non-invasive disease, in proportion to the enhanced serotype coverage beyond PCV7.
Numerous countries around the world have adopted PCVs into a national immunization program (NIP) in response to the substantial prevalence of pneumococcal diseases [13, 14], morbidity, and mortality [15]. Vaccine serotypes of S. pneumoniae have been identified as the predominant cause of IPD [16] in North Africa, causing 76.9% [18], 86.8% [16], and up to 90% [17] in Algeria and 68% [19], 78% [20], and up to 78.7% [21] in Tunisia. Some countries now have adopted PCV NIPs [13, 14], beginning with PCV13 in Morocco in October 2010 followed by PCV10 in July 2012 [22, 23] and then PCV13 in Algeria in April 2016. Likewise, PCV10 and PCV13 are registered and available within the private markets of Morocco and Tunisia. The introduction and maintenance of childhood pneumococcal vaccination programs in Morocco and Algeria, and the introduction in Tunisia, are expected to result in reduced mortality, disease burden, and direct medical costs.
Cost-effectiveness analyses are an effective tool to inform decision-makers about the value of introducing a vaccination program and the clinical and economic impact of each available PCV program [24]. Lower-middle income countries often perceive the cost of PCVs as high relative to other vaccines, but evidence suggests that PCV immunization programs can be a cost-saving and/or highly cost-effective health intervention to reduce their substantial disease burden [25, 26]. The objective of this study was to assess the public health impact and value of vaccination as assessed by the cost-effectiveness of a PCV13 or PCV10 NIP compared with no vaccination. These outcomes are presented for Algeria as the expected impact of the ongoing NIP and in Tunisia as the potential impact should an NIP begin.
Methods
Model
A decision-analytic model was programmed in Microsoft Excel™ and adapted to evaluate the clinical and economic outcomes of PCV vaccination in Tunisia and Algeria based on the total cases of IPD, pneumonia, and acute otitis media avoided, as described in detail previously [27,28,29,30]. Individuals entered the model with either a PCV13 or PCV10 NIP in place. Children < 1 year were assumed to receive the full two-dose primary series and one booster dose in the 2nd year of life. Each individual vaccine recipient had a probability of the following mutually exclusive health states: no disease, pneumococcal meningitis, pneumococcal bacteremia, all-cause pneumonia (in- or outpatient), and all-cause OM (Supplementary Fig. 1). IPD (bacteremia and meningitis) and inpatient pneumonia conferred an increased risk of mortality (Table 1), while meningitis also carried a probability of long-term sequelae such as neurologic impairment and hearing loss. Outpatient pneumonia and otitis media were expected not to be associated with mortality.
Outcomes due to vaccinating an infant birth cohort were calculated for the entire population over a 1-year time horizon once the vaccine effects were assumed to reach a steady state. The model then estimates the number of cases: IPD (bacteremia and meningitis), all-cause pneumonia (inpatient and outpatient), and all-cause OM. The estimated number of cases was calculated under multiple scenarios, which also included the assumption of indirect protection, meaning that the effects of the vaccine extended to both vaccinated and unvaccinated groups. Costs and quality adjusted life years (QALYs) were discounted at an assumed rate of 3% for both Algeria and Tunisia, and the results are presented from a payer perspective.
Population and Vaccination Rates
Table 1 presents population estimates for Algeria and Tunisia in 2016 with age-specific estimates in Supplementary Tables 2 and 3 [31]. Vaccination coverage for a three-dose series of PCV in an NIP was assumed to be 95% for Algeria and 98% for Tunisia, based on DTP3 (third-dose Diphtheria Tetanus Pertussis) coverage reported to the WHO for the year 2016 [32].
Incidence, Case Fatality Rates, and Serotype Coverage
Age-specific life expectancy was assumed to be the same as the general population for all individuals in the model. Incidence and case fatality rates for IPD were applied from country-specific estimates in children < 5 years of age [33] and from global estimates from lower-middle income countries of individuals ≥ 5 years of age [25]. Incidence and case-fatality rates of all-cause pneumonia were based on country-specific estimates published by Rudan et al. in children < 5 years of age [13, 14] and based on global estimates for individuals ≥ 5 years of age [25]. Hospitalized pneumonia was assumed to represent 8.6% of total cases of all-cause pneumonia in both Algeria and Tunisia. All pneumonia rates were adjusted to reflect age groups specific to the model. Due to the lack of local data, rates of all-cause OM were based on a large surveillance study conducted in the USA [34]. The only disease sequelae considered were in association with pneumococcal meningitis at an assumed rate of 7% for neurologic impairment and 13% for hearing loss [35].
Serotype coverage was obtained from local serotyping studies in Algeria [16] and Tunisia [20] by calculating the proportion of serotypes in the population covered by PCV10 and PCV13 and applied to all disease states (IPD, pneumonia, OM) and across all ages (Table 1).
Direct Effect
The direct effect of vaccine coverage corresponded to the reduction in disease among vaccinated individuals. To estimate direct effects for PCV10 or PCV13, vaccine efficacy estimates from PCV7 clinical trial data were adjusted based on country-specific serotype coverage, proportional to the additional serotypes covered in either PCV10 or PCV13, since no head-to-head efficacy trial exists, and clinical efficacy and impact data may not be directly comparable because of individual studies' differences in implementation, dosing, and underlying pneumococal etiology. Direct effects of PCV10 and PCV13 against IPD, pneumonia, and AOM were assumed. Direct effects against invasive pneumococcal disease (IPD) were taken to be 94% for the seven serotypes in common, based on clinical trial data for PCV7 [36]. Direct effects of PCV7 against pneumonia, in- and outpatient, were derived from the impact against clinical (all-cause) pneumonia [35, 36] and then adjusted to country- and vaccine-specific serotype coverage. Estimates of efficacy against all-cause AOM were also similarly derived from PCV7 trial data [37]. Effectiveness against pneumonia and AOM has been confirmed in real-world settings for PCV13, suggesting that current assumptions are conservative and may underestimate the true impact [38, 39].
Indirect Effect
Indirect effects represent the reduction in disease observed among unvaccinated individuals based on a mechanism of decreased acquistion of vaccine serotypes among vaccinated individuals that limits their circulation within the population. Since the introduction of PCV7 18 years ago and then of PCV13 8 years ago, numerous studies have demonstrated robust indirect effects of PCV7 and PCV13 [36, 38, 40]. Due to the robust data on indirect protection based on results from the US Centers for Disease Control and Prevention’s Active Bacterial Core Surveillance (ABCs) [35], we made a simplifying assumption that indirect effects of PCV7 would be similar in both Algeria and Tunisia, assuming a steady state of vaccine effects. To account for the difference in serotype distribution across countries, the indirect effects observed for PCV7 were adjusted to reflect local serotype coverage proportional to each vaccine [2, 41, 42] (Supplementary Table 4). In the base case scenario, PCV13 was assumed to confer an indirect effect on IPD, and PCV10 was not assumed to confer indirect effects, consistent with the available effectiveness data on indirect effects for both PCV10 [7, 8] and PCV13 [43]. In scenario analyses, indirect effects for pneumonia were included.
Economic Inputs
Due to a lack of local data reflecting direct medical costs, separate meetings in Algeria (3 June 2013) and Tunisia (21 June 2013) gathered local experts (in total, 25 pediatricians, microbiologists, and epidemiologists) to provide estimates in the local currency [Algeria (DZD) and Tunisia (TND)]. Costs were inflated to reflect 2016 values based on estimates from the World Bank [44] and for consistency were converted to USD based on exchange rates of 109.4 DZD:USD and 2.15 TND:USD as of April 2017.
Direct medical costs are those considered to treat cases of disease directly and for the costs for vaccine administration. Hospitalization costs for pneumococcal meningitis, pneumococcal sepsis/bacteremia, and pneumonia were based on hospital stay durations of 15, 6, and 5 days, respectively. Outpatient pneumonia costs included a physician consultation, chest X-ray, antibiotic(s), anti-inflammatory agent(s), and laboratory test(s) (Table 1). Otitis media costs included a physician consultation, antibiotic(s), and an anti-inflammatory agent (acetaminophen). Three doses per vaccinated child (2 + 1 schedule) and vaccination uptake of 95% and 98% of the birth cohort for Algeria and Tunisia, respectively, were assumed. Vaccination consisted of an administration fee per dose of USD 0.92 in Algeria and USD 2.48 in Tunisia and assumed vaccine prices per dose for PCV10 and PCV13 in both Algeria and Tunisia of USD 15.70. Additional scenario analyses were tested assuming a price per dose of either 14.13 or 12.56 for PCV10 in both Algeria and Tunisia.
In this analysis, a utility of 1.0 represented perfect health while 0.0 represented death. In the current analysis, utility weights were applied to life-years to estimate QALYs for individuals experiencing sequelae due to pneumococcal disease. Utility weights for meningitis sequelae of 0.60 for neurologic impairment and 0.80 for hearing loss (Table 1) [45] were applied for the remainder of the life expectancy.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Model Calculations
Calculated costs and outcomes for a vaccination strategy with PCV10 or PCV13 included the number of disease cases and deaths avoided, of QALYs gained, and of total costs from a payer perspective. Costs and outcomes for each PCV, versus no vaccination, were estimated. In accordance with the WHO-CHOICE [24], PCVs were considered to be cost-effective if they averted 1 quality adjusted life-year for < 3 times per capita gross domestic product (GDP) and to be highly cost-effective at < 1 time the GDP. The base case scenario assumed direct effects for each PCV against IPD, AOM, and pneumonia but indirect effects against IPD for PCV13 only.
Scenario Analysis
Additional scenario analyses were undertaken where both PCVs provide indirect protection for IPD and pneumonia, or solely with direct protection. In addition, scenario analyses varying mortality and utility rates by 20% and removing discounting (0%) were conducted.
Results
Tables 2 and 3 depict the health outcomes and costs of implementing a universal PCV vaccination program in Algeria and Tunisia under the base case scenario and under the varying sensitivity scenarios.
In Algeria, compared with no vaccination, implementing a PCV13 vaccination program would avoid 7608 cases of IPD, 57,800 cases of pneumonia, and 283,588 cases of AOM and save 2177 lives from pneumococcal diseases per year (Table 2). Each year, PCV13 is expected to offset $25.7 M of medical costs in Algeria and $2.24 M in Tunisia, respectively. Under the assumption of a 2 + 1 vaccination schedule, PCV13 would be highly cost effective at (USD) an incremental cost-effectiveness ratio (ICER) of $308 per QALY (< 1 × per capita GDP) from the payer perspective. Running a similar analysis for PCV10 versus no vaccination, 1224 deaths and 270,483 total cases of IPD, pneumonia, and acute otitis media would be avoided, and PCV10 would be highly cost-effective at $731/QALY (< 1 × per capita GDP) from the payer perspective. Each year, PCV10 is expected to offset $17.6 M of medical costs in Algeria and $1.8 M in Tunisia, respectively In scenarios assuming a price of 14.13 and 12.56 for PCV10, the cost per QALY was $616/QALY and $500/QALY, respectively.
In Tunisia, a PCV13 vaccination program would reduce the impact of pneumococcal disease by 1305 cases of IPD, 4833 cases of pneumonia, and 54,957 cases of AOM, and PCV13 would save 308 lives compared with the absence of a program at a highly cost-effective ICER of $848/QALY (< 1 × per capita GDP) (Table 2). In Tunisia, a PCV10 program would prevent 172 deaths and over 56,610 total cases of IPD, pneumonia, and acute otitis media, and it would be highly cost-effective at $1366/QALY (< 1 × per capita GDP). In scenarios assuming prices for PCV10 of 14.13 or 12.56, the cost per QALY was $1405/QALY and $1205/QALY, respectively.
Table 3 indicates the cost-effectiveness of PCV10 and PCV13 under varying assumptions for the impact of indirect effects. A PCV13 vaccination program remained highly cost-effective, even under the most restrictive assumption that there were no indirect effects, in Algeria at $475 per QALY (< 1 × per capita GDP) and Tunisia at $1239/QALY (< 1 × per capita GDP). For PCV10, the cost under the assumption that PCV10 conferred no indirect protection was $731/QALY in Algeria and $1366/QALY in Tunisia compared with no vaccination. By assuming that there was indirect protection for IPD and pneumonia, the cost per QALY decreased from the base case scenario to $198/QALY in Algeria and to $650/QALY in Tunisia. PCV13 versus no vaccination is expected to be more cost-effective compared with PCV10 versus no vaccination in all scenarios. All results remained cost-effective (< 1 × GDP per capita GDP) after varying mortality and utility rates and under a 0% discount rate.
Discussion
We used a well-established decision-analytic model to assess the cost-effectiveness in Algeria and Tunisia of a PCV13 pediatric immunization program compared with no vaccination and ran a similar analysis for PCV10. Compared with no vaccination, both PCV10 and PCV13 are cost-effective strategies in both Algeria and Tunisia. PCV13 prevents 348,997 total cases of disease in Algeria and 61,095 in Tunisia, and PCV10 prevents 270,483 and 56,610 total cases, respectively. A PCV13 program is expected to generate $25.79 M and $2.24 M in direct medical cost-savings in Algeria and Tunisia, respectively, offsetting a significant portion of the cost of vaccination. PCV10 can generate $17.6 M and $1.8 M in direct medical savings in Algeria and Tunisia, respectively.
Pharmacoeconomic analyses provide decision-makers with a holistic assessment of cost and benefits of vaccination programs and can be used as a tool to inform for future NIPs. This decision-analytic model has been applied in many settings [27,28,29,30] and provides a robust estimate of cost-effectiveness for the current situations in both Algeria and in Tunisia under varying scenarios that represent potential uncertainties. Epidemiologic inputs used in the model were informed by country-level estimates from the literature.
Our findings are supported by economic evidence of the continued cost-effectiveness of pneumococcal vaccination with PCV13 around the world. For instance, a cost-effectiveness study in Tunisia reported PCV13 to be a highly cost-effective strategy compared with no vaccination [26]. In addition, a study on the cost-effectiveness of PCVs across 35 pooled lower-middle-income countries, inclusive of both Tunisia and Algeria, reported both PCV10 and PCV13 as cost-effective compared with no vaccine, though a PCV13 program would reduce the most disease and associated costs [25]. In Spain, PCV13 implemented as a 2 + 1 schedule was found to be a cost-effective intervention from the payer perspective, compared with no vaccination [46]. Similar results were reported for Portugal when comparing PCV13 to no vaccination [47]. Our results suggest both PCV10 and PCV13 are cost-effective. Due to the broader serotype coverage of PCV13, numerous European countries have implemented a PCV13 program to prevent the most morbidity and mortality due to S. pneumoniae [27, 28, 30, 48]. In part due to the cost-effectiveness of PCVs, Algeria implemented a PCV13 NIP in April 2016, and our findings suggest Tunisia would benefit from a similar program.
Several limitations must be acknowledged in interpreting these results. First, due to a lack of publicly available cost data, all direct costs were derived from local experts, utilizing a conservative view, potentially biasing our results to underestimate the value of an NIP [26]. Yet, because costs were equally applied to both PCV10 and PCV13 vaccination, the bias would likely be non-differential between the two vaccines. Second, the model extrapolated the indirect protection that has been observed for PCV7 to PCV13 (as a base case). Numerous real-world studies have demonstrated a reduction in IPD among adults after implementing a national PCV13 infant immunization program, supporting the relevant impact of indirect effects [9, 49,50,51]. In a scenario analysis, indirect protection was assumed for PCV10. Nonetheless, even in a no indirect protection scenario analysis, each vaccine remained cost-effective in both Algeria and Tunisia. In the absence of country-specific epidemiologic data, global or regional disease estimates are an accepted method to inform gaps. However, future studies should aim to address these limitations by obtaining country-specific estimates for all disease states, as opposed to applying global or regional data, which may under- or overestimate the true disease incidence. In addition, the validity of these findings may be confirmed in future studies by assessing the impact of the implemented PCV program in Algeria.
Conclusion
A national program of pneumococcal vaccination can have a tremendous public health impact by preventing pneumococcal disease morbidity and mortality in Algeria and Tunisia. PCV13 has the highest coverage of local disease-causing pneumococcal serotypes and can offer significant prevention of disease through indirect protection, resulting in a highly cost-effective prevention program. This can lead to substantial health benefits and cost savings in North African societies.
References
Advisory Committee on Immunization Practices, Preventing pneumococcal disease among infants and young children. Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2000;49(RR-9):1–35.
Grijalva CG, et al. National impact of universal childhood immunization with pneumococcal conjugate vaccine on outpatient medical care visits in the United States. Pediatrics. 2006;118(3):865–73.
Zhou F, et al. Health care utilization for pneumonia in young children after routine pneumococcal conjugate vaccine use in the United States. Arch Pediatr Adolesc Med. 2007;161(12):1162–8.
Grijalva CG, et al. Decline in pneumonia admissions after routine childhood immunisation with pneumococcal conjugate vaccine in the USA: a time-series analysis. Lancet. 2007;369(9568):1179–86.
Prymula R, et al. Pneumococcal capsular polysaccharides conjugated to protein D for prevention of acute otitis media caused by both Streptococcus pneumoniae and non-typable Haemophilus influenzae: a randomised double-blind efficacy study. Lancet. 2006;367(9512):740–8.
Hausdorff WP, Feikin DR, Klugman KP. Epidemiological differences among pneumococcal serotypes. Lancet Infect Dis. 2005;5(2):83–93.
National Institute for Health and Welfare Incidence of invasive pneumococcal disease in Finland. 2016 23 June 2016. https://www.thl.fi/en/web/thlfi-en/research-and-expertwork/projects-and-programmes/monitoring-the-population-effectiveness-of-pneumococcal-conjugate-vaccination-in-the-finnish-national-vaccination-programme/incidence-of-invasive-pneumococcal-disease-in-finland. Accessed 1 Oct 2017.
New Zealand Public Health Surveillance: Institute of Environmental Science and Research Ltd (ESR). Data synthesized from Invasive pneumococcal disease reports 2004–2015. 2016 [cited 2016 30 September]. https://surv.esr.cri.nz/surveillance/IPD.php. Accessed 1 Oct 2017.
Moore MR, et al. Effect of use of 13-valent pneumococcal conjugate vaccine in children on invasive pneumococcal disease in children and adults in the USA: analysis of multisite, population-based surveillance. Lancet Infect Dis. 2015;15(3):301–9.
Lepoutre A, et al. Impact of the pneumococcal conjugate vaccines on invasive pneumococcal disease in France, 2001–2012. Vaccine. 2015;33(2):359–66.
Steens A, et al. Prompt effect of replacing the 7-valent pneumococcal conjugate vaccine with the 13-valent vaccine on the epidemiology of invasive pneumococcal disease in Norway. Vaccine. 2013;31(52):6232–8.
Ben-Shimol S, et al. Early impact of sequential introduction of 7-valent and 13-valent pneumococcal conjugate vaccine on IPD in Israeli children < 5 years: an active prospective nationwide surveillance. Vaccine. 2014;32(27):3452–9.
Rudan I, et al. Global estimate of the incidence of clinical pneumonia among children under five years of age. Bull World Health Organ. 2004;82(12):895–903.
Rudan I, et al. Epidemiology and etiology of childhood pneumonia. Bull World Health Organ. 2008;86(5):408–16.
Liu L, et al. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet. 2012;379(9832):2151–61.
Ramdani-Bouguessa N, et al. Evolution of antimicrobial resistance and serotype distribution of Streptococcus pneumoniae isolated from children with invasive and noninvasive pneumococcal diseases in Algeria from 2005 to 2012. New Microb New Infect. 2015;6:42–8.
Ziane H, et al. Serotypes and antibiotic susceptibility of Streptococcus pneumoniae isolates from invasive pneumococcal disease and asymptomatic carriage in a pre-vaccination period, in Algeria. Front Microbiol. 2016;7:803.
Tali-Maamar H, et al. Serotyping and antibiotic susceptibility of Streptococcus pneumoniae strains isolated in Algeria from 2001 to 2010. Med Mal Infect. 2012;42(2):59–65.
Marzouk M, et al. Serotype distribution and antimicrobial resistance of invasive and noninvasive pneumococcal isolates in Tunisia. Microb Drug Resist. 2015;21(1):85–9.
Charfi F, Smaoui H, Kechrid A. Non-susceptibility trends and serotype coverage by conjugate pneumococcal vaccines in a Tunisian paediatric population: a 10-year study. Vaccine. 2012;30(Suppl 6):G18–24.
Ktari S, et al. Serotype distribution and antibiotic susceptibility of Streptococcus pneumoniae strains in the south of Tunisia: a five-year study (2012–2016) of pediatric and adult populations. Int J Infect Dis. 2017;65:110–5.
Elmdaghri N, et al. Changing epidemiology of pediatric Streptococcus pneumoniae isolates before vaccine introduction in Casablanca (Morocco). Vaccine. 2012;30(Suppl 6):G46–50.
Diawara I, et al. Invasive pneumococcal disease among children younger than 5 years of age before and after introduction of pneumococcal conjugate vaccine in Casablanca, Morocco. Int J Infect Dis. 2015;40:95–101.
Macroeconomics and health. investing in health for economic development. Report of the Commission on Macroeconomics and Health. Geneva: World Health Organization; 2001.
Nakamura MM, et al. Cost effectiveness of child pneumococcal conjugate vaccination in middle-income countries. Int Health. 2011;3(4):270–81.
Zigmond JPL, Tichopad A, Roberts CS., Jomaa I. Modeled outcomes and overall costs of the 13-valent pneumococcal conjugate vaccine in the Tunisia vacciantion program. In: ISPOR 17th Annual European Congress. 2014: Amsterdam, The Netherlands.
Earnshaw SR, et al. Cost-effectiveness of 2 + 1 dosing of 13-valent and 10-valent pneumococcal conjugate vaccines in Canada. BMC Infect Dis. 2012;12:101.
Klok RM, et al. Cost-effectiveness of a 10- versus 13-valent pneumococcal conjugate vaccine in Denmark and Sweden. Clin Ther. 2013;35(2):119–34.
Mucino-Ortega E, et al. Economic evaluation of an infant immunization program in Mexico, based on 13-valent pneumococcal conjugated vaccines. Value Health. 2010;14(5 Suppl 1):S65–70.
Strutton DR, et al. Cost-effectiveness of 13-valent pneumococcal conjugate vaccine: Germany, Greece, and The Netherlands. J Infect. 2012;64(1):54–67.
U.S. Census Bureau. International Programs, International Data Base. [cited 2017 March]; http://www.census.gov/population/international/data/idb/informationGateway.php. Accessed 1 Oct 2017.
World Health Organization. Immunization: diphtheria tetanus toxoid and pertussis (DTP3) by country. Global Health Observatory Data Repository. [cited 2017 March]. http://www.who.int/gho/immunization/dtp3/en/.
O’Brien KL, et al. Burden of disease caused by Streptococcus pneumoniae in children younger than 5 years: global estimates. Lancet. 2009;374(9693):893–902.
Teele DW, Klein JO, Rosner B. Epidemiology of otitis media during the first seven years of life in children in greater Boston: a prospective, cohort study. J Infect Dis. 1989;160(1):83–94.
Ray GT, et al. Cost-effectiveness of pneumococcal conjugate vaccine: evidence from the first 5 years of use in the United States incorporating herd effects. Pediatr Infect Dis J. 2006;25(6):494–501.
Black SB, et al. Effectiveness of heptavalent pneumococcal conjugate vaccine in children younger than five years of age for prevention of pneumonia. Pediatr Infect Dis J. 2002;21(9):810–5.
Fireman B, et al. Impact of the pneumococcal conjugate vaccine on otitis media. Pediatr Infect Dis J. 2003;22(1):10–6.
Griffin MR, et al. Declines in pneumonia hospitalizations of children aged < 2 years associated with the use of pneumococcal conjugate vaccines—Tennessee, 1998–2012. MMWR Morb Mortal Wkly Rep. 2014;63(44):995–8.
Greenberg D, et al. Impact of PCV7/PCV13 introduction on community-acquired alveolar pneumonia in children < 5 years. Vaccine. 2015;33(36):4623–9.
Griffin MR, et al. US hospitalizations for pneumonia after a decade of pneumococcal vaccination. N Engl J Med. 2013;369(2):155–63.
Pilishvili T, et al. Sustained reductions in invasive pneumococcal disease in the era of conjugate vaccine. J Infect Dis. 2010;201(1):32–41.
Zhou F, et al. Trends in acute otitis media-related health care utilization by privately insured young children in the United States, 1997–2004. Pediatrics. 2008;121(2):253–60.
Guevara M, et al. Direct, indirect and total effects of 13-valent pneumococcal conjugate vaccination on invasive pneumococcal disease in children in Navarra, Spain, 2001 to 2014: cohort and case-control study. Euro Surveill. 2016;21(14):30186.
The World Bank. Data: GDP per capita (current US$). [cited 2017 March]. http://data.worldbank.org/indicator/NY.GDP.PCAP.CD/countries/TN?display=graph.
Morrow A, et al. The burden of pneumococcal disease in the Canadian population before routine use of the seven-valent pneumococcal conjugate vaccine. Can J Infect Dis Med Microbiol. 2007;18(2):121–7.
Diez-Domingo J, et al. Pharmacoeconomic assessment of implementing a universal PCV-13 vaccination programme in the Valencian public health system (Spain). Vaccine. 2011;29(52):9640–8.
Gouveia EL, Reis JN, Flannery B. Clinical outcome of pneumococcal meningitis during the emergence of pencillin-resistant Streptococcus pneumoniae: an observational study. BMC Infect Dis. 2011;11:323.
Ordonez JE, Orozco JJ. Cost-effectiveness analysis of the available pneumococcal conjugated vaccines for children under five years in Colombia. Cost Eff Resour Alloc. 2015;13:6.
Waight PA, et al. Effect of the 13-valent pneumococcal conjugate vaccine on invasive pneumococcal disease in England and Wales 4 years after its introduction: an observational cohort study. Lancet Infect Dis. 2015;15(5):535–43.
Harboe ZB, et al. Impact of 13-valent pneumococcal conjugate vaccination in invasive pneumococcal disease incidence and mortality. Clin Infect Dis. 2014;59(8):1066–73.
Elam-Evans LD, et al. National, state, and selected local area vaccination coverage among children aged 19–35 months—United States, 2013. MMWR Morb Mortal Wkly Rep. 2014;63(34):741–8.
Acknowledgements
We thank Jan Zigmond, Ales Tichopad, and Ladislav Pecen for their contributions to the manuscript.
Funding
This study and associated publication charges were funded by Pfizer. All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Sarah J. Pugh is an employee of Pfizer. Mark A. Fletcher is an employee of Pfizer. Apostolos Charos is an employee of Pfizer. Lynda Imekraz is an employee of Pfizer. Matt Wasserman is an employee of Pfizer. Raymond Farkouh is an employee of Pfizer.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Data Availability
The data sets during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced digital features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.7381529.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Pugh, S.J., Fletcher, M.A., Charos, A. et al. Cost-Effectiveness of the Pneumococcal Conjugate Vaccine (10- or 13-Valent) Versus No Vaccination for a National Immunization Program in Tunisia or Algeria. Infect Dis Ther 8, 63–74 (2019). https://doi.org/10.1007/s40121-018-0226-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-018-0226-x