Abstract
We report the successful management of a patient with severe respiratory failure due to COVID-19 admitted to an intensive care unit complicated by secondary catheter-related infection of Candida glabrata. We are discussing some of the clinical challenges and the pitfalls in molecular diagnosis of SARS-CoV-2, including the fact that a positive PCR result may not always reflect infectiousness.
Similar content being viewed by others
Introduction
Coronavirus disease 2019 (COVID-19) was first detected in Wuhan, China, in January 2020 [1] and rapidly reached a pandemic level, causing more than three million cases and more than 200,000 deaths worldwide by the end of April. The first case in Austria was confirmed at the end of February 2020.
We report the successful management of the first patient with severe respiratory failure due to COVID-19 admitted to an intensive care unit (ICU) in Vienna, Austria, and would like to point out some of the clinical challenges and of the virological pitfalls of this complex disease.
Case report
A 72-year-old patient, whose past medical history included arterial hypertension on treatment with a calcium-channel blocker, depression, hyperlipidemia and in situ resection of carcinoma of the prostate in 2018, developed fever, nausea, malaise and vertigo. On the 17th of February, he was admitted to a municipal hospital, where the initial laboratory results showed a reduced white blood cell count (WBC) of 3200 G/l with a normal lymphocyte count, thrombocytopenia (106 G/l) and a slightly elevated C-reactive protein (CRP) of 25 mg/l (cut-off 5 mg/l). Influenza PCR from a nasopharyngeal swab and a urinary antigen test for legionella pneumophila were negative. Since a small pneumonic infiltration in the left lower lobe was suspected on the initial chest X-ray, and crepitations were auscultated in this area, the patient received empiric antibiotic therapy with intravenous cefuroxime for 7 days. During all this time, the patient did not complain of dyspnea or cough and remained completely stable. He and his wife denied having been abroad or having had contact with business partners or anybody else from China or Italy. Apart from unresolved weakness and reduced appetite, his clinical condition improved markedly, CRP levels declined to 8 mg/l and the follow-up chest X-ray was normal. Therefore, the discharge was planned for the next few days.
However, on the 23rd of February, the patient suddenly ran a high temperature (> 39 °C) and had severe chills. CRP levels were rising, several sets of blood cultures were collected, and influenza was ruled out again, as was urinary tract infection. On the next day, antibiotic therapy was switched to levofloxacin. Once more, the patient confirmed that he had only been in Austria in the last few weeks.
Two days later, the patient complained about shortness of breath for the first time, and on the chest X-ray bilateral pneumonic infiltrations could be seen. Due to rapid further respiratory deterioration in spite of the application of high-flow nasal oxygen, the patient had to be transferred to the intensive care unit on the same day, with the immediate necessity for endotracheal intubation and mechanical ventilation. Antibiotic therapy was escalated to high-dose meropenem plus doxycycline plus linezolid.
As the CT scan revealed massive pneumonic consolidations in all lung lobes (see Fig. 1) with ground-glass opacities, tracheal secretion was sent for SARS-CoV-2 PCR. This was in accordance with an official decree released on the 24th of February for surveillance purposes in pneumonia patients. The sample yielded a positive result on the 27th (ct-E: 36.2 swab).
Consequently, the patient was transferred to our specialized department of infectious diseases, for isolation in a negative-pressure room and for further management.
At the time of admission to our ICU, the patient was mechanically ventilated with a fraction of inspired oxygen of 45%, a PEEP of 13 and a Pmax of 20 mbar. He was analgosedated with moderate doses of propofol and remifentanil and received hemodynamic support with low-dose noradrenaline.
Laboratory results showed a normal absolute WBC, an increased neutrophil (82%) and a decreased lymphocyte count (10%), a normal platelet count, a CRP of 128 mg/l and normal liver and kidney function parameters. Troponin T was not elevated.
We continued antibiotic therapy and established experimental antiviral therapy with chloroquine 500 mg bid plus lopinavir/ritonavir 400/100 mg bid. At that time, it was not possible to administer remdesivir in a compassionate use program due to the study protocol (catecholamine use was an exclusion criterion).
Due to the negative PCR results of legionella, mycoplasma, chlamydia and MRSA, linezolid and doxycycline were discontinued 2 days later and therapy with meropenem was maintained. On day 2 after admission to our department, bronchoscopy indicated an inflamed mucous membrane with multiple red spots with small amounts of red-brown mucus. There was no growth of pathogens in bronchoalveolar lavage (BAL), and galactomannan in BAL and beta-d-glucan in serum were both negative.
After initially rising up to 226 mg/l, CRP decreased continuously from day 4 after admission to our department. LDH increased initially and went down from day 6, lymphocyte count rose from day 6 onwards. Catecholamines could be stopped on day 7. FiO2 could be decreased from day 4 on (at no time, there was a need for prone positioning), and pressure-controlled ventilation was switched to pressure supported ventilation on day 7. Eventually, fever dropped on day 8.
Due to a prolonged QTc interval up to 546 ms in the ECG check-up, experimental antiviral therapy had to be stopped after 4 days. Given the lack of virus clearance (detected in blood and tracheal secretion) and the ongoing critical state of the patient, therapy with remdesivir was started as compassionate use on day 8 and was given for 10 days (loading dose 200 mg on day 1, afterwards 100 mg once daily).
On day 10 the leukocyte count and CRP increased greatly. Additionally, the patient developed a recurrent fever with a body temperature of 38.6 °C. The respiratory and hemodynamic situation deteriorated, and hemodynamic support with noradrenaline had to be restarted on day 11.
While the CT scan showed a significant reduction of pneumonic consolidations (see Fig. 2) and the bronchoscopy was unremarkable, the culture of the removed central venous catheter was positive for Candida glabrata. Therefore, therapy with caspofungin was given for 14 days. Blood cultures remained sterile.
Subsequently, the clinical patient’s clinical condition improved significantly, the inflammation parameters decreased, fever resolved on day 14 and catecholamines could be discontinued on day 16.
Due to the prolonged weaning process, a tracheostomy was performed on day 14 without complications.
After two consecutive negative SARS-CoV-2 PCR results respiratory secretions and nasopharyngeal swabs and in the absence of fever for more than 48 h, the patient was no longer considered to be infectious and was transferred to another intensive care unit. There he showed signs of ongoing depression, hypoactive delirium and suspected critical illness polyneuropathy with marked motor weakness.
Finally, the weaning process was successful, and there was no further need of oxygen therapy from day 25.
Because of contact with a patient who later turned out to have COVID-19, nasopharyngeal swabs were obtained again and yielded a negative result on day 24, but a positive result on day 25. Consequently, the patient was re-transferred to our department for isolation purposes.
Serological analysis performed retrospectively of a stored serum sample obtained during the first week of admission already displayed detectable anti-SARS-CoV2-IgM (ratio 20.5, Wantai, Bejing, China) and IgA (ratio 2.83, Euroimmun, Lübeck, Germany), but negative IgG (ratio 0.79), and also yielded a weakly positive PCR signal. In the sample from the 26th, we observed a significant increase of IgM and IgA (ratios 35.66 and 9.41, respectively) and IgG seroconversion (ratio 4.48). Antibody kinetics not only verified the infection serologically but also indicated that early symptoms were probably related to SARS-CoV-2 infection.
When two more respiratory samples tested negative for SARS-CoV-2, and in consideration of the serological results, we deduced that the result mentioned before did not indicate re-infection or infectiousness. As a result, isolation measures could be terminated and the patient was transferred to a neurological rehabilitation ward to treat his critical illness polyneuropathy (confirmed by nerve conduction study and electromyography).
The patient recovered remarkably well and was finally discharged home after a total of 40 hospital days in a very good general condition, being able to breathe, drink, eat and walk independently.
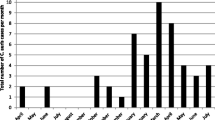
A summary of the course of disease of the patient is portrayed in Fig. 3.
Discussion
We report the case of a patient with severe COVID-19 complicated by secondary catheter-related infection of Candida glabrata. Prior to admission, the patient had been a physically and mentally fit non-smoker with no relevant comorbidities apart from arterial hypertension (well-controlled with amlodipine) and hyperlipidaemia.
A meta-analysis including over 45,000 patients with confirmed COVID-19 showed that hypertension is associated with more severe disease (odds ratio 2.36). Furthermore, older age has been shown to be an important independent predictor of severe course and mortality as well [2, 3].
Zhou et al. [4] reported in a retrospective, multicentre cohort study with 191 patients with confirmed COVID-19 that fever and cough were the most common initial symptoms, followed by malaise. Sepsis developed at a median of 9 days after start of symptoms, followed by severe respiratory insufficiency at day 12 and secondary infection at day 17. These reports fit the course of our patient: The first symptoms were fever, malaise and dry cough. He developed sepsis and ARDS 10 days and secondary infection 19 days after illness onset.
The alteration of the laboratory parameters, as listed in Table 1, was typical as well: elevated CRP, LDH, lymphocytopenia and thrombocytopenia. LDH increased initially but decreased from day 6 and lymphocyte increased from day 6 after admission to ICU. Both has been shown to be associated with favourable outcome [4].
After initial improvement, the patient’s clinical state deteriorated again on day 9 after admission to the ICU. Secondary infection has been reported in 15% of the patients with COVID-19 [4]. In our case, the patient suffered from catheter-related candidemia probably favoured by several courses of broad-spectrum antimicrobial therapy and by the necessity for parenteral nutrition due to the inability to administer enteral nutrition because of massive regurgitation (which in turn might be caused by viral affection of the gastrointestinal tract [5]). The mortality of candida spp. bloodstream infections has been reported to be as high as 30 [6] and up to 60% [7].
The patient showed signs of critical severe polyneuropathy after stopping the analgosedation. This stresses the importance of regular physiotherapy in patients suffering from COVID-19.
Administration of antiviral therapy proved difficult. At the time of admission to our department, it was not possible to start remdesivir in a compassionate use program because the study protocol excluded patients in need of catecholamine support. Lopinavir/ritonavir is known to elevate the plasma level of hydroxychloroquine leading to QT-prolongation [8]. In this case, the QT-prolongation required the termination of therapy. After catecholamine support could be tapered, remdesivir was given for 10 days.
The administration of intravenous remdesivir via a compassionate use programme may have accelerated viral clearance and thus have fastened clinical recovery.
While there is evidence of the in vitro efficacy of remdesivir against SARS-CoV-2 [9] and preliminary data about its clinical usefulness [10], definite proof of a clinical benefit in COVID-19 is still lacking due to the absence of large randomized-controlled trials. Recently, an under-powered randomized-controlled trial with no significant clinical benefit has been published [11].
Viral shedding, as listed in Table 2, took 21 days after illness onset which is in accordance with the cohort in the publication of Zhou et al. [4] (mean duration of 20 days in survivors). Antibodies were detected first on day 4 of the illness (positive IgA and IgM), and IgG could be detected from day 13 onwards.
Antibody levels against SARS-CoV-2 have been shown to correlate with disease severity, and the high IgG and IgA levels we detected in this patient further confirm this observation. The potential role of serological tests to determine the infection stage has also been highlighted.
In conclusion, this report highlights both successful clinical management of severe COVID-19 in a highly dedicated department and the pitfalls in molecular diagnosis of SARS-CoV-2, including the fact that a positive PCR result may not always reflect infectiousness.
References
World Health Organization. Novel coronavirus—China. 2020. http://www.who.int/csr/don/12-january-2020-novel-coronavirus-china/en/. Accessed 12 Apr 2020.
Yang J, Zheng Y, Gou X, et al. Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: a systematic review and meta-analysis. Int J Infect. 2020. https://doi.org/10.1016/j.ijid.2020.03.053.
Jordan RE, Adab P, Cheng KK. Covid-19: risk factors for severe disease and death. BMJ. 2020. https://doi.org/10.1136/bmj.m1198.
Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020. https://doi.org/10.1016/S0140-6736(20)30566-3.
Lamers MM, Beumer J, et al. SARS-CoV-2 productively infects human gut enterocytes. Science. 2020. https://doi.org/10.1126/science.abc1669.
David RA, et al. Impact of treatment strategy on outcomes in patients with Candidemia and other forms of invasive Candidiasis: a patient-level quantitative review of randomized trials. Clin Infect Dis. 2012. https://doi.org/10.1093/cid/cis021.
Fraser VJ, et al. Candidemia in a tertiary care hospital: epidemiology, risk factors, and predictors of mortality. Clin Infect. 1992. https://doi.org/10.1093/clind/15.3.414.
Kalil AC. Treating COVID-19—off-label drug use, compassionate use, and randomized clinical trials during pandemics. JAMA. 2020. https://doi.org/10.1001/jama.2020.4742.
Wang M, et al. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 2020. https://doi.org/10.1038/s41422-020-0282-0.
Grein J, et al. Compassionate use of remdesivir for patients with severe covid-19. N Engl J Med. 2020. https://doi.org/10.1056/NEJMoa2007016.
Wang Yeming, Zhang Dingyu, et al. Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial. Lancet. 2020. https://doi.org/10.1016/S0140-6736(20)31022-9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Seitz, T., Hoepler, W., Weseslindtner, L. et al. Successful management of the first reported case in Austria of COVID-19 with ARDS. Infection 48, 647–651 (2020). https://doi.org/10.1007/s15010-020-01458-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-020-01458-9