Abstract
Introduction
The incidence of Acinetobacter baumannii meningitis, which typically occurs after neurosurgery, has increased in recent years. Pediatric Acinetobacter baumannii meningitis due to the emergence of multidrug-resistant (MDR) and extensively drug-resistant (XDR) strains has important clinical significance.
Methodology
We retrospectively reviewed the clinical course and outcome of nine cases of meningitis due to Acinetobacter baumannii in children and reviewed the relevant literature.
Results
Seven patients had a history of neurosurgery, and the average time from the first surgery to cerebrospinal fluid (CSF) culture in these seven patients was 23.71 ± 17.43 days. Of all nine patients, four patients showed MDR isolates, two showed XDR isolates, and one showed pan-drug-resistant (PDR) isolates. Three patients received an intrathecal injection of amikacin. Two patients received intravenous colistin (5 mg/kg), and one received polymyxin B (2 mg/kg). The mean hospitalization duration was 39.44 days. Four patients eventually died: two with MDR Acinetobacter, one with PDR Acinetobacter, and one with susceptible Acinetobacter. Two of them still had positive CSF cultures at death.
Conclusion
Acinetobacter baumannii meningitis is usually associated with neurosurgery and the placement of foreign material, and it usually has a high mortality. Intrathecal or intraventricular polymyxin administration is expected to be an effective choice for meningitis but requires further study.
Similar content being viewed by others
Introduction
Acinetobacter is a Gram-negative coccus that is nonfermentative, strictly aerobic, catalase positive and oxidase negative. More than 30 genera [1] have been discovered, most of which are environmental microorganisms and have no human pathogenicity. Among them, Acinetobacter baumannii, Acinetobacter calcoaceticus, and Acinetobacter rufi are the most frequently reported strains. The term A. calcoaceticus–A. Baumannii (ACB) complex is also used because it is difficult to identify various Acinetobacter species based on phenotypic characteristics. ACB complexes include gene type 1 (Acinetobacter calcoaceticus), gene type 2 (Acinetobacter baumannii), gene type 3 and gene type 13TU [2]. Among them, Acinetobacter baumannii has the most clinical significance.
Acinetobacter baumannii can accumulate multiple drug resistance genes, resulting in multidrug resistance (MDR) and even pan-drug resistance to clinically used antibiotics. The resistance mechanisms often expressed in hospital Acinetobacter strains include β-lactamase [3], cell wall channels (porins) and efflux pump changes (cephalosporin, carbapenem, quinolone, tetracycline, chloramphenicol, and tigecycline resistance) [4]; gyrA and parC mutations (quinolone resistance) [5], aminoglycoside-modifying enzyme expression (aminoglycoside resistance); and PmrA and PmrB protein-coding gene mutations (polymyxin resistance) [6].
The most common clinical manifestations of Acinetobacter baumannii are ventilator-associated pneumonia and bloodstream infection [7], and Acinetobacter baumannii can also colonize the skin, wounds, respiratory tract and gastrointestinal tract. Acinetobacter baumannii is rare in nosocomial meningitis, but it has certain importance in postoperative meningitis. The risk factors are neurosurgical operation, head trauma, cerebrospinal fluid (CSF) leakage, wound infection, and foreign body implantation [8]. Acinetobacter baumannii meningitis has a high mortality rate of up to 15–71% [9]. Due to its limited treatments and poor prognosis (high mortality and neurological sequela rates), the clinical challenges are increasing. Pediatric Acinetobacter baumannii meningitis is relatively rare, and a lack of clinical cases, nonspecific clinical manifestations, poor therapeutic effects, poor prognosis, and its diagnosis and treatment present great challenges to pediatricians. In this paper, we retrospectively analyzed the clinical features, drug resistance spectrum and treatment experience of 9 children with Acinetobacter baumannii meningitis in this children’s hospital and review the relevant literature to improve the understanding of such diseases.
Materials and methods
Inclusion and exclusion criteria
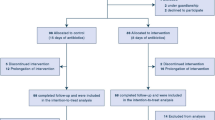
A retrospective review of all Acinetobacter baumannii (n = 3409) cases from the microbiology laboratory within a single regional teaching hospital, which has 1900 beds and a well-equipped pediatric intensive care unit (PICU), surgical intensive care unit (SICU), neonatal intensive care unit (NICU) and cardiac intensive care unit (CICU), between 1 July 2006 and 1 June 2018 was undertaken.
The inclusion criteria were as follows: (1) isolation of Acinetobacter baumannii from CSF; (2) increased white blood cells (≥ 10 × 106/L) and protein (≥ 450 mg/L) and decreased glucose (≤ 2.78 mmol/L) in the CSF; and (3) clinical evidence of central nervous system (CNS) infection, fever, headache, vomiting, confusion, irritability or meningeal irritation.
The exclusion criteria were as follows: (1) non-CSF specimen and (2) pseudomeningitis, in which the CSF is culture positive in the absence of clinical and laboratory features of meningitis.
Subjects
We retrospectively analyzed the following data: age, sex, underlying condition, invasive procedure, days from first neurosurgery to diagnosis, CSF culture, antibiotic resistance category, length of stay, duration of intravenous and intrathecal antibiotic treatment, time to CSF sterilization, and outcome. If the same child had multiple positive CSF cultures, we analyzed the data for the first instance.
Strain and drug sensitivity test
We used the VITEK2 compact (an automated microbial identification system) for strain identification and drug susceptibility testing. The minimum inhibitory concentration (MIC) was measured according to the AST-GN16 susceptibility card.
Antimicrobial susceptibilities
According to 2011 European and American antibiotic resistance consensus [10], Acinetobacter baumannii susceptibility test results can be divided into four categories, which are described below. Common antibacterial agents for Acinetobacter baumannii include broad-spectrum cephalosporins (ceftazidime, cefepime), anti-Pseudomonas carbapenems (imipenem, meropenem), enzyme inhibitors (ampicillin sulbactam, piperacillin tazobactam, cefoperazone sulbactam), fluoroquinolones (ciprofloxacin, levofloxacin), aminoglycosides (gentamicin, tobramycin, amikacin), polymyxin (colistin, polymyxin B), and tigecycline. The four categories are as follows: MDR, resistant to at least three types of antimicrobial agents; extensively drug-resistant (XDR), resistant to most of the above drugs and sensitive to only one or two antibiotics; pan-drug-resistant (PDR), resistant to all of the above antibacterial drugs; and susceptible Acinetobacter (SA), sensitive to most of the above drugs.
Results
Basic characteristics (Table 1)
Among the 3409 specimens, 21 positive CSF samples were observed in 9 children: 6 males and 3 females. The male:female ratio was 2:1, and the average patient age was 52.70 ± 48.14 months. Seven patients (77.8%) had a history of neurosurgery, and the average time from the first surgery to CSF culture in 7 patients was 23.71 ± 17.43 days. The Acinetobacter baumannii drug susceptibility test showed that there were four MDR cases, two XDR cases, one PDR case, and two SA cases. The average hospital stay was 39.44 days. Four patients eventually died: two with MDR Acinetobacter, one with PDR Acinetobacter and one with an SA isolate.
Clinical manifestation and laboratory examination
Nine patients had clinical manifestations of fever, vomiting, and disturbance of consciousness, and five patients had convulsions. The CSF showed an increased white cell count, with an average of 483.11 × 106/L (10-2780 × 106/L), with neutrophils as the main contributor, and decreased sugar, with an average content of 0.34 mmol/L (0.05–0.94 mmol/L). The chloride content decreased, and the protein content increased, averaging 3002.98 mg/L (754.9–7499 mg/L). Peripheral blood routinely showed an increased white blood cell count, mostly consisting of neutrophils, and an increased C-reactive protein (CRP) level, averaging 47.4 mg/L (15.5–110 mg/L).
Mixed other infections
Corynebacterium and Penzantella were found in the CSF of one patient. In three cases, Acinetobacter baumannii was also found in sputum samples.
Antimicrobial susceptibilities
The resistance of Acinetobacter baumannii to clinical first-line antibiotics and antibiotic selection in nine cases is shown in Table 2. In one case each, Acinetobacter baumannii was only sensitive to amikacin and ceftazidime, polymyxin and amikacin, polymyxin and tigecycline, amikacin and tobramycin, amikacin, and tigecycline. In addition, Acinetobacter baumannii was only moderately sensitive to tigecycline in one case.
Treatment and prognosis
In addition to the two cases of neonatal septicemia, the other seven cases who had terrible underlying conditions received antibiotics to prevent perioperative infection or underwent anti-infective treatment before the diagnosis of meningitis. Among these cases, four cases received meropenem combined with vancomycin, two cases received ceftriaxone, and one case received piperacillin tazobactam. When the CSF culture was positive, the treatment plan was actively adjusted according to the drug sensitivity test. Although case 5, with a diagnosis of neonatal sepsis, was only sensitive to aminoglycosides, antibiotics were not changed due to the large side effects of the drug and its good clinical treatment effect. The antibiotics were adjusted for the remaining eight patients. See Table 2 for details. Although the susceptibility test for polymyxin was not routinely performed, our clinical pediatricians tried polymyxin in three patients based on the latest clinical experience and achieved good clinical results. Two patients received intravenous colistin (5 mg/kg) and one received polymyxin B (2 mg/kg); all CSF culture turned negative. Three patients received an intrathecal injection of amikacin according to the drug susceptibility results. The drainage tubes of six patients were removed. Four children died, two of whom still had positive CSF cultures.
Discussion and literature review
Acinetobacter meningitis mainly occurs after neurosurgery, and the risk factors include long neurosurgical operations, CSF leakage, incision infection, foreign body implantation, external ventricle drain (EVD) placement, multiple operations, and previous antibiotic treatments [8]. A targeted literature search was performed on PubMed, the Cochrane Library database and the World of Science. Relevant publications in English published before 1 July 2018 were found through a search on PubMed using the following key search terms: “Acinetobacter baumannii,” “meningitis,” “intracranial infection,” and “neurosurgery.” Summarized below are 16 articles that describe 33 pediatric cases (Table 3) [11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26]. Some of the 16 articles did not provide all of the information that is described below. Among the known information, there are 13 males and 10 females, aged from newborn to 16 years, with an average age of 57.96 ± 66.32 months. All underwent neurosurgical procedures, and eleven patients underwent EVD placement. Eventually five patients (15.2%) died. These findings are consistent with our case summary results. Seven of our nine patients underwent neurosurgical procedures, and six patients underwent EVD placement. Our case report and literature review have effectively demonstrated that outside the neonatal period, Acinetobacter baumannii meningitis was associated with neurosurgery and the placement of foreign material, such as an EVD.
The clinical manifestations of Acinetobacter meningitis are similar to those reported for meningitis. Most patients present with fever, convulsions, meningeal irritation, and local signs of nervous system disturbances. The CSF typically shows an increased white blood cell count, mainly neutrophils, and biochemical indicators of decreased glucose levels and significantly increased protein levels. However, it is still necessary to exclude pseudomeningitis caused by CSF specimen contamination [27], as indicated by a positive CSF culture in the absence of clinical and laboratory features of meningitis. Two of our nine patients did not undergo neurosurgery but were included because these two children were neonates with fever, convulsions and bulging of the anterior fontanelle, and their CSF samples showed increases in the white cell count and protein level.
The appearance of Acinetobacter MDR, XDR and even PDR strains makes treatment very difficult and seriously threatens patient survival. Among our nine patients, most isolates were resistant to multiple classes of antimicrobials: there were four MDR cases, two XDR cases and one PDR case. In 7 of 8 patients in the retrospective studies by Saleem et al. [23], MDR Acinetobacter baumannii was cultured in the CSF. These case reports reflect the increasing resistance of Acinetobacter baumannii, and there may be no effective medicine in the future. In addition, Acinetobacter baumannii meningitis is usually associated with a high mortality, and the mortality rate of our 9 children approached 50%. Although whether the high mortality rate can be completely attributed to Acinetobacter infection is unclear and the severity of the intracranial injury itself also affects the prognosis, this mortality rate sounds the alarm for all pediatricians.
The rational selection of antibacterial drugs is crucial for neurosurgical Acinetobacter baumannii meningitis. For the first-line treatment, the carbapenem meropenem is the most commonly recommended empirical treatment, but its resistance rate exceeds 40% with carbapenem-resistant strains [28]. For such resistant Acinetobacter, polymyxin has been successful. However, polymyxin has a poor solubility in the CNS. When administered intravenously, its CSF level can only reach approximately 25% that of the serum level [18]; thus, it can be administered intrathecally or intraventricularly, combined with intravenous medications for these resistant Acinetobacter strains [29]. There are no unified standards for the intrathecal or intraventricular administration of polymyxin, and the relevant literature reports a wide range of doses. The recommended total daily dose should be from 0.75 to 7.5 mg colistin base activity (25,000–250,000 U polymyxin E sodium methanesulfonate) [19]. In 2004, the American Society of Infectious Diseases recommended a dose of intraventricular colistin of 125,000 U (10 mg) [30]. Possible complications of intraventricular or intrathecal administration include aseptic chemical meningitis or ventriculitis, but this neurotoxicity is dose-dependent and reversible [31].
Among our nine patients, two patients received colistin (5 mg/kg), and one received polymyxin B (2 mg/kg); their CSF cultures turned negative. Three patients received an intrathecal injection of amikacin (10–15 mg/day) according to the drug susceptibility test results, and two CSF culture turned negative; however, two patients still died. Therefore, the effect is not significant. Of the 4 patients who died, two still had positive CSF cultures, and the days to CSF sterilization of the other 2 patients were very high, with an average of 18.5 days. Thus, CSF sterilization is very difficult to achieve. However, this retrospective study still found many shortcomings in terms of clinical experience. There were discrepancies between our selection of antibiotics and the international recommendations. These discrepancies may be due to the rarity of pediatric Acinetobacter baumannii meningitis cases and the difficulty of obtaining polymyxins. Additionally, the polymyxin susceptibility tests were unconventional because our AST-GN16 susceptibility card does not routinely include polymyxin, and the bacterial laboratory does not have an additional polymyxin test strip. Few reports have described intrathecal antibiotic treatments, and there is no consensus regarding the dose. The treatment of Acinetobacter meningitis should last for at least 3 weeks [19] and should be thoroughly evaluated by clinical tests and repeated CSF cultures.
Conclusion
Acinetobacter baumannii meningitis occurs mostly after neurosurgery and is usually associated with the placement of foreign material, such as an EVD, and a high mortality rate. Most of our patients had cultured MDR strains. Therefore, antibiotic selection is challenging due to the appearance of MDR and even PDR bacteria. Early diagnosis and treatment are critical. However, it is very difficult to achieve CSF sterilization. Polymyxins are safe and effective for the treatment of Acinetobacter baumannii meningitis, and intrathecal or intraventricular administration is expected to be an effective choice for meningitis, but this drug still needs to be subjected to further clinical studies.
References
Dijkshoorn L, van der Toorn J. Acinetobacter species: which do we mean? Clin Infect Dis. 1992;15:748–9.
Zarrilli R, Giannouli M, Tomasone F, Triassi M, Tsakris A. Carbapenem resistance in Acinetobacter baumannii: the molecular epidemic features of an emerging problem in health care facilities. J Infect Dev Ctries. 2009;3:335–41.
Mugnier P, Poirel L, Pitout M, Nordmann P. Carbapenem-resistant and OXA-23-producing Acinetobacter baumannii isolates in the United Arab Emirates. Clin Microbiol Infect. 2008;14:879–82. https://doi.org/10.1111/j.1469-0691.2008.02056.x.
Peleg AY, Adams J, Paterson DL. Tigecycline efflux as a mechanism for nonsusceptibility in Acinetobacter baumannii. Antimicrob Agents Chemother. 2007;51:2065–9. https://doi.org/10.1128/AAC.01198-06.
Bonomo RA, Szabo D. Mechanisms of multidrug resistance in Acinetobacter species and Pseudomonas aeruginosa. Clin Infect Dis. 2006;43:49–56. https://doi.org/10.1086/504477.
Adams MD, Nickel GC, Bajaksouzian S, Lavender H, Murthy AR, Jacobs MR, et al. Resistance to colistin in Acinetobacter baumannii associated with mutations in the PmrAB two-component system. Antimicrob Agents Chemother. 2009;53:3628–34. https://doi.org/10.1128/AAC.00284-09.
Munoz-Price LS, Weinstein RA. Acinetobacter infection. N Engl J Med. 2008;358:1271–81. https://doi.org/10.1056/NEJMra070741.
Korinek AM, Baugnon T, Golmard JL, van Effenterre R, Coriat P, Puybasset L. Risk factors for adult nosocomial meningitis after craniotomy role of antibiotic prophylaxis. Neurosurgery. 2006;59:126–33. https://doi.org/10.1227/01.neu.0000243291.61566.21.
Kim BN, Peleq AY, Lodise TP, Lipman J, Li J, Nation R, et al. Management of meningitis due to antibiotic-resistant Acinetobacter species. Lancet Infect Dis. 2009;9:245–55. doi:https://doi.org/10.1016/S1473-3099(09)70055-6.
Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18:268–81. https://doi.org/10.1111/j.1469-0691.2011.03570.x.
Hook EB, Aase JM. Herellea meningitis following ventriculography. Am J Dis Child. 1964;108:452–3.
Yogev R. Ventriculitis from Acinetobacter calcoaceticus variant anitratus. J Neurol Neurosurg Psychiatry. 1979;42:475–7.
Wirt TC, McGee ZA, Oldfield EH, Meacham WF. Intraventricular administration of amikacin for complicated Gram-negative meningitis and ventriculitis. J Neurosurg. 1979;50:95–9. https://doi.org/10.3171/jns.1979.50.1.0095.
Kelkar R, Gordon SM, Giri N, Rao K, Ramakrishnan G, Saikia T, et al. Epidemic iatrogenic Acinetobacter spp. meningitis following administration of intrathecal methotrexate. J Hosp Infect. 1989;14:233–43.
Kaplan SL, Patrick CC. Cefotaxime and aminoglycoside treatment of meningitis caused by gram-negative enteric organisms. Pediatr Infect Dis J. 1990;9:810–4.
Siegman-Igra Y, Bar-Yosef S, Gorea A, Avram J. Nosocomial acinetobacter meningitis secondary to invasive procedures: report of 25 cases and review. Clin Infect Dis. 1993;17:843–9.
Fernandez-Viladrich P, Corbella X, Corral L, Tubau F, Mateu A. Successful treatment of ventriculitis due to carbapenem-resistant Acinetobacter baumannii with intraventricular colistin sulfomethate sodium. Clin Infect Dis. 1999;28:916–7. https://doi.org/10.1086/517243.
Jimenez-Mejias ME, Pichardo-Guerrero C, Marquez-Rivas FJ, Martin-Lozano D, Prados T, Pachon J. Cerebrospinal fluid penetration and pharmacokinetic/pharmacodynamic parameters of intravenously administered colistin in a case of multidrug-resistant Acinetobacter baumannii meningitis. Eur J Clin Microbiol Infect Dis. 2002;21:212–4. https://doi.org/10.1007/s10096-001-0680-2.
Ng J, Gosbell IB, Kelly JA, Boyle MJ, Ferguson JK. Cure of multiresistant Acinetobacter baumannii central nervous system infections with intraventricular or intrathecal colistin: case series and literature review. J Antimicrob Chemother. 2006;58:1078–81. https://doi.org/10.1093/jac/dkl347.
Lee SY, Lee JW, Jeong DC, Chung SY, Chung DS, Kang JH. Multidrug-resistant Acinetobacter meningitis in a 3-year-old boy treated with i.v. colistin. Pediatr Int. 2008;50:584–5. https://doi.org/10.1111/j.1442-200X.2008.02677.x.
Dalgic N, Ceylan Y, Sancar M, Telhan L, Kafadar I, Cavusoglu H, et al. Successful treatment of multidrug-resistant Acinetobacter baumannii ventriculitis with intravenous and intraventricular colistin. Ann Trop Paediatr. 2009;29:141–7. https://doi.org/10.1179/146532809X440761.
Ozdemir H, Tapisiz A, Ciftci E, Ince E, Mokhtari H, Guriz H, et al. Successful treatment of three children with post-neurosurgical multidrug-resistant Acinetobacter baumannii meningitis. Infection. 2010;38:241–4. https://doi.org/10.1007/s15010-010-0018-z.
Saleem AF, Shah MS, Shaikh AS, Mir F, Zaidi AK. Acinetobacter species meningitis in children: a case series from Karachi, Pakistan. J Infect Dev Ctries. 2011;5:809–14.
Alaoui SY, Nejmi SE, Chakir AA, Hmamouchi B, Chlilek A. Intraventricular colistin use in neonatal meningitis caused by Acinetobacter baumanii. Ann Fr Anesth Reanim. 2011;30:854–5. https://doi.org/10.1016/j.annfar.2011.07.008.
Wang JH, Lin PC, Chou CH, Ho CM, Lin KH, Tsai CT, et al. Intraventricular antimicrobial therapy in postneurosurgical Gram-negative bacillary meningitis or ventriculitis: a hospital-based retrospective study. J Microbiol Immunol Infect. 2014;47:204–10. https://doi.org/10.1016/j.jmii.2012.08.028.
Ni S, Li S, Yang N, Zhang S, Hu D, Li Q, et al. Post-neurosurgical meningitis caused by Acinetobacter baumannii: case series and review of the literature. Int J Clin Exp Med. 2015;8:21833–8.
Gusten WM, Hansen EA, Cunha BA. Acinetobacter baumannii pseudomeningitis. Heart Lung. 2002;31:76–8.
Metan G, Alp E, Aygen B, Sumerkan B. Carbapenem-resistant Acinetobacter baumannii: an emerging threat for patients with post-neurosurgical meningitis. Int J Antimicrob Agents. 2007;29:112–3. https://doi.org/10.1016/j.ijantimicag.2006.08.035.
Benifla M, Zucker G, Cohen A, Alkan M. Successful treatment of Acinetobacter meningitis with intrathecal polymyxin E. J Antimicrob Chemother. 2004;54:290–2. https://doi.org/10.1093/jac/dkh289.
Tunkel AR, Hartman BJ, Kaplan SL, Kaufman BA, Roos KL, Scheld WM, et al. Practice guidelines for the management of bacterial meningitis. Clin Infect Dis. 2004;39:1267–84. https://doi.org/10.1086/425368.
Landman D, Georgescu C, Martin DA, Quale J. Polymyxins revisited. Clin Microbiol Rev. 2008;21:449–65. https://doi.org/10.1128/CMR.00006-08.
Funding
Sheng Ye received grants from the Zhejiang Medical and Health Science and Technology Plan Project (2007 B119, 2012 KYB119) and the Natural Science Foundation of Zhejiang Province (LY12 H19006).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Availability of data and materials
Data sharing is applicable to this article, and we wish to share our data.
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Xiao, J., Zhang, C. & Ye, S. Acinetobacter baumannii meningitis in children: a case series and literature review. Infection 47, 643–649 (2019). https://doi.org/10.1007/s15010-018-1234-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-018-1234-1