Abstract
Purpose
Migrants represent a considerable proportion of HIV diagnoses in Europe and are considered a group at risk of late presentation. This study examined the incidence of HIV diagnoses and the risk of late presentation according to migrant status, ethnic origin and duration of residence.
Methods
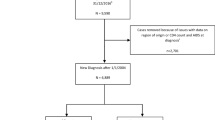
We conducted a historically prospective cohort study comprising all adult migrants to Denmark between 1.1.1993 and 31.12.2010 (n = 114.282), matched 1:6 to Danish born by age and sex. HIV diagnoses were retrieved from the National Surveillance Register and differences in incidence were assessed by Cox regression model. Differences in late presentation were assessed by logistic regression.
Results
Both refugees (HR = 5.61; 95% CI 4.45–7.07) and family-reunified immigrants (HR = 10.48; 95% CI 8.88–12.36) had higher incidence of HIV diagnoses compared with Danish born and the incidence remained high over time of residence for both groups. Migrants from all regions, except Western Asia and North Africa, had higher incidence than Danish born. Late presentation was more common among refugees (OR = 1.87; 95% CI 1.07–3.26) and family-reunified immigrants (OR = 2.30; 95% CI 1.49–3.55) compared with Danish born. Southeast Asia and Sub-Saharan Africa were the only regions with a higher risk of late presentation. Late presentation was only higher for refugees within 1 year of residence, whereas it remained higher within 10 years of residence for family-reunified immigrants.
Conclusions
This register-based study revealed a higher incidence of HIV diagnoses and late presentation among migrants compared with Danish born and the incidence remained surprisingly high over time.
Similar content being viewed by others
References
Statistics Denmark. Immigrants in denmark. Statistics Denmark, Copenhagen; 2015.
Norredam M, Nielsen SS, Krasnik A. Migrants’ utilization of somatic healthcare services in Europe—a systematic review. Eur J Public Health. 2010;20:555–63.
Norredam M. Migrants’ access to healthcare. Dan Med Bull. 2011;58(10):B4339
WHO. HIV/AIDS Key facts [Internet]. [cited 2016 Oct 14]. Available from: http://www.who.int/mediacentre/factsheets/fs360/en/.
European Centre for Disease Prevention and. Control ECDC. Assessing the burden of key infectious diseases affecting migrant populations in the EU/EEA. Tech. Rep. 2014.
Mocroft A, Lundgren JD, Sabin ML, d’Arminio Monforte A, Brockmeyer N, Casabona J, et al. Risk factors and outcomes for late presentation for HIV-positive persons in Europe: results from the collaboration of observational HIV Epidemiological Research Europe Study (COHERE). PLoS Med. 2013;10.
Christiansen A, Cowan SHIV. 2016. EPI-News No. 36. [Internet]. 2017 [cited 2017 Sep 28]. Available from: https://www.ssi.dk/English/News/EPI-NEWS/2017/No 36–2017.aspx.
Sobrino-Vegas P, Moreno S, Rubio R, Viciana P, Bernardino JI, Blanco JR, et al. Impact of late presentation of HIV infection on short-, mid- and long-term mortality and causes of death in a multicenter national cohort: 2004–2013. J Infect. 2016;72:587–96.
Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365:493–505.
Sabin CA, Smith CJ, Gumley H, Murphy G, Lampe FC, Phillips AN, et al. Late presenters in the era of highly active antiretroviral therapy. Aids. 2004;18:2145–51.
Spallek J, Zeeb H, Razum O. What do we have to know from migrants’ past exposures to understand their health status? a life course approach. Emerg Themes Epidemiol BioMed Central Ltd. 2011;8:6.
Alvarez-Del Arco D, Monge S, Azcoaga A, Rio I, Hernando V, Gonzalez C, et al. HIV testing and counselling for migrant populations living in high-income countries: a systematic review. Eur J Public Health. 2013;23:1039–45.
Schäfer G, Kreuels B, Schmiedel S, Hertling S, Hüfner A, Degen O, et al. High proportion of HIV late presenters at an academic tertiary care center in northern Germany confirms the results of several cohorts in Germany: time to put better HIV screening efforts on the national agenda? Infection. 44. Berlin Heidelberg: Springer; 2016. pp. 347–52.
Hernando V, Alvárez-del Arco D, Alejos B, Monge S, Amato-Gauci AJ, Noori T, et al. HIV Infection in Migrant Populations in the European Union and European Economic Area in 2007–2012. JAIDS. 2015;70:204–11.
Norredam M, Agyemang C, Hoejbjerg Hansen OK, Petersen JH, Byberg S, Krasnik A, et al. Duration of residence and disease occurrence among refugees and family reunited immigrants: Test of the “healthy migrant effect” hypothesis. Trop Med Int Heal. 2014;19:958–67.
Antinori A, Coenen T, Costagiola D, Dedes N, Ellefson M, Gatell J, et al. Late presentation of HIV infection: a consensus definition. HIV Med. 2011;12:61–4.
Division UNS. Standard country and area codes classifications (M49). Available from: https://unstats.un.org/unsd/methodology/m49/.
AM HFD. The changing face of the HIV epidemic in Western Europe: what are the implications for public health policies? Lancet. 2004;364:83–94.
Chadborn TR, Delpech VC, Sabin CA, Sinka K, Evans BG. The late diagnosis and consequent short-term mortality of HIV-infected heterosexuals. 2006;2000–4.
European Centre for Disease Prevention. and Control (ECDC). HIV/AIDS surveillance in Europe 2014. 2015.
Op de Coul ELM, van Sighem A, Brinkman K, Benthem BH van, Ende ME van der, Geerlings S, et al. Factors associated with presenting late or with advanced HIV disease in the Netherlands, 1996–2014: results from a national observational cohort. BMJ Open. 2016;6:e009688.
Hachfeld A, Ledergerber B, Darling K, Weber R, Calmy A, Battegay M, et al. Reasons for late presentation to HIV care in Switzerland. J Int AIDS Soc. 2015;18:1–8.
Helleberg M, Engsig FN, Kronborg G, Laursen AL, Pedersen G, Larsen O, et al. Late presenters, repeated testing, and missed opportunities in a Danish nationwide HIV cohort. Scand J Infect Dis. 2012;44:282–8.
Brännström J, Svedhem Johansson V, Marrone G, Wendahl S, Yilmaz A, Blaxhult A, et al. Deficiencies in the health care system contribute to a high rate of late HIV diagnosis in Sweden. HIV Med. 2016;17:425–35.
Sulis G, El Hamad I, Fabiani M, Rusconi S, Maggiolo F, Guaraldi G, et al. Clinical and epidemiological features of HIV/AIDS infection among migrants at first access to healthcare services as compared to Italian patients in Italy: a retrospective multicentre study, 2000–2010. Infection. 2014;42:859–67.
Hønge BL, Jespersen S, Aunsborg J, Mendes DV, Medina C, Té D da. S, et al. High prevalence and excess mortality of late presenters among HIV-1, HIV-2 and HIV-1/2 dually infected patients in Guinea-Bissau - A cohort study from West Africa. Pan Afr Med J. 2016;25:1–13.
Jeong SJ, Italiano C, Chaiwarith R, Ng OT, Vanar S, Jiamsakul A, et al. Late Presentation into Care of HIV Disease and Its Associated Factors in Asia: Results of TAHOD. AIDS Res Hum Retroviruses. 2016;32:255–61.
Blondell SJ, Kitter B, Griffin MP, Durham J. Barriers and Facilitators to HIV Testing in Migrants in High-Income Countries: a systematic review. Aids Behav. 2015;19:2012–24.
Alberer M, Malinowski S, Sanftenberg L, Schelling J. Notifiable infectious diseases in refugees and asylum seekers: experience from a major reception center in Munich, Germany. Infection. 2018;46:375–83.
European Centre for Disease Prevention and Control (ECDC), WHO Regional Office for Europe. Migrant health: access to HIV prevention, treatment and care for migrant populations in EU/EEA countries. Stockholm, ECDC 2009; p 35.
Internation Organization for Migration (IOM). Assisting Quota Refugees for Resettlement to Denmark. 2006. Available from: https://www.iom.int/jahia/webdav/site/myjahiasite/shared/shared/mainsite/projects/showcase_pdf/Denmarkcases.pdf
Frederiksen HW, Norredam M. Sundhedsforhold hos nyankomne indvandrere—En rapport fra Forskningscenter for Migration, Etnicitet og Sundhed. Forskningscenter for Migration, Etnicitet og Sundhed (MESU), København, 2012;3–53. (In Danish).
Frederiksen HW, Krasnik A, Nørredam M. Policies and practices in the health-related reception of quota refugees in Denmark. Dan Med J. 2012;59:A4352.
United Nations High Commissioner for Refugees. Policy Statement on HIV Testing and Counselling in Health Facilities for Refugees, Internally Displaced Persons and other Persons of Concern to UNHCR. 2009;21. Available from: http://www.who.int/hiv/pub/vct/unhcr.pdf?ua=1.
Fakoya I, Álvarez-del Arco D, Woode-Owusu M, Monge S, Rivero-Montesdeoca Y, Delpech V, et al. A systematic review of post-migration acquisition of HIV among migrants from countries with generalised HIV epidemics living in Europe: implications for effectively managing HIV prevention programmes and policy. BMC Public Health BMC Public Health. 2015;15:561.
Quota refugees [Internet]. Danish Immigr. Serv. [cited 2016 Oct 14]. Available from: https://www.nyidanmark.dk/en-us/coming_to_dk/asylum/quota_refugees.htm.
Funding
None.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Standards
The project was approved by the Danish Protection Agency (No 2012-41-0065). Further ethical approval regarding registry-based research is not required in Denmark. The data set was made available and analysed in an anonymous form by remote online access to the data set stored at Statistics Denmark.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Deen, L., Cowan, S., Wejse, C. et al. Refugees and family-reunified immigrants have a high incidence of HIV diagnosis and late presentation compared with Danish born: a nationwide register-based cohort study. Infection 46, 659–667 (2018). https://doi.org/10.1007/s15010-018-1167-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-018-1167-8