Abstract
Purpose
The incidence of Staphylococcus aureus skin and soft tissue infection (SSTI) is high in sub-Saharan Africa. This is fueled by a high prevalence of Panton-Valentine leukocidin (PVL), which can be associated with necrotizing disease. The aim was to describe the clinical presentation and the treatment of SSTI in the African setting and to identify challenges in the management.
Methods
Patients (n = 319) were recruited in DR Congo (n = 56, 17.6%), Gabon (n = 89, 27.9%), Mozambique (n = 79, 24.8%) and Tanzania (n = 95, 29.8%) during the prospective observational StaphNet cohort study (2010–2015). A physician recorded the clinical management in standardized questionnaires and stratified the entity of SSTI into superficial (sSSTI) or deep-seated (dSSTI). Selected virulence factors (PVL, β hemolysin) and multilocus sequence types (MLST) were extracted from whole genome sequencing data.
Results
There were 220/319 (69%) sSSTI and 99/319 (31%) dSSTI. Compared to sSSTI, patients with dSSTI were more often hospitalized (13.2 vs. 23.5%, p = 0.03), HIV-positive (7.6 vs. 15.9%, p = 0.11), and required more often incision and drainage (I&D, 45.5 vs. 76.5%, p = 0.04). The proportion of an adequate antimicrobial therapy increased marginally from day 1 (empirical therapy) to day 3 (definite therapy), for sSSTI (70.7 to 72.4%) and dSSTI (55.4 to 58.9%). PVL was a risk factor for I&D (OR = 1.7, p = 0.02) and associated with MLST clonal complex CC121 (OR = 2.7, p < 0.001).
Conclusion
Appropriate antimicrobial agents and surgical services to perform I&D were available for the majority of patients. Results from susceptibility testing should be considered more efficiently in the selection of antimicrobial therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Staphylococcus aureus is part of the normal flora of animals and humans. At the same time, it is one of the most common invasive pathogens leading to high morbidity and mortality both in the community and hospital setting. For instance, S. aureus is the leading cause of skin and soft tissue infection (SSTI), infective endocarditis or osteomyelitis [1].
The most common S. aureus diseases in the community setting are SSTI such as impetigo, cellulitis, abscesses, necrotizing fasciitis, or pyomyositis [1]. The incidence of community-acquired SSTI increased in several countries (e.g. USA, UK, Australia) in the past decades [1]. In the USA, the annual incidence of SSTI increased from 32.1 (1997) to 48.1 (2005) per 1000 individuals [2]. The standard treatment depends on the entity and severity of infection. Incision and drainage (I&D) of purulent infection sites should be done always; adjunctive antibiotics should be considered in moderate (e.g. systemic signs of infection) and severe disease (e.g. immunosuppression, failed initial antimicrobial treatment, signs and symptoms of shock) [1, 3]. In non-purulent infection (e.g. necrotizing fasciitis, cellulitis, erysipelas), antibiotics are always recommended, with or without debridement [3].
Staphylococcus aureus has numerous virulence factors but only a few have been clearly linked with SSTI such as α hemolysin (HLA), Panton-Valentine leukocidin (PVL) or phenol-soluble modulins (PSM) [1, 4, 5]. The prevalence of PVL among S. aureus from Africa is higher (17–74%) as compared to Germany (3%), or the UK (3.7%) [6,7,8]. This might be reflected by a higher annual incidence of SSTI in infants in Gabon (1572 per 100,000) compared to the US (452 per 100,000) [9, 10]. Noteworthy, also healthy travelers have more frequently SSTI caused by PVL-positive S. aureus after returning from the tropics [11]. However, it is likely that not only PVL but also additional factors [e.g. HLA, β hemolysin (HLB)] contribute to the severity of SSTI in sub-Saharan Africa [12, 13]. Despite the high burden of SSTI and the alarmingly high levels of PVL-positive S. aureus, little is known about the management of SSTI in Africa. The aim of this study was, therefore, to analyze the treatment of SSTI in different settings across four sub-Saharan African countries linked together by the StaphNet consortium network [14] and to identify challenges in the diagnostic and therapeutic management of patients.
Materials and methods
Ethical clearance
We received ethical clearance from the institutional review boards of each participating institution (ethics committee of the University of Kinshasa (ESP/CO/070/2012 and ESP/CO/070b/2014), Ministry of Health and Social Welfare of Tanzania (A 81-2009), Institutional Ethics Committee of the Medical Research Unit of the International Foundation of the Albert Schweitzer Hospital (CERIL 15/09), Mozambican National Committee on Bioethics for Health (IRB00002657, Ref. 325/CNBS/12), Ethics Committee of the University of Münster (2009-227-b-S), Ethics Committee of Freiburg (248/09_120491) and the Ethics Committee of the Chamber of Physicians of Saarland (19/09). Each participant or its guardian if underage provided a written informed consent.
Study design
We performed a prospective observational multi-center cohort study in 2010–2015. Patients were recruited in the framework of the German-African StaphNet cooperation on staphylococcal disease in Bagamoyo (Tanzania), Kinshasa (Democratic Republic of the Congo), Lambaréné (Gabon) and Manhiça (Mozambique) [14]. We used a standardized questionnaire to assess systematically the infrastructure at the four study sites for the management of S. aureus SSTI infections. The questionnaire items included commercially available antimicrobial agents and its costs, healthcare insurance, turn-around time for antimicrobial test results, follow-up visits after starting an antimicrobial therapy, availability of a surgical service for I&D, the total number of admission and the total number of blood cultures sent for microbiological analysis. The Principal Investigator (ASA, TK, ML, IM) collected the data from each study site. Study sites were anonymized by a number code when reporting questionnaire results.
Patients and clinical management
The inclusion criterion was a culture-confirmed and community-acquired S. aureus SSTI (i.e. S. aureus had to be isolated in the community setting or up to 48 h after admission including at a transferal hospital). No exclusion criteria were applied. A standardized questionnaire was used to record demographic data (sex, age), the clinical presentation judged by a physician (e.g. severe sepsis/septic shock [assessed according to definitions of the ACCP/SCCM consensus conference [15], site of infection) and outcome on day 14 (admission, 14-day mortality, surgical treatment such as I&D). The HIV-status was recorded as reported by the patient. The physician stratified the SSTI into superficial infections [sSSTI; e.g. impetigo, ecthyma, folliculitis, cellulitis, erysipelas, superficial abscess (judged to be restricted to dermis, amenable to immediate/ad hoc incision) or wound infection] and deep-seated infections [dSSTI; e.g. subcutaneous abscess (involving deep subcutaneous tissue, incision preferentially by surgically experienced physician), pyomyositis and necrotising fasciitis] [3]. The management of patients was based on the physician’s judgement, and no guidance was provided by the investigators.
The empirical antimicrobial therapy was judged adequate if the causative S. aureus isolate was tested susceptible to the respective antimicrobial compound; intermediate results were treated as resistant. Two investigators (SR, FS) did the stratification into ‘adequate’ and ‘inadequate’ therapy independently. Discordant results were resolved during telephone conferences. Aminoglycosides were only considered adequate if given in combination with a susceptible tested second drug.
Bacterial isolates
Clinical specimen were cultured on Columbia blood agar and species identification was done by Gram staining, a positive catalase and coagulase test. Species was confirmed as S. aureus for all isolates in Germany by MALDI-TOF (BRUKER Daltonics GmbH, Bremen, Germany). Susceptibility testing was done at each study site according to Clinical Laboratory Standards Institute guidelines to guarantee prompt reporting of antimicrobial susceptibility results to the clinician [16]. Non-susceptibility rates include resistant and intermediate isolates. Determinants for species confirmation (nuc, coa), multilocus sequence types (MLST) and selected virulence factors (lukS-PV/lukF-PV, hlb) were extracted from already available whole genome sequences (accession numbers of the European Nucleotide Archive (https://www.ebi.ac.uk/ena: PRJEB15192, PRJEB11627, PRJEB14816) [12, 17, 18]. Other virulence factors associated with SSTI (HLA, PSM) were not included in the analysis as they belong to the core genome [4]. Since they were present in almost all isolates investigated, the sole presence of the gene is not suitable to assess strain-specific virulence. A minimum-spanning tree was constructed based on the allelic profiles of the MLST scheme to assess the clonal structure of isolates from both sSSTI and dSSTI (SeqSphere+ software, version 2.4.0, Ridom GmbH, Münster, Germany). MLST STs were grouped into clonal complexes (CC) if they shared at least six out of seven alleles using eBURST (http://eburst.mlst.net/). The association with CCs was based on the dataset of the S. aureus MLST database (https://pubmlst.org/saureus/, accessed 2 November 2017).
Statistical analysis
Medians (ranges) of non-normally distributed data (i.e. age) were compared between sSSTI and dSSTI using the Wilcoxon rank sum test with continuity correction. We used the Kruskal–Wallis test to compare the median age between the four study sites. The Fisher’s exact test or Chi2-test was used where appropriate to assess an association between categorical variables and to calculate the odds ratio (OR) and its 95% confidence interval (95% CI). The association of MLST CCs with SSTI was corrected for multiple testing (Hommel p value adjustment). The management of superficial versus deep-seated SSTI (i.e. selection of antimicrobial therapies, antimicrobial treatment ± I&D) was assessed by logistic regression. Significance level was set at 0.05. Analyses were done with “R” (package “epiDisplay”).
Results
In total, 319 patients were recruited at the four study sites in DR Congo (n = 56, 17.6%), Gabon (n = 89, 27.9%), Mozambique (n = 79, 24.8%) and Tanzania (n = 95, 29.8%) and included in the final analysis.
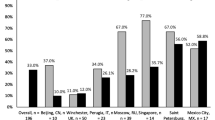
The majority of the patients (n = 220; 69%) presented with an sSSTI. A dSSTI was diagnosed in 99 patients (31%) with abscesses (n = 89) representing the predominant entity, followed by pyomyositis (n = 4) and others (n = 4). All SSTI were S. aureus monomicrobial infections. Species of all isolates was confirmed by MALDI-TOF and the detection of nuc and coa. The antimicrobial non-susceptibility rates were similar among isolates from sSSTI to dSSTI (Fig. 1). High non-susceptibility rates (sSSTI/dSSTI) were detected against penicillin (95.9/99.0%), followed by tetracycline (55.8/48.5%) and trimethoprim-sulfamethoxazole (30.9/32.3%, Fig. 1).
The proportion of females (34.7–53.9%, p = 0.075) and sSSTI (59.9–75.3%, p = 0.141) and the distribution of median age (1–26, p = 0.098) were comparable between each study site.
Patients with dSSTI were older (median age 6 vs. 3 years, p = 0.002), more likely HIV-positive (15.9 vs. 7.6%, p = 0.11), were more often admitted to the hospital (23.5 vs. 13.2%, p = 0.03) and underwent I&D more often (76.5 vs. 45.5%, p = 0.04) compared to patients with sSSTI (Table 1). Taken all SSTI together, 93.4% (n = 297) of the patients received a treatment consisting of either antimicrobials alone (38.4%, n = 122), I&D alone (8.8%, n = 28) or antimicrobials plus I&D (n = 46.2%, n = 147) on Day 1 (Table 1).
The most common antimicrobial agents (daily dosage range, application) were flucloxacillin (0.25–1.5 g, po), cloxacillin (0.125–1.5 g, po), oxacillin (0.125 g, po), ampicillin (0.075–3 g, iv), amoxicillin (0.009–1.5 g, po) and erythromycin (0.125–1 g, po, Table 2). In total, 8.6% (n = 19, sSSTI) and 11.1% (n = 11, dSSTI) of the patients received gentamicin as a combination drug.
There was no statistically significant difference in the selection of antimicrobial agents for the treatment of superficial versus deep-seated infections (Table 2). However, anti-staphylococcal penicillins were more frequently used for the treatment of sSSTI compared to dSSTI (day 1: 31.4 vs. 18.2%; day 3: 21.8 vs. 14.1%). In contrast, (amino-)penicillins were less frequently used in sSSTI compared to dSSTI (day 1: 21.8 vs. 30.3%; day 3: 15.0 vs. 27.1%, Table 2).
Patients with deep-seated infection received less likely an adequate antimicrobial therapy both on day 1 as an empirical therapy (55.4 vs. 70.7%, p = 0.049) and on day 3 (58.9 vs. 72.4%, p = 0.04). Importantly, the four study sites were heterogeneous in selecting antimicrobial agents: the proportion of an adequate therapy ranged between 37.2–90% (day 1) and 34.6–89.9% (day 3).
In total, antimicrobial therapy was adapted in 25.5% (56/220) and 9.1% (9/99) of patients with sSSTI and dSSTI, respectively, when the antimicrobial susceptibility results were available. In some cases, an inadequate therapy was stopped or switched to an adequate therapy (Table 3). An adequate therapy was discontinued in 26 patients of whom the majority underwent I&D (n = 21) yielding to clinical improvement. In five cases, the antimicrobial therapy was switched to a compound that was not tested susceptible, for unknown reasons.
In total, 21 patients with a MRSA SSTI (6.5%) were detected with similar proportions in sSSTI (6.8%, n = 15) and dSSTI (6.1%, n = 6). Of these, two patients received an adequate antimicrobial therapy with clindamycin on day 1. On day 3, four additional patients were treated with chloramphenicol, which was tested susceptible.
In a next step, we assessed the impact of PVL and HLB on SSTIs, as both were shown to be associated with SSTI in Africa [12]. PVL, but not HLB, was associated with dSSTI (Table 1). A surgical intervention (I&D) was more frequently done if the SSTI was caused by a PVL-positive isolate compared to infections with a PVL-negative isolate (59.8 vs. 19.2%, OR = 1.7, 95% CI 1.1–2.7, p = 0.02). In contrast, PVL was not associated with hospital admission (OR = 0.7, 95% CI 0.4–1.4, p = 0.33). PVL-positive isolates (n = 205) mainly belonged to ST152 (n = 68), ST121 (n = 43), ST2430 (n = 25) and others (n = 69). The majority of isolates (PVL-positive and -negative) belonged to MLST clonal complexes CC5 (n = 140, 43.9%), CC121 (n = 74, 23.2%), CC152 (n = 68, 21.3%), CC88 (n = 12, 3.8%), CC80 (n = 8, 2.5%) and others (n = 17, 5.3%, Fig. 2). Compared to dSSTI, sSSTI was more likely caused by isolates belonging to CC5 (48.6 vs. 33.3%, OR = 1.9, 95% CI 1.2–3.1, Hommel adjusted p = 0.08) and CC152 (23.6 vs. 16.2%, OR = 1.6, 95% CI 0.9–3.0, Hommel adjusted p = 0.66). In contrast, CC121 was more common in deep-seated compared to superficial SSTI (36.4 vs. 17.3%, OR = 2.7, 95% CI 1.6–4.8, Hommel adjusted p < 0.001).
Population structure of Staphylococcus aureus from superficial and deep-seated skin and soft tissue infections. A minimum spanning-tree was constructed using the allelic profile of the multilocus sequence typing (MLST) scheme. The labels of the nodes represent the MLST sequence types. The size of the node corresponds to the number of isolates. The distance between the nodes is shown as the number of differing alleles. The major clonal complexes (CCs) are encircled in dashed lines
The assessment of the infrastructure for the management of SSTI revealed that all study sites have access to the majority of antimicrobial agents that can be used for S. aureus SSTI (Table 4). However, anti-staphylococcal penicillins or first-generation cephalosporins are available only at three sites. Given the high rates of resistance to tetracycline and trimethoprim-sulfamethoxazole, the major challenge is the availability of MRSA-directed therapies (i.e. glycopeptides, linezolid, daptomycin) for severe infections. At three study sites, the patients cover the treatment costs. If patients have a health insurance, this will cover 75–100% of expenses in Gabon. Amoxicillin/clavulanic acid is the most expensive agent in all countries, but cloxacillin could be a cheaper and S. aureus specific alternative. Three laboratories return the susceptibility test results within three days to the clinician while ≤ 40% of patients with SSTI are generally scheduled for a follow-up visit. A surgical service for I&D is either available on site (n = 3) or at a referral center (Table 4). The number of blood cultures per admission was very low at three study sites (0–0.108 blood cultures per admission) except for one site (0.8 blood cultures per admission, Table 4).
Discussion
We assessed the clinical management of S. aureus SSTI in four sub-Saharan countries, and found that the necessary treatment infrastructure (i.e. surgery, antimicrobial agents) was available for, and applied to the majority of patients. The microbiological test results had limited impact on the management of SSTI.
In our study, sSSTI was more common than dSSTI, which is in line with a European multi-center study on S. aureus SSTI in returning travelers (sSSTI: 56.6%, dSSTI: 43.4%) [11]. Of note, the majority of travelers in this study returned from sub-Saharan Africa (33%), where they most likely acquired the causative S. aureus strain. The antimicrobial resistance rates were comparable to those of isolates from both sSSTI- and dSSTI from our study (Fig. 1) [11]. In general, high resistance rates to penicillin (73.7–100%), tetracycline (21.8–92%) and trimethoprim/sulfamethoxazole (4–89.1%) are widespread in sub-Saharan Africa most likely due to the frequent use of trimethoprim/sulfamethoxazole in particular for the treatment and prevention of infections (e.g. in HIV-positive patients) [8, 19, 20]. This has to be considered in empirical therapies.
The higher proportion of sSSTI compared to dSSTI in our study (69 vs. 31%) is also in line with a large study from Japan (superficial SSTI: 63.6%, deep-seated SSTI: 36.4%) [21]. In addition, the lower median age in patients with sSSTI compared to dSSTI is in accordance with results from a study from China [22]. Here, impetigo was more common in children than in adults (83.5 vs. 7.5%), while abscesses, folliculitis and furuncle, which tend to develop to deep-seated SSTI more likely, were less frequent in children than in adults (3.9 vs. 8.9%) [22].
In total, 85.9% (85/99) of patients with dSSTI received an antimicrobial therapy, which was inadequate in almost one-half of the cases (Table 1). This suggests a poor strategy to select the right empirical therapy at least in dSSTI. The guidelines of the Infectious Diseases Society of America (IDSA) suggest trimethoprim/sulfamethoxazole or doxycycline (moderate purulent disease) or an MRSA-directed therapy in severe disease (e.g. vancomycin, daptomycin, linezolid) [3]. However, the IDSA guideline is not applicable to most sub-Saharan African settings, as resistance rates against tetracycline (48.5–55.8%) and trimethoprim/sulfamethoxazole (30.8–32.3%) are too high (Fig. 1), whilst the prevalence of MRSA is too low (6.9%) to be considered in the empirical treatment. Therefore, there is a need for continuous antimicrobial resistance surveillance to develop guidelines tailored to regional resistance patterns in Africa. Numerous studies on antimicrobial resistance are already available, but the quality of data is usually insufficient due to missing harmonization between laboratories and poor performance in species identification and susceptibility testing [23, 24].
Noteworthy, the proportion of an adequate antimicrobial therapy increased only by 1.7–3.5% on day 3, when the susceptibility reports are usually available (Table 1). Apparently, microbiological diagnostics had limited impact on the management of SSTI in our study. This can be due to the pre-analytical (e.g. selection of the specimen, storage and transport condition), analytical (e.g. timeliness in reporting results to the physician) or the post-analytical processes (e.g. laboratory software, prescribing habits of the physician, unavailability of antimicrobials, unawareness of susceptibility results, loss to follow-up of the patients). In 26 patients, an adequate therapy was stopped on day 3 (Table 4). This was most likely due to a rapid clinical improvement since the majority of these patients underwent I&D. However, to improve the switch to an adequate definitive therapy after receiving the laboratory reports, joint training and improved communication between microbiologists and physicians should be considered to increase the value of the privilege of a microbiological laboratory in resource-limited settings [25]. Accordingly, the low numbers of blood cultures sampled documents underutilization of microbiological facilities (Table 4). The implementation of antibiotic stewardship programs could support the appropriate use of antimicrobial agents, also in low- and middle-income countries if widespread challenges (e.g. laboratory infrastructure, access to quality antimicrobials, knowledge and awareness of the providers) are adequately addressed [26]. An exchange of perceptions and attitudes might also be constructive, particularly in South–South cooperation. As shown in our study, one site performed very well in the selection of empirical therapies and others might benefit from this knowledge.
More than one-half of the patients underwent I&D; the proportion was even higher in patients with d SSTI (76.8%, Table 1). I&D was frequently combined with a systemic antimicrobial therapy (37.7–64.7%), which is usually not recommended in simple abscesses. Notwithstanding, these data are comparable to a study from a tertiary care hospital in the USA; after the implementation of an abscess treatment algorithm, 48% of pediatric patients underwent I&D; of these, 75% received an additional antimicrobial therapy after I&D [27].
There is now convincing evidence that abscesses/furuncles are associated with PVL, although the exact pathophysiological mechanisms remains controversial [5]. Since the majority of deep-seated infections in our study were abscesses (89.9%), the clear association of PVL with deep-seated SSTI fits well into the current concept (Table 1). PVL was a risk factor for surgical intervention in our study (Table 1). This association was also shown in travelers with SSTI. In contrast to our study, travelers with PVL-positive S. aureus infection were more frequently admitted compared to patients with a PVL-negative SSTI [11].
Our study has several limitations: First, the significance of the results is limited by a high level of missing values that reaches up to almost 50% for some items (e.g. HIV status, 14-day mortality, Table 1). In part, this is due to a high proportion of patients with (minor) superficial skin infections who were not admitted to the hospital and were lost to follow-up. In addition, many participants might not have known their HIV-status in the absence of forceful test-and-treat policies. Second, the four study sites are part of the international StaphNet research cooperation receiving training, capacity building and external quality assessment which is known to improve laboratory performance [25]. Therefore, they might not be representative for sub-Saharan Africa. Third, pediatric patients are overrepresented in the cohort; thus, generalizability of some aspects (e.g. SSTI presentation, selection of antimicrobial agents) to adult populations may be impeded. Fourth, the vast majority of SSTI were minor infections since no septic shock or death was recorded. Our population, therefore, does not represent the whole spectrum of SSTI including severe infections.
Conclusions
A sufficient infrastructure was available for the majority of patients to access antimicrobials and I&D. There is a need for continuous local antimicrobial resistance surveillance to provide guidance for empirical antimicrobial therapies. This could be flanked by joint trainings of clinicians and lab personnel including the implementation of antibiotic stewardship programs. These steps are crucial to make the most of the valuable resource of a microbiology laboratory to improve patient’s care in resource-limited settings.
References
Tong SYC, Davis JS, Eichenberger E, Holland TL, Fowler VG. Staphylococcus aureus infections: epidemiology, pathophysiology, clinical manifestations, and management. Clin Microbiol Rev. 2015;28:603–61. https://doi.org/10.1128/cmr.00134-14.
Hersh AL, Chambers HF, Maselli JH, Gonzales R. National trends in ambulatory visits and antibiotic prescribing for skin and soft-tissue infections. Arch Intern Med. 2008;168:1585–91. https://doi.org/10.1001/archinte.168.14.1585.
Stevens DL, Bisno AL, Chambers HF, Dellinger EP, Goldstein EJ, Gorbach SL, et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin Infect Dis. 2014;59:e10–52. https://doi.org/10.1093/cid/ciu444.
Otto M. Phenol-soluble modulins. Int J Med Microbiol. 2014;304:164–9. https://doi.org/10.1016/j.ijmm.2013.11.019.
Shallcross LJ, Fragaszy E, Johnson AM, Hayward AC. The role of the Panton-Valentine leucocidin toxin in staphylococcal disease: a systematic review and meta-analysis. Lancet Infect Dis. 2013;13:43–54. https://doi.org/10.1016/S1473-3099(12)70238-4.
Ruffing U, Alabi A, Kazimoto T, Vubil DC, Akulenko R, Abdulla S, et al. Community-associated Staphylococcus aureus from Sub-Saharan Africa and Germany: a cross-sectional geographic correlation study. Sci Rep. 2017;7:154. https://doi.org/10.1038/s41598-017-00214-8.
Horner C, Utsi L, Coole L, Denton M. Epidemiology and microbiological characterization of clinical isolates of Staphylococcus aureus in a single healthcare region of the UK, 2015. Epidemiol Infect. 2017;145:386–96. https://doi.org/10.1017/s0950268816002387.
Schaumburg F, Alabi AS, Peters G, Becker K. New epidemiology of Staphylococcus aureus infection in Africa. Clin Microbiol Infect. 2014;20:589–96. https://doi.org/10.1111/1469-0691.12690.
Schaumburg F, Alabi AS, Mombo-Ngoma G, Kaba H, Zoleko RM, Diop DA, et al. Transmission of Staphylococcus aureus between mothers and infants in an African setting. Clin Microbiol Infect. 2014;20:O390–6. https://doi.org/10.1111/1469-0691.12417.
Gutierrez K, Halpern MS, Sarnquist C, Soni S, Arroyo AC, Maldonado Y. Staphylococcal infections in children, California, USA, 1985–2009. Emerg Infect Dis. 2013;19:10–20. https://doi.org/10.3201/eid1901.111740 (quiz 185).
Nurjadi D, Friedrich-Jänicke B, Schäfer J, Van Genderen PJJ, Goorhuis A, Perignon A, et al. Skin and soft tissue infections in intercontinental travellers and the import of multi-resistant Staphylococcus aureus to Europe. Clin Microbiol Infect. 2015;21:e1–10. https://doi.org/10.1016/j.cmi.2015.01.016.
Lebughe M, Phaku P, Niemann S, Mumba D, Peters G, Muyembe-Tamfum J-J et al. The impact of the Staphylococcus aureus virulome on infection in a developing country: a cohort study. Front Microbiol. 2017;8. https://doi.org/10.3389/fmicb.2017.01662.
Li T, Yu X, Xie J, Xu Y, Shang Y, Liu Y, et al. Carriage of virulence factors and molecular characteristics of Staphylococcus aureus isolates associated with bloodstream, and skin and soft tissue infections in children. Epidemiol Infect. 2013;141:2158–62. https://doi.org/10.1017/s0950268812002919.
Herrmann M, Abdullah S, Alabi A, Alonso P, Friedrich AW, Fuhr G, et al. Staphylococcal disease in Africa: another neglected ‘tropical’ disease. Future Microbiol. 2013;8:17–26. https://doi.org/10.2217/fmb.12.126.
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Crit Care Med. 2003;31:1250–6. https://doi.org/10.1097/01.ccm.0000050454.01978.3b.
Institute Clinical Laboratory Standards. Performance standards for antimicrobial susceptibility testing. 27th ed. Wayne: CLSI; 2017.
Strauss L, Ruffing U, Abdulla S, Alabi A, Akulenko R, Garrine M, et al. Detecting Staphylococcus aureus virulence and resistance genes: a comparison of whole-genome sequencing and DNA microarray technology. J Clin Microbiol. 2016;54:1008–16. https://doi.org/10.1128/JCM.03022-15.
Strauss L, Stegger M, Akpaka PE, Alabi A, Breurec S, Coombs G, et al. Origin, evolution, and global transmission of community-acquired Staphylococcus aureus ST8. Proc Natl Acad Sci USA. 2017. https://doi.org/10.1073/pnas.1702472114.
Egyir B, Guardabassi L, Sorum M, Nielsen SS, Kolekang A, Frimpong E, et al. Molecular epidemiology and antimicrobial susceptibility of clinical Staphylococcus aureus from healthcare institutions in Ghana. PLOS One. 2014;9:e89716. https://doi.org/10.1371/journal.pone.0089716.
Nurjadi D, Olalekan AO, Layer F, Shittu AO, Alabi A, Ghebremedhin B, et al. Emergence of trimethoprim resistance gene dfrG in Staphylococcus aureus causing human infection and colonization in sub-Saharan Africa and its import to Europe. J Antimicrob Chemother. 2014;69:2361–8. https://doi.org/10.1093/jac/dku174.
Watanabe S, Ohnishi T, Yuasa A, Kiyota H, Iwata S, Kaku M, et al. The first nationwide surveillance of antibacterial susceptibility patterns of pathogens isolated from skin and soft-tissue infections in dermatology departments in Japan. J Infect Chemother. 2017;23:503–11. https://doi.org/10.1016/j.jiac.2017.05.006.
Liu Y, Xu Z, Yang Z, Sun J, Ma L. Characterization of community-associated Staphylococcus aureus from skin and soft-tissue infections: a multicenter study in China. Emerg Microbes Infect. 2016;5:e127. https://doi.org/10.1038/emi.2016.128.
Tadesse BT, Ashley EA, Ongarello S, Havumaki J, Wijegoonewardena M, Gonzalez IJ, et al. Antimicrobial resistance in Africa: a systematic review. BMC Infect Dis. 2017;17:616. https://doi.org/10.1186/s12879-017-2713-1.
Frean J, Perovic O, Fensham V, McCarthy K, von Gottberg A, de Gouveia L, et al. External quality assessment of national public health laboratories in Africa, 2002-2009. Bull World Health Organ. 2012;90:191–9. https://doi.org/10.2471/blt.11.091876.
Barbé B, Yansouni CP, Affolabi D, Jacobs J. Implementation of quality management for clinical bacteriology in low-resource settings. Clin Microbiol Infect. 2017;23:426–33. https://doi.org/10.1016/j.cmi.2017.05.007.
Cox JA, Vlieghe E, Mendelson M, Wertheim H, Ndegwa L, Villegas MV, et al. Antibiotic stewardship in low- and middle-income countries: the same but different? Clin Microbiol Infect. 2017;23:812–8. https://doi.org/10.1016/j.cmi.2017.07.010.
Nelson CE, Chen A, McAndrew L, Tay KY, Balamuth F. Management of skin and soft-tissue infections before and after clinical pathway implementation. Clin Pediatr (Phila). 2017:9922817738329. https://doi.org/10.1177/0009922817738329.
Acknowledgements
This study received grants from the Deutsche Forschungsgemeinschaft (HE 1850/11-1 to M.H., KE 700/3-1 to W.V.K., ME 3205/4-1 to A.M., and PE 296/6-1 to G.P.).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Alabi, A., Kazimoto, T., Lebughe, M. et al. Management of superficial and deep-seated Staphylococcus aureus skin and soft tissue infections in sub-Saharan Africa: a post hoc analysis of the StaphNet cohort. Infection 46, 395–404 (2018). https://doi.org/10.1007/s15010-018-1140-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-018-1140-6