Abstract
Objective
The objective of the study was to evaluate the efficacy and tolerability of trimethoprim–sulfamethoxazole (also known as co-trimoxazole, TMPS) to treat Klebsiella pneumoniae (Kp)-K. pneumoniae carbapenemase (KPC) infections.
Methods
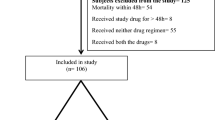
Clinical data of patients with a TMPS-susceptible Kp-KPC infection were collected as a case series.
Results
We report clinical outcomes and tolerability for 14 patients infected by Kp-KPC strains susceptible to TMPS, including three bloodstream infections. In ten cases (71.4%), TMPS was administered as monotherapy. In all but one case, Kp-KPC infection was cured. In the remaining patient, therapy was discontinued because of an adverse event.
Conclusions
The use of TMPS to treat TMPS-susceptible Kp-KPC infections seems promising.
Similar content being viewed by others
References
European Antimicrobial Resistance Surveillance Network (EARS-Net). http://ecdc.europa.eu/en/healthtopics/antimicrobial_resistance/database/Pages/table_reports.aspx. Accessed Nov 2016.
Maltezou HC, Giakkoupi P, Maragos A, et al. Outbreak of infections due to KPC-2-producing Klebsiella pneumoniae in a hospital in Crete (Greece). J Infect. 2009;58:213–9.
Souli M, Galani I, Antoniadou A, et al. An outbreak of infection due to beta-Lactamase Klebsiella pneumoniae Carbapenemase 2-producing K. pneumoniae in a Greek University Hospital: molecular characterization, epidemiology, and outcomes. Clin Infect Dis. 2010;50:364–73.
Grundmann H, Livermore DM, Giske CG, et al. Carbapenem-non-susceptible Enterobacteriaceae in Europe: conclusions from a meeting of national experts. Euro Surveill 2010;15.
Freire MP, Abdala E, Moura ML, et al. Risk factors and outcome of infections with Klebsiella pneumoniae carbapenemase-producing K. pneumoniae in kidney transplant recipients. Infection. 2015;43:315–23.
Tumbarello M, Trecarichi EM, De Rosa FG, et al. Infections caused by KPC-producing Klebsiella pneumoniae: differences in therapy and mortality in a multicentre study. J Antimicrob Chemother. 2015;70:2133–43.
Daikos GL, Tsaousi S, Tzouvelekis LS, et al. Carbapenemase-producing Klebsiella pneumoniae bloodstream infections: lowering mortality by antibiotic combination schemes and the role of carbapenems. Antimicrob Agents Chemother. 2014;58:2322–8.
Qureshi ZA, Paterson DL, Potoski BA, et al. Treatment outcome of bacteremia due to KPC-producing Klebsiella pneumoniae: superiority of combination antimicrobial regimens. Antimicrob Agents Chemother. 2012;56:2108–13.
van der Donk CF, Beisser PS, Hoogkamp-Korstanje JA, Bruggeman CA, Stobberingh EE, Antibiotic Resistance Surveillance Group. A 12 year (1998-2009) antibiotic resistance surveillance of Klebsiella pneumoniae collected from intensive care and urology patients in 14 Dutch hospitals. J Antimicrob Chemother. 2011;66:855–8.
Lombardi F, Gaia P, Valaperta R, et al. Emergence of Carbapenem-Resistant Klebsiella pneumoniae: progressive spread and four-year period of observation in a cardiac surgery division. Biomed Res Int. 2015;2015:871947.
Oteo J, Ortega A, Bartolomé R, et al. Prospective multicenter study of carbapenemase-producing Enterobacteriaceae from 83 hospitals in Spain reveals high in vitro susceptibility to colistin and meropenem. Antimicrob Agents Chemother. 2015;59:3406–12.
Bremmer DN, Clancy CJ, Press EG, et al. KPC-producing Klebsiella pneumoniae strains that harbor AAC(6′)-Ib exhibit intermediate resistance to amikacin. Antimicrob Agents Chemother. 2014;58:7597–600.
Walsh TR, Toleman MA, Poirel L, et al. Metallo-b-lactamases: the quiet before the storm? Clin Microbiol Rev. 2005;18:306–25.
Sievert DM, Ricks P, Edwards JR, et al. Antimicrobial-resistant pathogens associated with healthcare-associated infections: summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2009–2010. Infect Control Hosp Epidemiol. 2013;34:1–14.
Giani T, Pini B, Arena F, et al. Epidemic diffusion of KPC carbapenemase-producing Klebsiella pneumoniae in Italy: results of the first countrywide survey, 15 May to 30 June 2011. Euro Surveill 2013;18:20849.
ECDC. Annual epidemiological report 2013: reporting on 2011 surveillance data and 2012 epidemic intelligence data. Stockholm: European Centre for Disease Prevention and Control; 2013. http://ecdc.europa.eu/en/publications/Publications/annual-epidemiological-report-2013.pdf.. Accessed Jan 2017.
Falagas ME, Rafailidis PI. Nephrotoxicity of colistin: new insight into an old antibiotic. Clin Infect Dis. 2009;48:1729–31.
Monaco M, Giani T, Raffone M, et al. Colistin resistance superimposed to endemic carbapenem-resistant Klebsiella pneumoniae: a rapidly evolving problem in Italy, November 2013 to April 2014. Euro Surveill. 2014;23:19.
Kontopidou F, Giamarellou H, Katerelos P, et al. Infections caused by carbapenem-resistant Klebsiella pneumoniae among patients in intensive care units in Greece: a multi-centre study on clinical outcome and therapeutic options. Clin Microbiol Infect. 2014;20:O117–23.
Neuner EA, Yeh JY, Hall GS, et al. Treatment and outcomes in carbapenem-resistant Klebsiella pneumoniae bloodstream infections. Diagn Microbiol Infect Dis. 2011;69:357–62.
Freire AT, Melnyk V, Kim MJ, et al. Comparison of tigecycline with imipenem/cilastatin for the treatment of hospital-acquired pneumonia. Diagn Microbiol Infect Dis. 2010;68:140–51.
Akova M, Daikos GL, Tzouvelekis L, Carmeli Y. Interventional strategies and current clinical experience with carbapenemase-producing Gram-negative bacteria. Clin Microbiol Infect. 2012;18:439–48.
Tumbarello M, Viale P, Viscoli C, et al. Predictors of mortality in bloodstream infections caused by Klebsiella pneumoniae carbapenemase-producing K. pneumoniae: importance of combination therapy. Clin Infect Dis. 2012;55:943–50.
Ji S, Lv F, Du X, et al. Cefepime combined with amoxicillin/clavulanic acid: a new choice for the KPC-producing Klebsiella pneumoniae infection. Int J Infect Dis. 2015;38:108–14.
Limbago BM, Rasheed JK, Anderson KF, et al. IMP-producing carbapenem-resistant Klebsiella pneumoniae in the US. J Clin Microbiol. 2011;49:4239–45.
Ahn C, Syed A, Hu F, O’Hara JA, Rivera JI, Doi Y. Microbiological features of KPC-producing enterobacter isolates identified in a US hospital system. Diagn Microbiol Infect Dis. 2014;80:154–8.
Acknowledgements
We are grateful to Leonida Passeri for his technical assistance in data management.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Funding
No funding has been received for this study. The present manuscript was revised by San Francisco Edit, which was supported by internal funding. The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Rights and permissions
About this article
Cite this article
Murri, R., Fiori, B., Spanu, T. et al. Trimethoprim–sulfamethoxazole therapy for patients with carbapenemase-producing Klebsiella pneumoniae infections: retrospective single-center case series. Infection 45, 209–213 (2017). https://doi.org/10.1007/s15010-016-0968-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-016-0968-x