Abstract
Background
Current political crises in the Middle East and economic discrepancies led millions of people to leave their home countries and to flee to Western Europe. This development raises unexpected challenges for receiving health care systems. Although pan-European initiatives strive for updated and optimized vaccination strategies, little data on immunity against vaccine-preventable diseases in the current refugee population exist.
Methods
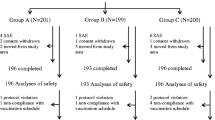
We quantified serum IgG against tetanus and diphtheria (TD) in n = 678 refugees currently seeking shelter in six German refugee centers.
Findings
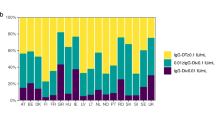
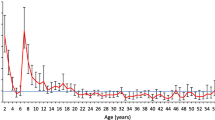
Reflecting current migration statistics in Europe, the median age within the cohort was 26 years, with only 23.9 % of female subjects. Insufficient IgG levels without long-term protection against tetanus were found in 56.3 % of all refugees. 76.1 % of refugees had no long-term protection against diphtheria. 47.7 % of subjects needed immediate vaccination against tetanus, and 47.7 % against diphtheria. For both diseases, an age-dependent decline in protective immunity occurred.
Interpretation
We observed a considerably low rate of tetanus-protected refugees, and the frequency of diphtheria-immune refugees was far from sufficient to provide herd immunity. These findings strongly support recent intentions to implement and enforce stringent guidelines for refugee vaccination in the current crisis.




Similar content being viewed by others
Abbreviations
- EU:
-
European Union
- IgG:
-
Immunoglobulin G
- TD:
-
Tetanus, diphtheria
- VPD:
-
Vaccine-preventable diseases
- WHO:
-
World Health Organization
- UNHCR:
-
United Nations High Commissioner for Refugees
- UNICEF:
-
United Nations Children’s Fund
References
Takla A, Barth A, Siedler A, Stöcker P, Wichmann O, Deleré Y. Measles outbreak in an asylum-seekers’ shelter in Germany: comparison of the implemented with a hypothetical containment strategy. Epidemiol Infect (Cambridge University Press). 2012;140:1589–98.
Kouadio IK, Koffi AK, Attoh-Toure H, Kamigaki T, Oshitani H. Outbreak of measles and rubella in refugee transit camps. Epidemiol Infect. 2009;137:1593.
Heudtlass P, Speybroeck N, Guha-Sapir D. Monitoring mortality in forced migrants—can bayesian methods help us to do better with the (little) data we have? PLoS Med. 2015;12:e1001887. doi:10.1371/journal.pmed.1001887.
Jakab Z. Population movement is a challenge for refugees and migrants as well as for the receiving population [Internet]. 2015. http://www.euro.who.int/en/health-topics/health-determinants/migration-and-health/news/news/2015/09/population-movement-is-a-challenge-for-refugees-and-migrants-as-well-as-for-the-receiving-population. Accessed 23 May 2016.
WHO, UNHCR, UNICEF. Joint technical guidance: general principles of vaccination of refugees, asylum-seekers and migrants in the WHO European Region. 2015.
Robert-Koch-Institut. Konzept zur Umsetzung frühzeitiger Impfungen bei Asylsuchenden nach Ankunft in Deutschland. Epidemiol Bull. 2015;41:439–44.
Grote U, Wildenau G, Behrens G, Jablonka A. Primary care for refugees in Germany—first data on demographics and reasons for treatment after the establishment of basic health care in refugee camps. Primärärztliche Versorgung von Flüchtlingen in Deutschland. Erste Daten zu Demographie und Behandlu. Anasthesiol Intensivmed. 2015;56:654–60.
Jablonka A, Happle C, Grote U, Schleenvoigt B, Hampel A, Schmidt RE, et al. Measles, mumps, rubella and varicella seroprevalence in refugees in Germany in 2015. Infection. 2016;. doi:10.1007/s15010-016-0926-7.
Hampel A, Solbach P, Cornberg M, Schmidt RE, Behrens GMN, Jablonka A. Current seroprevalence, vaccination and predictive value of liver enzymes for hepatitis B among refugees in Germany. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2016;59:578–83.
Jablonka A, Solbach P, Ringe B, Schleenvoigt B, Dopfer C, Hampel A, et al. Niedrige Seroprävalenz von Hepatitis C bei Flüchtlingen in Deutschland im Jahr 2015. Notfall- und Rettungsmedizin. 2016;. doi:10.1007/s10049-016-0198-x.
Jablonka A, Solbach P, Nothdorft S, Hampel A, Schmidt RE, Behrens GMN. Niedrige Seroprävalenz von Syphilis und HIV bei Flüchtlingen in Deutschland. Dtsch Medizinische Wochenschrift. 1007;2016:141.
Eurostat. Asylum statistics [Internet]. Eurostat. 2015. http://ec.europa.eu/eurostat/statistics-explained/index.php/Asylum_statistics#Asylum_applicants. Accessed 14 June 2016.
Zielinski A, Rudowska J. Tetanus in Poland in 2011. Przegl Epidemiol. 2013;67:253–8.
Filia A, Bella A, von Hunolstein C, Pinto A, Alfarone G, Declich S, et al. Tetanus in Italy 2001-2010: a continuing threat in older adults. Vaccine. 2014;32:639–44.
Centers for Disease Control and Prevention (CDC). Tetanus surveillance—United States, 2001–2008. MMWR Morb Mortal Wkly Rep. 2011;60:365–9.
Quinn HE, McIntyre PB. Tetanus in the elderly—an important preventable disease in Australia. Vaccine. 2007;25:1304–9.
World Health Organization. Factsheet tetanus [Internet]. 2015. http://www.wpro.who.int/mediacentre/factsheets/fs_20120307_tetanus/en. Accessed 25 Apr 2016.
World Health Organization. Diphtheria-tetanus-pertussis (DTP3) immunization coverage [Internet]. 2014. http://www.who.int/gho/immunization/dtp3/en/. Accessed 25 Apr 2016.
Poethko-Müller C, Schmitz R. Vaccination coverage in German adults: results of the German health interview and examination survey for adults (DEGS1). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2013;56:845–57.
Bödeker B, Remschmidt C, Müters S, Wichmann O. Influenza, tetanus, and pertussis vaccination coverage among adults in Germany. Bundesgesundheitsblatt. Gesundheitsforschung. Gesundheitsschutz. 2015;58:174–81.
Dittmann S, Wharton M, Vitek C, Ciotti M, Galazka A, Guichard S, et al. Successful control of epidemic diphtheria in the states of the Former Union of Soviet Socialist Republics: lessons learned. J Infect Dis. 2000;181:S10–22.
di Giovine P, Kafatos G, Nardone A, Andrews N, Ölander RM, Alfarone G, et al. Comparative seroepidemiology of diphtheria in six European countries and Israel. Epidemiol Infect. 2013;141:132–42.
European Centre for Disease Prevention and Control. Cutaneous diphtheria among recently arrived refugees and asylum seekers in the EU, 30 July 2015. Stockholm: ECDC; 2015.
Sadoh AE, Oladokun RE. Re-emergence of diphtheria and pertussis: implications for Nigeria. Vaccine. 2012;30:7221–8.
STIKO. Empfehlungen der Ständischen Impfkommission (STIKO) am RKI-Stand: August 2015. Epidemiol Bull. 2015;2015:105–14.
Begg N (WHO). Manual for the management and control of diphtheria in the European region. Copenhagen: WHO Regional Office for Europe;1994.
Robert-Koch-Institut. Konzept zur Umsetzung frühzeitiger Impfungen bei Asylsuchenden nach Ankunft in Deutschland. Epidemiol Bull. 2015;41:439–48.
Robert-Koch-Institut. Dem Robert Koch-Institut übermittelte meldepflichtige Infektionskrankheiten bei Asylsuchenden in Deutschland [Internet]. 2015. http://www.rki.de/DE/Content/Gesundheitsmonitoring/Gesundheitsberichterstattung/GesundAZ/Content/A/Asylsuchende/Inhalt/meldepflichtige_Infektionskrankheiten_bei_Asylsuchendenpdf?__blob=publicationFile. Accessed 25 Apr 2016.
Nicolai T, Fuchs O, von Mutius E. Caring for the Wave of Refugees in Munich. N Engl J Med. 2015;373:1593–5.
Bozorgmehr K, Razum O. EU’s external borders: what is the role for global health law. Lancet (London, England). 2015;385:2147.
Steel Z, Liddell BJ, Bateman-Steel CR, Zwi AB. Global protection and the health impact of migration interception. PLoS Med. 2011;8:e1001038.
Acknowledgments
The authors would like to thank all doctors and medical personnel involved in medical care of the refugees for their exceptional work. We would furthermore like to thank Christian Berger, Don-Philipp Dratschke, Matthias Joachim, Jean-Luc Kruppa, Henrick Langner, Bianca Schnake, Arne Steinbrück and Kai Zaengel for the organization of medical care, Annika Hampel for data processing and Torsten Bergemann of Nexave for the extraction from the electronic database.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None to specify.
Additional information
Alexandra Jablonka and Georg MN Behrens contributed equally.
Rights and permissions
About this article
Cite this article
Jablonka, A., Behrens, G.M.N., Stange, M. et al. Tetanus and diphtheria immunity in refugees in Europe in 2015. Infection 45, 157–164 (2017). https://doi.org/10.1007/s15010-016-0934-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-016-0934-7