Abstract
Purpose of Review
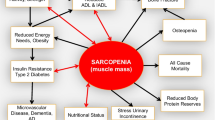
COPD exacerbations are widely recognised as a significant cause of mortality and morbidity through their impact on respiratory function but their effect on skeletal muscle function and mass receives less attention. In this article, we review the association of this entity with COPD, the potential contributing factors, and the evidence behind the interventions available to manage this condition with a focus on the elderly population.
Recent Findings
In patients with COPD, there has been a paradigm shift from the focus on body weight and mass index to a more detailed assessment of the loss of muscle mass and function defined as sarcopaenia. Factors that can potentially lead to sarcopaenia has been the subject of multiple basic science and translational research studies. Interventions that have been proven to be associated with clinically significant outcomes in COPD patients include early mobilisation, inpatient exercise programmes, early pulmonary rehabilitation, and nutritional interventions. Prolonged courses of steroids following an acute exacerbation are non-beneficial and can lead to loss of muscle function.
Summary
Multiple factors can potentially contribute to sarcopaenia among patients admitted with COPD exacerbations and should be identified early and treated in a multidisciplinary setting. Nutritional interventions, early mobilisation, and limitation of systemic steroid prescribing are simple and effective interventions that should be utilised.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
• Biolo G, Cederholm T, Muscaritoli M. Muscle contractile and metabolic dysfunction is a common feature of sarcopenia of aging and chronic diseases: from sarcopenic obesity to cachexia. Clin Nutr Edinb Scotl. 2014;33(5):737–48. Provides a very detailed yet succinct description of sarcopaenia and its causative factors.
Ståhl E, Lindberg A, Jansson S-A, Rönmark E, Svensson K, Andersson F, et al. Health-related quality of life is related to COPD disease severity. Health Qual Life Outcomes. 2005;3:56.
Akinbami LJ, Liu X. Chronic obstructive pulmonary disease among adults aged 18 and over in the United States, 1998–2009. NCHS Data Brief. 2011;63:1–8.
Maleki-Yazdi MR, Kelly SM, Lam SY, Marin M, Barbeau M, Walker V. The burden of illness in patients with moderate to severe chronic obstructive pulmonary disease in Canada. Can Respir J. 2012;19(5):319–24.
Ford ES, Murphy LB, Khavjou O, Giles WH, Holt JB, Croft JB. Total and state-specific medical and absenteeism costs of COPD among adults aged ≥ 18 years in the United States for 2010 and projections through 2020. Chest. 2015;147(1):31–45.
Bustacchini S, Chiatti C, Furneri G, Lattanzio F, Mantovani LG. The economic burden of chronic obstructive pulmonary disease in the elderly: results from a systematic review of the literature. Curr Opin Pulm Med. 2011;17(Suppl 1):S35–41.
World Health Organization. Chronic Obstructive Pulmonary Disease (COPD). 2018. Available from: http://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd).
Miravitlles M, Ferrer M, Pont A, Zalacain R, Alvarez-Sala JL, Masa F, Verea H, Murio C, Ros F, Vidal R, IMPAC Study Group. Effect of exacerbations on quality of life in patients with chronic obstructive pulmonary disease: a 2 year follow up study. Thorax 2004;59(5):387–395.
Donaldson GC, Wedzicha JA. COPD exacerbations .1: epidemiology. Thorax 2006;61(2):164–168.
Perera PN, Armstrong EP, Sherrill DL, Skrepnek GH. Acute exacerbations of COPD in the United States: inpatient burden and predictors of costs and mortality. COPD. 2012;9(2):131–41.
Miravitlles M, García-Polo C, Domenech A, Villegas G, Conget F, de la Roza C. Clinical outcomes and cost analysis of exacerbations in chronic obstructive pulmonary disease. Lung. 2013;191(5):523–30.
Singer JP, Peterson ER, Snyder ME, Katz PP, Golden JA, D’Ovidio F, et al. Body composition and mortality after adult lung transplantation in the United States. Am J Respir Crit Care Med. 2014;190(9):1012–21.
Xue Q-L, Walston JD, Fried LP, Beamer BA. Prediction of risk of falling, physical disability, and frailty by rate of decline in grip strength: the women’s health and aging study. Arch Intern Med. 2011;171(12):1119–21.
Dufour AB, Hannan MT, Murabito JM, Kiel DP, McLean RR. Sarcopenia definitions considering body size and fat mass are associated with mobility limitations: the Framingham Study. J Gerontol A Biol Sci Med Sci. 2013;68(2):168–74.
Janssen I. Evolution of sarcopenia research. Appl Physiol Nutr Metab Physiol Appl Nutr Metab. 2010;35(5):707–12.
Pitta F, Troosters T, Probst VS, Spruit MA, Decramer M, Gosselink R. Physical activity and hospitalization for exacerbation of COPD. Chest. 2006;129(3):536–44.
Garcia-Aymerich J, Farrero E, Félez MA, Izquierdo J, Marrades RM, Antó JM, Estudi del Factors de Risc d’Agudització de la MPOC investigators. Risk factors of readmission to hospital for a COPD exacerbation: a prospective study. Thorax 2003;58(2):100–105.
Cesari M, Pedone C, Chiurco D, Cortese L, Conte ME, Scarlata S, et al. Physical performance, sarcopenia and respiratory function in older patients with chronic obstructive pulmonary disease. Age Ageing. 2012;41(2):237–41.
• da Rocha Lemos Costa TM, Costa FM, Moreira CA, Rabelo LM, Boguszewski CL, Borba VZC. Sarcopenia in COPD: relationship with COPD severity and prognosis. J Bras Pneumol Publicacao Of Soc Bras Pneumol E Tisilogia. 2015;41(5):415–21. This paper evaluates the prevalence of sarcopaenia in COPD patients and also confirms that sarcopaenia correlates with a worse prognosis in COPD.
de Morton NA, Keating JL, Jeffs K. Exercise for acutely hospitalised older medical patients. Cochrane Database Syst Rev. 2007;1:CD005955.
Puhan MA, Gimeno-Santos E, Cates CJ, Troosters T. Pulmonary rehabilitation following exacerbations of chronic obstructive pulmonary disease. In: The Cochrane Library [Internet]. John Wiley & Sons, Ltd; 2016 [cited 2018 May 12]. Available from: https://doi.org/10.1002/14651858.CD005305.pub4/full
Rodriguez DA, Rodo-Pin A, Guerrero M, Coll R, Huerta A, Soler N, et al. Impact of step exercises as an early intervention during COPD exacerbation. Eur Respir J. 2016;48(suppl 60):PA2061.
Donaldson GC, Seemungal TAR, Patel IS, Bhowmik A, Wilkinson TMA, Hurst JR, et al. Airway and systemic inflammation and decline in lung function in patients with COPD. Chest. 2005;128(4):1995–2004.
Di Francia M, Barbier D, Mege JL, Orehek J. Tumor necrosis factor-alpha levels and weight loss in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1994;150(5 Pt 1):1453–5.
Byun MK, Cho EN, Chang J, Ahn CM, Kim HJ. Sarcopenia correlates with systemic inflammation in COPD. Int J Chron Obstruct Pulmon Dis. 2017;12:669–75.
Ferrando AA, Stuart CA, Sheffield-Moore M, Wolfe RR. Inactivity amplifies the catabolic response of skeletal muscle to cortisol. J Clin Endocrinol Metab. 1999;84(10):3515–21.
Bowyer SL, LaMothe MP, Hollister JR. Steroid myopathy: incidence and detection in a population with asthma. J Allergy Clin Immunol. 1985;76(2 Pt 1):234–42.
Decramer M, Lacquet LM, Fagard R, Rogiers P. Corticosteroids contribute to muscle weakness in chronic airflow obstruction. Am J Respir Crit Care Med. 1994;150(1):11–6.
Leuppi JD, Schuetz P, Bingisser R, Bodmer M, Briel M, Drescher T, et al. Short-term vs conventional glucocorticoid therapy in acute exacerbations of chronic obstructive pulmonary disease: the REDUCE randomized clinical trial. JAMA. 2013;309(21):2223–31.
Vermeeren M a P, Creutzberg EC, Schols AMWJ, Postma DS, Pieters WR, Roldaan AC, et al. Prevalence of nutritional depletion in a large out-patient population of patients with COPD. Respir Med. 2006;100(8):1349–55.
Schols AM, Slangen J, Volovics L, Wouters EF. Weight loss is a reversible factor in the prognosis of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998;157(6 Pt 1):1791–7.
Schols AMWJ, Broekhuizen R, Weling-Scheepers CA, Wouters EF. Body composition and mortality in chronic obstructive pulmonary disease. Am J Clin Nutr. 2005;82(1):53–9.
Prado CMM, Lieffers JR, McCargar LJ, Reiman T, Sawyer MB, Martin L, et al. Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: a population-based study. Lancet Oncol. 2008;9(7):629–35.
Del Fabbro E, Parsons H, Warneke CL, Pulivarthi K, Litton JK, Dev R, et al. The relationship between body composition and response to neoadjuvant chemotherapy in women with operable breast cancer. Oncologist. 2012;17(10):1240–5.
Muscaritoli M, Anker SD, Argilés J, Aversa Z, Bauer JM, Biolo G, et al. Consensus definition of sarcopenia, cachexia and pre-cachexia: joint document elaborated by Special Interest Groups (SIG) “cachexia-anorexia in chronic wasting diseases” and “nutrition in geriatrics”. Clin Nutr Edinb Scotl. 2010;29(2):154–9.
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, Martin FC, Michel JP, Rolland Y, Schneider SM, Topinková E, Vandewoude M, Zamboni M, European Working Group on Sarcopenia in Older People. Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in Older People. Age Ageing 2010;39(4):412–423.
Woo J, Leung J, Morley JE. Validating the SARC-F: a suitable community screening tool for sarcopenia? J Am Med Dir Assoc. 2014;15(9):630–4.
Metter EJ, Conwit R, Tobin J, Fozard JL. Age-associated loss of power and strength in the upper extremities in women and men. J Gerontol A Biol Sci Med Sci. 1997;52(5):B267–76.
Morley JE. Sarcopenia: diagnosis and treatment. J Nutr Health Aging. 2008;12(7):452–6.
Joseph A-M, Adhihetty PJ, Buford TW, Wohlgemuth SE, Lees HA, Nguyen LM-D, et al. The impact of aging on mitochondrial function and biogenesis pathways in skeletal muscle of sedentary high- and low-functioning elderly individuals. Aging Cell. 2012;11(5):801–9.
Bua EA, McKiernan SH, Wanagat J, McKenzie D, Aiken JM. Mitochondrial abnormalities are more frequent in muscles undergoing sarcopenia. J Appl Physiol Bethesda Md 1985. 2002;92(6):2617–24.
Hepple RT. Mitochondrial involvement and impact in aging skeletal muscle. Front Aging Neurosci. 2014;6:211.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Tara Cahill and Mohammed Ahmed declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Pulmonology and Respiratory Care
Rights and permissions
About this article
Cite this article
Cahill, T., Ahmed, M. Muscle Wasting in the Hospitalised COPD Patients—How Can it Be Prevented and Treated?. Curr Geri Rep 7, 147–153 (2018). https://doi.org/10.1007/s13670-018-0245-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13670-018-0245-1