Abstract
Purpose
Chronic respiratory diseases are prevalent among adults and lung function testing is imperative for appropriate diagnosis and treatment. While spirometry is the standard measure of lung function, there exist groups of individuals unable to adequately perform accurate and reproducible lung function testing. Impedance oscillometry system (IOS) is an effort independent test that may be employed to assess airway function in challenging groups such as children and elderly. This review will compare IOS and spirometry and describe the physiologic measurements of lung function and interpretation strategies in adults with chronic airway disease.
Recent Findings
In adults with COPD, impedance oscillometry measurements of airway resistance correlate with the severity of airflow limitation measured with spirometry. In adults with asthma, IOS is a sensitive measure of airway hyperresponsiveness and bronchodilator response.
Summary
Impedance oscillometry is emerging, alternative method to assess lung function in adults.


Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–128.
Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. Samet J, ed. PLoS Med. 2006;3(11):2011–30.
Adeloye D, Chua S, Lee C, Basquill C, Papana A, Theodoratou E, et al. Global and regional estimates of COPD prevalence: systematic review and meta-analysis. J Glob Health. 2015;5(2):020415.
National Center for Health Statistics. Health, United States, 2016: with chartbook on long-term trends in health.; 2017.
United States Department of Health and Human Services. The health consequences of smoking—50 years of progress a report of the surgeon general. A Rep Surg Gen. 2014:1081.
Malmberg LP, Pelkonen A, Poussa T, Pohianpalo A, Haahtela T, Turpeinen M. Determinants of respiratory system input impedance and bronchodilator response in healthy Finnish preschool children. Clin Physiol Funct Imaging. 2002;22:64–71.
Park JH, Yoon JW, Shin YH, Jee HM, Wee YS, Chang SJ, et al. Reference values for respiratory system impedance using impulse oscillometry in healthy preschool children. Korean J Pediatr. 2011;54(2):64–8.
Torre-Bouscoulet L, Velázquez-Uncal M, García-Torrentera R, et al. Spirometry quality in adults with very severe lung function impairment. Respir Care. 2015;60(5):740–3.
Schulz H, Flexeder C, Rgen Behr J, et al. Reference values of impulse oscillometric lung function indices in adults of advanced Age. PLoS One. 2013;8(5).
Hegewald MJ, Gallo HM, Wilson EL. Accuracy and quality of spirometry in primary care offices. Ann Am Thorac Soc. 2016;13(12):2119–24.
Borg BM, Hartley MF, Bailey MJ, Thompson BR. Adherence to acceptability and repeatability criteria for spirometry in complex lung function laboratories. Respir Care. 2012;57(12):2032–8.
Celli BR, Decramer M, Wedzicha JA, Wilson KC, Agustí A, Criner GJ, et al. An official American Thoracic Society/European Respiratory Society statement: research questions in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2015;191(7):e4–e27.
Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–38.
Dubois AB, Botelho SY, Comroe JH. A new method for measuring airway resistance in man using a body plethysmograph: values in normal subjects and in patients with respiratory disease. J Clin Invest. 1956;35(3):327–35.
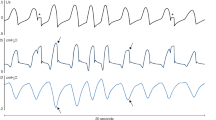
Smith HJ, Reinhold P GM. Forced oscillation technique and impulse oscillometry. Eur Repir Mon. 2005:72–105.
Uchida A, Ito S, Suki B, Matsubara H, Hasegawa Y. Influence of cheek support on respiratory impedance measured by forced oscillation technique. Springerplus. 2013;2(1):342.
Oostveen E, Macleod D, Lorino H, et al. The forced oscillation technique in clinical practice: methodology, recommendations and future developments on behalf of the ERS task force on respiratory impedance measurements. Eur Respir J. 2003;22(6):1026–41.
•• Bickel S, Popler J, Lesnick B, Eid N. Impulse oscillometry: interpretation and practical applications. Chest. 2014;146(3):841–7. https://doi.org/10.1378/chest.13-1875. Comprehensive review of impedance osciIlometry.
•• Galant SP, Komarow HD, Shin H-W, Siddiqui S, Lipworth BJ. The case for impulse oscillometry in the management of asthma in children and adults. Ann Allergy, Asthma Immunol. 2017;118(6):664–71. Excellent review of the application of IOS in pediatric and adult patients with asthma.
Kaminsky DA. What does airway resistance tell us about lung function? Respir Care. 2012;57(1):85–99.
• Kalchiem-Dekel Or, Hines SE. Forty years of reference values for respiratory system impedance in adults: 1977-2017. Respir Med. 2018;136:37–47. Summary of published studies reporting normal reference values or prediction equations for impedance oscillometry in adults. Height and gender were major contributors to prediction equations. Elderly subjects were underrepresented and ethnicity may play a role. For adults, reference values and prediction equations for respiratory impedance measurements is limited and there is a need for further large scale collection of respiratory impedance measurements.
Pasker HG, Schepers R, Clément J, Van De Woestijne KP. Total respiratory impedance measured by means of the forced oscillation technique in subjects with and without respiratory complaints. Eur Respir J. 1996;9(1):131–9.
Brown NJ, Xuan W, Salome CM, Berend N, Hunter ML, Musk AW(B), et al. Reference equations for respiratory system resistance and reactance in adults. Respir Physiol Neurobiol. 2010;172(3):162–8.
Làndsér FJ, Clément J, Van de Woestijne KP. Normal values of total respiratory resistance and reactance determined by forced oscillations. Chest. 1982;81(5):586–91.
Clément J, Làndsér FJ, Van de Woestijne KP. Total resistance and reactance in patients with respiratory complaints with and without airways obstruction. Chest. 1983;83(2):215–20.
Newbury W, Crockett A, Newbury J. A pilot study to evaluate Australian predictive equations for the impulse oscillometry system. Respirology. 2008;13(7):1070–5.
Guo YF, Herrmann F, Michel J-P, Janssens J-P. Normal values for respiratory resistance using forced oscillation in subjects >65 years old. Eur Respir J. 2005;26(4):602–8.
Parshall MB, Schwartzstein RM, Adams L, Banzett RB, Manning HL, Bourbeau J, et al. An official American Thoracic Society statement: update on the mechanisms, assessment, and management of dyspnea. Am J Respir Crit Care Med. 2012;185(4):435–52.
Vestbo J, Lange P. Can GOLD stage 0 provide information of prognostic value in chronic obstructive pulmonary disease? Am J Respir Crit Care Med. 2002;166(3):329–32.
Woodruff PG, Barr RG, Bleecker E, Christenson SA, Couper D, Curtis JL, et al. Clinical significance of symptoms in smokers with preserved pulmonary function. N Engl J Med. 2016;374(19):1811–21.
Brown NJ, Xuan W, Salome CM, Berend N, Hunter ML, Musk AW(B), et al. Reference equations for respiratory system resistance and reactance in adults. Respir Physiol Neurobiol. 2010;172(3):162–8.
Frantz S, Nihlén U, Dencker M, Engström G, Löfdahl CGG, Wollmer P. Impulse oscillometry may be of value in detecting early manifestations of COPD. Respir Med. 2012;106(8):1116–23.
Kolsum U, Borrill Z, Roy K, Starkey C, Vestbo J, Houghton C, et al. Impulse oscillometry in COPD: identification of measurements related to airway obstruction, airway conductance and lung volumes. Respir Med. 2009;103(1):136–43.
• Crim C, Celli B, Edwards LD, et al. Respiratory system impedance with impulse oscillometry in healthy and COPD subjects: ECLIPSE baseline results. Respir Med. 2011;105(7):1069–78. Comparison of spirometry and lung impedance measurements by IOS was performed in healthy non-smokers, healthy former smokers, and patients with COPD. In the COPD group, respiratory system impedance was worse compared with controls. Compared to healthy non-smokers, 29–86% of the COPD subjects had values that fell within the 90% confidence interval of several parameters. IOS can be reliably used in large cohorts of subjects to assess respiratory system impedance.
Berger KI, Goldring RM, Oppenheimer BW. Should oscillometry be used to screen for airway disease? Yes. Chest. 2015;148(5):1131–5.
•• Enright PL. COUNTERPOINT: should oscillometry be used to screen for airway disease? No. Chest. 2015;148(5):1135–6. Balanced discussion regarding the potential benefits and limitations in screening for airway disease.
Celli BR, MacNee W, Agusti A, Anzueto A, Berg B, Buist AS, et al. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J. 2004;23(6):932–46.
Chung KF, Wenzel SE, Brozek JL, Bush A, Castro M, Sterk PJ, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J. 2014;43(2):343–73.
Nair A, Ward J, Lipworth BJ. Comparison of bronchodilator response in patients with asthma and healthy subjects using spirometry and oscillometry. Ann Allergy Asthma Immunol. 2011;107(4):317–22.
Williamson PA, Clearie K, Menzies D, Vaidyanathan S, Lipworth BJ. Assessment of small-airways disease using alveolar nitric oxide and impulse oscillometry in asthma and COPD. Lung. 2011;189(2):121–9.
Robinson PD, King GG, Sears MR, Hong CY, Hancox RJ. Determinants of peripheral airway function in adults with and without asthma. Respirology. 2017;22(6):1110–7.
Young HM, Guo F, Eddy RL, Maksym G, Parraga G. Oscillometry and pulmonary MRI measurements of ventilation heterogeneity in obstructive lung disease: relationship to quality of life and disease control. J Appl Physiol. 2018;125(1):73–85.
Ortiz G, Menendez R. The effects of inhaled albuterol and salmeterol in 2- to 5-year-old asthmatic children as measured by impulse oscillometry. J Asthma. 2002;39(6):531–6.
Komarow HD, Skinner J, Young M, Gaskins D, Nelson C, Gergen PJ, et al. A study of the use of impulse oscillometry in the evaluation of children with asthma: analysis of lung parameters, order effect, and utility compared with spirometry. Pediatr Pulmonol. 2012;47(1):18–26.
Mansur AH, Manney S, Ayres JG. Methacholine-induced asthma symptoms correlate with impulse oscillometry but not spirometry. Respir Med. 2008;102(1):42–9.
Naji N, Keung E, Kane J, Watson RM, Killian KJ, Gauvreau GM. Comparison of changes in lung function measured by plethymography and IOS after bronchoprovocation. Respir Med. 2013;107(4):503–10.
Schulze J, Smith HJ, Fuchs J, Herrmann E, Dressler M, Rose MA, et al. Methacholine challenge in young children as evaluated by spirometry and impulse oscillometry. Respir Med. 2012;106(5):627–34.
Short PM, Anderson WJ, Manoharan A, Lipworth BJ. Usefulness of impulse oscillometry for the assessment of airway hyperresponsiveness in mild-to-moderate adult asthma. Ann Allergy Asthma Immunol. 2015;115(1):17–20.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Mohammed F. Zaidan, Shahanaz Meah, and Alexander Duarte declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on COPD and Asthma
Rights and permissions
About this article
Cite this article
Zaidan, M.F., Meah, S. & Duarte, A. The Use and Interpretation of Impedance Oscillometry in Pulmonary Disorders. Curr Pulmonol Rep 7, 196–202 (2018). https://doi.org/10.1007/s13665-018-0218-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13665-018-0218-z