Abstract
Introduction
No hierarchy of first-line treatments for anogenital warts (AGWs) is provided in international guidelines. This study aimed to determine the efficacy of topical treatments and ablative procedures for the management of AGWs.
Methods
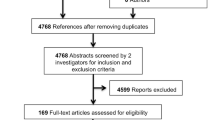
Twelve electronic databases were systematically searched from inception to August 2018. All randomized controlled trials (RCTs) comparing immunocompetent adults with AGWs who received at least 1 provider-administered or patient-administered treatment in at least 1 parallel group were included. Risk of bias assessment followed the Cochrane Handbook. The study endpoint was complete lesion response after clearance and recurrence assessment. A network meta-analysis was performed.
Results
A network geometry was constructed based on 49 of the 70 RCTs included in our systematic review. All but 4 RCTs had a high risk of bias. The most efficacious treatments compared to placebo were surgery (RR 10.54; CI 95% 4.53–24.52), ablative therapy + imiquimod (RR 7.52; CI 95% 4.53–24.52), and electrosurgery (RR 7.10; CI 95% 3.47–14.53). SUCRA values confirmed the superiority of surgery (90.9%), ablative therapy + imiquimod (79.8%), and electrosurgery (77.1%). The most efficacious patient-administered treatments were podophyllotoxin 0.5% solution (63.5%) and podophyllotoxin 0.5% cream (62.2%).
Conclusions
With low-level evidence of most included RCTs, surgery and electrosurgery were superior to other treatments after clearance and recurrence assessment. Podophyllotoxin 0.5% was the most efficacious patient-administered treatment. Combined therapies should be evaluated in future RCTs in view of their identified effectiveness. The results of future RCTs should systematically include clinical type, number and location of AGWs, and sex of the patient, to refine therapeutic indications.
Protocol Registration
PROSPERO-CRD42015025827
Similar content being viewed by others
Why carry out this study? | |
Anogenital warts (AGWs) are one of the most common sexually transmitted diseases, with an overall prevalence rate of around 1–5%. | |
No clinically meaningful hierarchy of first-line treatments for anogenital warts is provided in international guidelines. | |
What was learned from the study? | |
Based on a low level of evidence, surgery and electrosurgery achieved the best complete lesion response after clearance and recurrence assessment. | |
Podophyllotoxin 0.5% was the most efficacious patient-administered treatment. |
Introduction
Anogenital warts (AGWs) are benign epithelial skin lesions that are predominantly caused by the human papillomavirus (HPV types 6 and 11), but are sometimes associated with other types of oncogenic HPV [1]. With an overall prevalence rate of around 1–5%, they are one of the most common sexually transmitted infections [2]. AGWs are usually asymptomatic, but they can be painful or pruritic and can cause significant psychosocial distress depending on size and location [3, 4]. Numerous HPV vaccination campaigns have been conducted, but few studies have demonstrated their efficacy in reducing the number of AGWs [5]. Moreover, in most countries, vaccination coverage is partial and has yet to be extended to men [6, 7].
Many treatments are available to treat AGWs. These can be divided into provider-administered treatments (ProTs) [trichloroacetic acid (TCA), podophyllin resin, CO2 laser surgery, cryotherapy, surgical excision, electrosurgery, intralesional therapy, etc.] and patient-administered treatments (PaTs) [podophyllotoxin, imiquimod, sinecatechins, 5-fluorouracil (5-FU) cream, etc.]. The latest guidelines [8,9,10,11] recommend that treatment of AGWs be adapted to: size, number, and anatomic site of AGWs; patient preference; convenience; adverse effects; cost of treatment; and physician experience. These recommendations, however, are based on head-to-head randomized trials or on expert advice. Furthermore, RCTs comparing several major treatments for AGWs (cryotherapy [12] vs podophyllotoxin cream or gel, imiquimod vs TCA, CO2 laser vs surgery or electrosurgery, etc.) are lacking [10, 13,14,15] and may never be performed (because they are costly, time-consuming, less attractive than new treatments, etc.). Reliable evidence on the comparative efficacy of these treatments is nevertheless needed to make informed clinical decisions.
In this context, network meta-analyses (NMAs) can help compare the relative benefits associated with different types of intervention for the same disease [16, 17]. The only NMA on AGWs, which was conducted by Barton et al. [13] based on a systematic review up to March 2018, concluded that ablative techniques were superior; it also found podophyllotoxin 0.5% gel to be the most cost-effective topical treatment. However, this NMA did not examine sinecatechins, 5-FU cream, and several RCTs on new treatments [citric acid, intralesional bleomycin, potassium hydroxide (KOH), photodynamic therapy (PDT), etc.].
Our NMA aims to establish a clinically meaningful hierarchy of PaTs and ProTs for the management of AGWs.
Methods
The study protocol is registered with PROSPERO (No. CRD42015025827). The systematic review, which was published earlier [14], adheres to the PRISMA Statement [18]. The present study adheres to the PRISMA extension for NMA [19]. This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Systematic Review
Twelve electronic databases were systematically searched from inception to August 2018 by 2 independent reviewers (A.B. and C.D.). Search terms included 2 synonym groups, AGW and RCT, with adjustments for each database (Appendix S1). The reference lists of all published studies and all recent reviews and meta-analyses were also searched [8,9,10, 13, 20,21,22]. No language restriction was imposed. To be included in the NMA, RCTs had to: (1) have at least 1 treatment group composed of immunocompetent adults clinically diagnosed with AGWs and treated with a ProT (TCA, podophyllin, CO2 laser, cryotherapy, surgical excision, electrosurgery, all intralesional treatments, KOH, PDT, citric acid) or a PaT [podophyllotoxin, imiquimod, sinecatechins, 5-FU, cidofovir, interferon (INF) cream]; and (2) provide original estimates with risk ratios and confidence intervals (CIs) or present sufficient data to allow calculation of these estimates. Complete lesion response (CLR) at the end of follow-up was assessed based on two outcome measures: clearance at 3 months and recurrence 3 months later.
An extraction grid was developed after collegial discussion. For all selected studies, variables of interest were extracted independently by 2 independent reviewers (A.B. and C.D.). These reviewers assessed the risk of bias in the selected RCTs using the Cochrane Collaboration Risk of Bias tool [23]. When different RCTs involved the same patient cohort, the RCT with the longest follow-up period was considered.
Data Synthesis
An NMA was performed that combined the results of all selected comparisons of AGW treatments. This statistical technique is used to account for direct comparisons performed in single trials and to make indirect comparisons across trials based on a common comparator intervention [24]. In our NMA, placebo and podophyllin served as comparators for indirect comparisons even though they are not used in clinical practice. For RCTs comparing treatments at lower or higher dosages than recommended in published guidelines, only recommended dosages were considered. All analyses were performed with a frequentist approach using a random effects model, with an equal heterogeneity variance assumed for all comparisons.
The network geometry was assessed by graphically examining the connections between interventions [17]. Each node represented an intervention. The thickness of nodes was proportional to the number of allocated patients. The thickness of connecting lines was inversely proportional to the variance between 2 interventions.
Netmeta R package version 8.0 (available at: https://CRAN.R-project.org/package=netmeta) was used to perform head-to-head comparisons of different treatments to a placebo [25]. Specifically, 2 forest plots using random effects models were generated by calculating point estimates of relative risk (RR) with a CI 95%. A heat mapping function (which is a type of matrix visualization) was created with the Netmeta R package to evaluate heterogeneity and inconsistency [26]. Warmer or cooler colors indicated significant inconsistency.
The patient was the unit of analysis for all RCTs. The endpoint—CLR after clearance and recurrence assessment—was evaluated using per protocol analysis (cured patients/follow-up patients). Sensitivity analyses of 2 scenarios were performed: (1) a worst-case (intention to treat) scenario, in which patients lost to follow-up were considered to be failing treatment (cured patients/all included patients); and (2) a best-case scenario, in which patients lost to follow-up were considered cured [(cured patients + lost to follow-up patients)/all included patients].
The probability that each intervention achieved CLR was estimated based on the relative effect sizes estimated with the NMA. A hierarchy of compared interventions was performed using the Surface Under the Cumulative Ranking curve (SUCRA). SUCRA values are expressed as percentages and show the relative probability of an intervention being among the best options.
Results
Characteristics of Selected Trials
Seventy RCTs involving 9931 patients with a mean of 142 participants per study fulfilled the inclusion criteria [14] (Appendix S2–S3). The overwhelming majority of included RCTs (66/70) were found to be of poor quality (Appendix S4) [14]. Twenty-one RCTs were excluded from the NMA: 6 because they compared dosages that were lower than recommended [27,28,29,30,31,32], 14 because they did not evaluate recurrence [33,34,35,36,37,38,39,40,41,42,43,44,45,46], and 1 because it was disconnected from the network (intralesional bleomycin vs podophyllin + cryotherapy) [47].
Nine studies comparing a recommended dosage with a lower dosage were included, but without the treatment arm that received the lower dosage [48,49,50,51,52,53,54,55,56]. Ultimately, 29 treatments or combination therapies were included. One RCT compared 4 arms [57], 5 RCTs compared 3 arms [58,59,60,61,62], and 43 compared 2 arms [48,49,50,51,52,53,54,55,56, 63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96]. Following these inclusion criteria, only two of 4 low risk of bias RCTs were included [27, 45]. The median follow-up for the 6006 covered patients was 6 months (3–12 month range).
Network Geometry
The complex network generated from the 49 included RCTs is shown in Fig. 1. Compared treatments were connected either directly or indirectly through 1 or more “comparators.” The level of evidence informing each comparison was evaluated. Treatment comparisons involving the largest number of patients were polyphenon vs placebo (3 trials; 767 patients receiving treatment) and podophyllin vs podophyllotoxin gel (6 trials; 1005 patients receiving treatment). Only 12 RCTs [50, 57, 58, 62, 77, 78, 81, 83, 84, 87, 90, 96] directly compared a ProT to a PaT; of these, 9 examined treatments that are not used in clinical practice (6 on podophyllin and 3 on intralesional therapies). The most commonly studied agents were placebo (18 trials; 939 patients receiving treatment) and podophyllin (13 trials; 716 patients receiving treatment).
Evidence network of eligible comparisons for complete lesion response in network meta-analysis. The thickness of connecting lines represents the cumulative number of trials for each comparison, and the thickness of nodes is proportional to the number of enrolled participants. Cryo cryotherapy, ablative ablative treatment (surgery or electrosurgery or CO2 laser or cryotherapy), imi imiquimod 5%, 5-FU 5 fluorouracil, 5-FU intra intralesional 5 fluorouracil, TCA trichloroacetic acid, podo podophyllin 20–25%, citric ac citric acid 9%, polyph polyphenon 15%, podotox cr podophyllotoxin 0.5% cream, podotox cr/gel podophyllotoxin 0.5% gel + cream, podotox gel podophyllotoxin 0.5% gel, PDT photodynamic therapy, mycobac intra intralesional Mycobacterium, KOH potassium hydroxide, electro electrosurgery, INF-1a intra intralesional interferon-1α, INF-2b intra intralesional interferon-2β
Forest plot of the estimates of relative risk between each treatment and the reference placebo for complete lesion response. Data presented as RR (95% CI). Cryo cryotherapy, ablative ablative treatment (surgery or electrosurgery or CO2 laser or cryotherapy), imi imiquimod 5%, 5-FU 5 fluorouracil, 5-FU intra intralesional 5 fluorouracil, TCA trichloroacetic acid, podo podophyllin 20–25%, citric ac citric acid 9%, polyph polyphenon 15%, podotox cr podophyllotoxin 0.5% cream, podotox cr/gel podophyllotoxin 0.5% gel + cream, podotox gel podophyllotoxin 0.5% gel, PDT photodynamic therapy, mycobac intra intralesional Mycobacterium, KOH potassium hydroxide, electro electrosurgery, INF-1a intra intralesional interferon-1α, INF-2b intra intralesional interferon-2β
Complete Lesion Response
Figure 2 presents the CLR of all treatments and placebos compared using a random effects model. Most CIs were wide, but rarely included value 1. Cidofovir, citric acid 9%, intralesional INF, intralesional placebo, and polyphenon 15% achieved a CLR not significantly different from placebo. Surgery (RR 10.54; CI 95% 4.53–24.52), ablative therapy + imiquimod (RR 7.52; CI 95% 3.63–15.57), and electrosurgery (RR 7.10; CI 95% 3.47–14.53) achieved the best CLR compared to placebo. Other comparisons to placebo had RRs that ranged from 3.84 to 6.75
Head-to-head comparisons using NMA are shown in the online supplement (Appendix S5). Surgery was more efficacious than imiquimod (RR 2.22; CI 95% 1.04–4.76), TCA (RR 2.28; CI 95% 1.09–4.75), KOH (RR 2.48; CI 95% 1.02–6.01), cryotherapy (RR 2.43; CI 95% 1.17–5.03), 5-FU (RR 2.44; CI 95% 1.07–5.56), and polyphenon (RR 7.07, CI 95% 2.82–17.72). No significant differences were found between surgery and other ablative therapies (electrosurgery, CO2 laser), or between surgery and podophyllotoxin 0.5% solution or 0.5% cream. As regards direct comparisons (except for those involving a placebo or podophyllin), the only significant result was the superiority of CO2 laser over cryotherapy (RR 2.40; CI 95% 1.29–4.46).
Examined RCTs presented both heterogeneity and inconsistency. The Netmeta R package provided an I2 value of 60% from a Q statistic for the overall network of 70.7, which had a chi-square distribution with 28 degrees of freedom and yielded a p-value of 0.0001 [25]. The Q statistic was further decomposed into heterogeneity and inconsistency components, valued at 14.7 and 56.0, respectively.
As shown in the net heat plot in Fig. 3, a high inconsistency among mapping functions was found for RCTs comparing the following treatments: cryotherapy vs podophyllin 20–25% vs electrosurgery; 5-FU vs podophyllin; 5-FU vs CO2 laser vs 5-FU + CO2 laser; and CO2 laser vs cryotherapy. Treatments examined in a single study were not evaluated.
Net heat plot. Assessment of consistency between direct and indirect evidence. Horizontal: detached comparisons; vertical: comparisons observed in the network; warm color in the net heat plot indicates that significant inconsistency may arise from a specific comparison and this trend is illustrated by the intensity of the color; gray color: contribution of each direct comparison to the network estimates
Table 1 presents the SUCRA results that emerged from these data. These results confirm that ablative therapy, surgery (90.9%), and electrosurgery (77.1%) are the most efficacious treatments for AGWs. The SUCRA value of combination therapies was also good (PDT + CO2 laser: 68.0%; CO2 laser + 5-FU: 67.4%; Cryotherapy + podophyllotoxin 0.5% cream: 59.5%). Podophyllotoxin 0.5% solution (63.5%) and podophyllotoxin 0.5% cream (62.2%) had the highest SUCRA values of all PaTs. The SUCRA values of imiquimod, TCA, KOH, cryotherapy, and 5-FU ranged from 40 to 50%. The SUCRA value for polyphenon 15% was low at 13.1%.
Sensitivity Analyses
Only polyphenon and podophyllin + TCA had a CI that included value 1 (Appendix S6).
Worst-case (intention to treat) scenario sensitivity analyses showed a superiority of surgery over podophyllotoxin 0.5% solution (RR 1.94; CI 95% 1.00–3.76), CO2 laser (RR 2.20; CI 95% 1.05–4.60), electrosurgery (RR 2.28; CI 95% 1.10–4.74), and cryotherapy + podophyllotoxin 0.5% cream (RR 2.68; CI 95% 1.18–6.07). Ablative therapy + imiquimod was superior to imiquimod alone (RR 1.57; CI 95% 1.01–2.44) and to cryotherapy (RR 1.74; CI 95% 1.05–2.89). A superiority of podophyllotoxin 0.5% cream and podophyllotoxin 0.5% solution over cryotherapy was also found (RR 1.66; CI 95% 1.04–2.66 and RR 1.52; CI 95% 1.06–2.18, respectively) (Appendix S7).
Sensitivity analyses of SUCRA values confirmed the superiority of surgery and combination therapies. Worst-case scenario sensitivity analyses showed an increase in the efficacy of podophyllotoxin 0.5% cream and 0.5% solution (72.2% and 77.7%, respectively), as well as a decrease in the efficacy of electrosurgery due to the high number of patients lost to follow-up in the study by Stone et al. [61] (Appendix S8).
Discussion
In our NMA, ProTs — mainly surgery and electrosurgery — achieved the best CLR, with a median follow-up of 6 months. These results differ from our pooled analysis, which found higher clearance for ProTs but lower recurrence at 12 months for PaTs [97]. Few RCTs have used CLR as a study endpoint. This is unfortunate given that CLR, which assesses clearance until no recurrence, is more meaningful for patients undergoing treatment for AGWs. Combined with the more robust statistical methods of NMA, this endpoint yields more accurate results than pooled analyses. Cidofovir was ranked 4th in our SUCRA analysis. Yet, it is difficult to conclude on the efficacy of this treatment, as the only RCT on the topic found no significant difference with placebo use.
Our results are in line with the NMA of Barton et al. [13], which concluded that ablative techniques were superior. However, unlike us, Barton et al. recommended CO2 laser as first-line treatment. This difference may be explained by the fact that their NMA was restricted to 39 RCTs, included immunocompromised patients and only one RCT using CO2 laser [64], whereas our NMA compared 49 RCTs, focused on non-immunocompromised adults and compared 5 RCTs using CO2 laser [59, 64, 69, 70, 92]. Moreover, Barton et al. found that podophyllotoxin 0.5% solution was the most cost-effective therapeutic solution, followed by CO2 laser. In our NMA, podophyllotoxin 0.5% solution achieved the best CLR among all PaTs.
Unlike systematic reviews on AGW management [10, 13, 97], our NMA examined the efficacy of combination therapies, including ablative therapy + imiquimod, cryotherapy + podophyllotoxin 0.5% cream, and CO2 laser + 5-FU. However, many combination therapies are missing from our NMA, including those most commonly recommended and used in practice: cryotherapy + imiquimod and cryotherapy + podophyllotoxin 0.5% solution. Combination therapies should be given greater consideration and should be adapted as best as possible to individual patients.
Our search was limited by restrictions on access to Chinese databases, especially regarding treatments like PDT. While our NMA results suggest that this treatment is highly efficacious, they are based on only 1 RCT (note that numerous non-randomized studies on MEDLINE have yielded the same finding [98, 99]). Other RCTs on PDT have likely been performed, but they remain inaccessible to the scientific community.
The management of AGWs is heterogeneous in terms of: the type of treatment used; the level of physician experience (for ProTs); the level of patient compliance (for PaTs); the clinical type of AGWs (papillary, flat, or pedunculated); the location of AGWs; the number of AGWs; and the sex of the patient [100, 101]. Such heterogeneity renders more difficult the establishment of a clinically meaningful hierarchy of treatments. In our systematic review, more than 90% of RCTs were found to have a high risk of bias [14], thus casting doubt on the validity of published recommendations. NMAs do not increase the level of evidence of risks of bias, as they remain dependent on the methodology of each RCT. But they do increase statistical power because they encompass all patients included in examined RCTs. Moreover, NMAs can be used to compare treatments that have never been compared before, to identify gaps in knowledge, and to help develop clinically meaningful hierarchies of treatments [24].
Only 2 RCTs in our NMA compared a recommended ProT to a recommended PaT (imiquimod and cryotherapy in both cases) [58, 90]. Future RCTs should compare recommended ProTs and PaTs—for instance, cryotherapy vs podophyllotoxin cream or solution; surgery vs imiquimod; surgery vs podophyllotoxin cream or solution; CO2 laser vs imiquimod; and CO2 laser vs podophyllotoxin cream or solution. Moreover, combination therapies should be more thoroughly assessed to help increase the efficacy of AGW management, and to make it better adapted to the number, type, and location of AGWs. New treatments (KOH, PDT alone or as an adjuvant) should also be evaluated further. Although 5-FU was not mentioned in guidelines until 2019 [10], it could be proposed as a second-line treatment in the future.
Our systematic review and our NMA should be updated regularly. Side effects should be assessed to help physicians personalize treatments for their individual patients. Lastly, study endpoints and ProT use practices (e.g., standardization of freezing or surgical procedures) should be homogenized to allow better comparison of RCTs.
Conclusions
To conclude, in our NMA, surgery and electrosurgery achieved the best CLR, and podophyllotoxin 0.5% was the most efficacious patient-administered treatment. Combined therapies should be evaluated more in future RCTs in view of their identified effectiveness. The results of future RCTs should systematically include clinical type, number and location of AGWs, and sex of the patient, to refine therapeutic indications.
References
Aubin F, Prétet J-L, Jacquard A-C, et al. Human papillomavirus genotype distribution in external acuminata condylomata: a large French national study (EDiTH IV). Clin Infect Dis. 2008;47:610–5.
Patel H, Wagner M, Singhal P, et al. Systematic review of the incidence and prevalence of genital warts. BMC Infect Dis. 2013;13:39.
Qi S-Z, Wang S-M, Shi J-F, et al. Human papillomavirus-related psychosocial impact of patients with genital warts in China: a hospital-based cross-sectional study. BMC Public Health. 2014;14:739.
Woodhall SC, Jit M, Soldan K, et al. The impact of genital warts: loss of quality of life and cost of treatment in eight sexual health clinics in the UK. Sex Transm Infect. 2011;87:458–63.
Drolet M, Bénard É, Boily M-C, et al. Population-level impact and herd effects following human papillomavirus vaccination programmes: a systematic review and meta-analysis. Lancet Infect Dis. 2015;15:565–80.
Bruni L, Diaz M, Barrionuevo-Rosas L, et al. Global estimates of human papillomavirus vaccination coverage by region and income level: a pooled analysis. Lancet Glob Health. 2016;4:e453–e463463.
Sinisgalli E, Bellini I, Indiani L, et al. HPV vaccination for boys? A systematic review of economic studies. Epidemiol Prev. 2015;39:51–8.
Gross GE, Werner RN, Becker JC, et al. A.S2k guideline: HPV-associated lesions of the external genital region and the anus — anogenital warts and precancerous lesions of the vulva, the penis, and the peri- and intra-anal skin (short version). J Dtsch Dermatol Ges. 2018;16:242–255
Anogenital warts - 2015 STD Treatment Guidelines. https://www.cdc.gov/std/tg2015/warts.htm. Accessed July 17, 2015.
Gilson R, Nugent D, Werner RN, Ballesteros J. 2019 European Guideline for the Management of Anogenital Warts. https://www.iusti.org/regions/Europe/pdf/2019/IUSTIguidelinesHPV2019.pdf. Accessed May 16, 2019
Bouscarat F, Pelletier F, Fouéré S, Janier M, Bertolloti A, Aubin F, La section MST de la SFD. External genital warts (condylomata). Ann Dermatol Venereol. 2016;143:741–5
Bertolotti A, Dupin N, Bouscarat F, et al. Cryotherapy to treat anogenital warts in non-immunocompromised adults: systematic review and meta-analysis. J Am Acad Dermatol. 2017;77:518–26.
Barton S, Wakefield V, O'Mahony C, Edwards S. Effectiveness of topical and ablative therapies in treatment of anogenital warts: a systematic review and network meta-analysis. BMJ Open. 2019;31(9):e027765.
Bertolotti A, Milpied B, Fouéré S, Cabié A, Dupin N, Derancourt C. Methodological gaps and risk of bias in randomized controlled trials of local anogenital warts treatments. J Am Acad Dermatol. 2019;81:1197–8.
Bertolotti A, Milpied B, Fouéré S, Dupin N, Cabié A, Derancourt C. Local management of anogenital warts in non-immunocompromised adults: a systematic review and meta-analyses of randomized controlled trials. Dermatol Ther (Heidelb). 2019;9:761–74.
Lu G, Ades AE. Combination of direct and indirect evidence in mixed treatment comparisons. Stat Med. 2004;23:3105–24.
Mills EJ, Thorlund K, Ioannidis JP. Demystifying trial networks and network meta-analysis. BMJ. 2013;346:f2914.
Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;349:g7647.
Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162:777–84.
Batista CS, Atallah AN, Saconato H, et al. 5-FU for genital warts in non-immunocompromised individuals. Cochrane Database Syst Rev. 2010;(4):CD006562
Grillo-Ardila CF, Angel-Müller E, Salazar-Díaz LC, et al. Imiquimod for anogenital warts in non-immunocompromised adults. Cochrane Database Syst Rev. 2014;11:CD010389
Yan J, Chen S-L, Wang H-N, et al. Meta-analysis of 5% imiquimod and 0.5% podophyllotoxin in the treatment of condylomata acuminata. Dermatol Basel Switz. 2006;213:218–23
Higgins JPT, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Caldwell DM, Ades AE, Higgins JP. Simultaneous comparison of multiple treatments: combining direct and indirect evidence. BMJ. 2005;331:897–900.
Neupane B, Richer D, Bonner AJ, Kibret T, Beyene J. Network meta-analysis using R: a review of currently available automated packages. PLoS ONE. 2014;9:e115065.
Biondi-Zoccai G, editor. Network meta-analysis: evidence synthesis with mixed treatment comparison. Hauppauge: Nova Science Publishers; 2014.
Baker DA, Ferris DG, Martens MG, et al. Imiquimod 3.75% cream applied daily to treat anogenital warts: combined results from women in two randomized, placebo-controlled studies. Infect Dis Obstet Gynecol. 2011:806105
Claesson U, Lassus A, Happonen H, et al. Topical treatment of venereal warts: a comparative open study of podophyllotoxin cream versus solution. Int J STD AIDS. 1996;7:429–34.
Strand A, Brinkeborn RM, Siboulet A. Topical treatment of genital warts in men, an open study of podophyllotoxin cream compared with solution. Genitourin Med. 1995;71:387–90.
Syed TA, Ahmadpour OA, Ahmad SA, et al. Management of female genital warts with an analog of imiquimod 2% in cream: a randomized, double-blind, placebo-controlled study. J Dermatol. 1998;25:429–33.
Syed TA, Hadi SM, Qureshi ZA, et al. Treatment of external genital warts in men with imiquimod 2% in cream. A placebo-controlled, double-blind study. J Infect. 2000;41:148–51
White DJ, Billingham C, Chapman S, et al. Podophyllin 0.5% or 2.0% v podophyllotoxin 0.5% for the self treatment of penile warts: a double blind randomised study. Genitourin Med. 1997;73:184–7
Abdullah AN, Walzman M, Wade A. Treatment of external genital warts comparing cryotherapy (liquid nitrogen) and trichloroacetic acid. Sex Transm Dis. 1993;20:344–5.
Edwards A, Atma-Ram A, Thin RN. Podophyllotoxin 0.5% v podophyllin 20% to treat penile warts. Genitourin Med. 1988;64:263–5
Komericki P, Akkilic-Materna M, Strimitzer T, et al. Efficacy and safety of imiquimod versus podophyllotoxin in the treatment of anogenital warts. Sex Transm Dis. 2011;38:216–8.
Mazurkiewicz W, Jablońska S. Clinical efficacy of Condyline (0.5% podophyllotoxin) solution and cream versus podophyllin in the treatment of external condylomata acuminata. J Dermatol Treat. 1990;1:123–5
On SCJa, Linkner RVa, Haddican Ma, et al. A single-blinded randomized controlled study to assess the efficacy of twice daily application of sinecatechins 15% ointment when used sequentially with cryotherapy in the treatment of external genital warts. J Drugs Dermatol. 2014:13:1400–5
Sherrard J, Riddell L. Comparison of the effectiveness of commonly used clinic-based treatments for external genital warts. Int J STD AIDS. 2007;18:365–8.
Simmons PD, Langlet F, Thin RN. Cryotherapy versus electrocautery in the treatment of genital warts. Br J Vener Dis. 1981;57:273–4.
Syed TA, Khayyami M, Kriz D, et al. Management of genital warts in women with human leukocyte interferon-alpha vs. podophyllotoxin in cream: a placebo-controlled, double-blind, comparative study. J Mol Med Berl Ger. 1995;73:255–8
Tyring SK, Arany I, Stanley MA, et al. A randomized, controlled, molecular study of condylomata acuminata clearance during treatment with imiquimod. J Infect Dis. 1998;178:551–5.
Weismann K, Kassis V. Treatment of condyloma acuminatum with 0.5% 5-fluorouracil-solution, a double-blind clinical trial. Z Für Hautkrankh. 1982;57:810–6
Keay S, Teng N, Eisenberg M, et al. Topical interferon for treating condyloma acuminata in women. J Infect Dis. 1988;158:934–9.
Reichman RC, Oakes D, Bonnez W, et al. Treatment of condyloma acuminatum with three different interferons administered intralesionally. A double-blind, placebo-controlled trial. Ann Intern Med. 1988;108:675–9
Vance JC, Bart BJ, Hansen RC, et al. Intralesional recombinant alpha-2 interferon for the treatment of patients with condyloma acuminatum or verruca plantaris. Arch Dermatol. 1986;122:272–7.
Welander CE, Homesley HD, Smiles KA, et al. Intralesional interferon alfa-2b for the treatment of genital warts. Am J Obstet Gynecol. 1990;162:348–54.
Mahajan BBA, Tilak Raj Rb, Kumar R. A comparative evaluation of therapeutic efficacy and safety of the cryotherapy (liquid nitrogen) with topical 20% podophyllin v/s intralesional bleomycin with topical 5% placentrex gel in the treatment of condyloma acuminata. Asian J Pharm Clin Res. 2014:7:36–42
Beutner KR, Tyring SK, Trofatter KF, et al. Imiquimod, a patient-applied immune-response modifier for treatment of external genital warts. Antimicrob Agents Chemother. 1998;42:789–94.
Edwards L, Ferenczy A, Eron L, et al. Self-administered topical 5% imiquimod cream for external anogenital warts. HPV Study Group. Human PapillomaVirus. Arch Dermatol. 1998;134:25–30
Lacey CJN, Goodall RL, Tennvall GR, et al. Randomised controlled trial and economic evaluation of podophyllotoxin solution, podophyllotoxin cream, and podophyllin in the treatment of genital warts. Sex Transm Infect. 2003;79:270–5.
Ormerod AD, van Voorst Vader PC, Majewski S, et al. Evaluation of the efficacy, safety, and tolerability of 3 dose regimens of topical sodium nitrite with citric acid in patients with anogenital warts: a randomized clinical trial. JAMA Dermatol. 2015;151:854–61.
Stockfleth E, Beti H, Orasan R, et al. Topical Polyphenon® E in the treatment of external genital and perianal warts: a randomized controlled trial. Br J Dermatol. 2008;158:1329–38.
Syed TA, Cheema KM, Khayyami M, et al. Human leukocyte interferon-alpha versus podophyllotoxin in cream for the treatment of genital warts in males. A placebo-controlled, double-blind, comparative study. Dermatol Basel Switz. 1995;191:129–32
Gross G, Meyer KG, Pres H, Tatet al. A randomized, double-blind, four-arm parallel-group, placebo-controlled phase II/III study to investigate the clinical efficacy of two galenic formulations of Polyphenon E in the treatment of external genital warts. J Eur Acad Dermatol Venereol. 2007;21:1404–12
Tatti S, Swinehart JM, Thielert C, et al. Sinecatechins, a defined green tea extract, in the treatment of external anogenital warts: a randomized controlled trial. Obstet Gynecol. 2008;111:1371–9.
von Krogh G, Szpak E, Andersson M, et al. Self-treatment using 0.25–0.50% podophyllotoxin-ethanol solutions against penile condylomata acuminata: a placebo-controlled comparative study. Genitourin Med. 1994;70:105–9
Bilensoy EA, Moroy PB, Çirpanli YA, et al. A double-blind placebo-controlled study of 5-fluorouracil: cyclodextrin complex loaded thermosensitive gel for the treatment of HPV induced condyloma. J Incl Phenom Macrocycl Chem. 2011;69:309–13.
Akhavan S, Mohammadi SR, Modarres Gillani M, et al. Efficacy of combination therapy of oral zinc sulfate with imiquimod, podophyllin or cryotherapy in the treatment of vulvar warts. J Obstet Gynaecol Res. 2014;40:2110–3.
Relakis K, Cardamakis E, Korantzis A, et al. Treatment of men with flat (FC) or acuminata (CA) condylomata with interferon alpha-2a. Eur J Gynaecol Oncol. 1996;17:529–33.
Schöfer HA, V/van Ophoven AB, Henke UA, et al. Randomized, comparative trial on the sustained efficacy of topical imiquimod 5% cream versus conventional ablative methods in external anogenital warts. Eur J Dermatol. 2006;16:642–8
Stone KM, Becker TM, Hadgu A, et al. Treatment of external genital warts: a randomised clinical trial comparing podophyllin, cryotherapy, and electrodesiccation. Genitourin Med. 1990;66:16–9.
Swinehart JM, Sperling M, Philips S, et al. Intralesional fluorouracil/epinephrine injectable gel for treatment of condylomata acuminata. Arch Dermatol. 1997;133:67–73.
Arican O, Guneri F, Bilgic K, et al. Topical imiquimod 5% cream in external anogenital warts: a randomized, double-blind, placebo-controlled study. J Dermatol. 2004;31:627–31.
Azizjalali M, Ghaffarpour G, Mousavifard B. CO2 laser therapy versus cryotherapy in treatment of genital warts; a randomized controlled trial (RCT). Iran J Microbiol. 2012;4:187–90.
Benedetti Panici P, Scambia G, Baiocchi G, et al. Randomized clinical trial comparing systemic interferon with diathermocoagulation in primary multiple and widespread anogenital condyloma. Obstet Gynecol. 1989;74:393–7.
Beutner KR, Conant MA, Friedman-Kien AE, et al. Patient-applied podofilox for treatment of genital warts. Lancet. 1989;1:831–4.
Bornstein J, Pascal B, Zarfati D, et al. Recombinant human interferon-beta for condylomata acuminata: a randomized, double-blind, placebo-controlled study of intralesional therapy. Int J STD AIDS. 1997;8:614–21.
Camargo CLdA, Belda WJr, Fagundes LJ, et al. A prospective, open, comparative study of 5% potassium hydroxide solution versus cryotherapy in the treatment of genital warts in men. An Bras Dermatol. 2014;89:236–41
Carpiniello VL, Malloy TR, Sedlacek TV, et al. Results of carbon dioxide laser therapy and topical 5-fluorouracil treatment for subclinical condyloma found by magnified penile surface scanning. J Urol. 1988;140:53–4.
Chen K, Chang BZ, Ju M, et al. Comparative study of photodynamic therapy vs CO2 laser vaporization in treatment of condylomata acuminata: a randomized clinical trial. Br J Dermatol. 2007;156:516–20.
Duus BR, Philipsen T, Christensen JD, et al. Refractory condylomata acuminata: a controlled clinical trial of carbon dioxide laser versus conventional surgical treatment. Genitourin Med. 1985;61:59–61.
Eron LJ, Alder MB, O’Rourke JM, et al. Recurrence of condylomata acuminata following cryotherapy is not prevented by systemically administered interferon. Genitourin Med. 1993;69:91–3.
Gabriel G, Thin RN. Treatment of anogenital warts. Comparison of trichloracetic acid and podophyllin versus podophyllin alone. Br J Vener Dis. 1983;59:124–6
Gilson RJC, Ross J, Maw R, et al. A multicentre, randomised, double-blind, placebo controlled study of cryotherapy versus cryotherapy and podophyllotoxin cream as treatment for external anogenital warts. Sex Transm Infect. 2009;85:514–9.
Godley MJ, Bradbeer CS, Gellan M, et al. Cryotherapy compared with trichloroacetic acid in treating genital warts. Genitourin Med. 1987;63:390–2.
Greenberg MD, Rutledge LH, Reid R, et al. A double-blind, randomized trial of 0.5% podofilox and placebo for the treatment of genital warts in women. Obstet Gynecol. 1991;77:735–9
Hellberg D, Svarrer T, Nilsson S, et al. Self-treatment of female external genital warts with 0.5% podophyllotoxin cream (Condyline) vs weekly applications of 20% podophyllin solution. Int J STD AIDS. 1995;6:257–61
Işik S, Koca R, Sarici G, et al. A comparison of a 5% potassium hydroxide solution with a 5-fluorouracil and salicylic acid combination in the treatment of patients with anogenital warts: a randomized, open-label clinical trial. Int J Dermatol. 2014;53:1145–50.
Jensen SL. Comparison of podophyllin application with simple surgical excision in clearance and recurrence of perianal condylomata acuminata. Lancet. 1985;2:1146–8.
Khawaja HT. Podophyllin versus scissor excision in the treatment of perianal condylomata acuminata: a prospective study. Br J Surg. 1989;76:1067–8.
Kinghorn GR, McMillan A, Mulcahy F, et al. An open, comparative, study of the efficacy of 0.5% podophyllotoxin lotion and 25% podophyllotoxin solution in the treatment of condylomata acuminata in males and females. Int J STD AIDS. 1993;4:194–9
Kirby P, Dunne A, King DH, et al. Double-blind randomized clinical trial of self-administered podofilox solution versus vehicle in the treatment of genital warts. Am J Med. 1990;88:465–9.
Kumar P, Dar L, Saldiwal S, et al. Intralesional injection of Mycobacterium w vaccine vs imiquimod, 5%, cream in patients with anogenital warts: a randomized clinical trial. JAMA Dermatol. 2014;150:1072–8.
Lassus A. Comparison of podophyllotoxin and podophyllin in treatment of genital warts. Lancet Lond Engl. 1987;2:512–3.
Lotfabadi P, Maleki F, Gholami A, et al. Liquid nitrogen cryotherapy versus 70% trichloroacetic acid in the treatment of anogenital warts: a randomized controlled trial. Iran J Dermatol. 2015;18:151–5.
Nath D, Kumar B, Sharma VK, et al. Comparison of podophyllin and trichloroacetic acid for the treatment of genital warts. Indian J Dermatol Venereol Leprol. 1990;56:22–4.
Padhiar BB, Karia UK, Aggarwal R, et al. A comparative study of efficacy of imiquimod 5% versus podophyllin 20% in treatment of external and genital warts (60 patients). Indian J Sex Transm Dis. 2006;27:671–9
Petersen CS, Agner T, Ottevanger V, et al. A single-blind study of podophyllotoxin cream 0.5% and podophyllotoxin solution 0.5% in male patients with genital warts. Genitourin Med. 1995;71:391–2
Snoeck R, Bossens M, Parent D, et al. Phase II double-blind, placebo-controlled study of the safety and efficacy of cidofovir topical gel for the treatment of patients with human papillomavirus infection. Clin Infect Dis. 2001;33:597–602.
Stefanaki C, Katzouranis I, Lagogianni E, et al. Comparison of cryotherapy to imiquimod 5% in the treatment of anogenital warts. Int J STD AIDS. 2008;19:441–4.
Syed TA, Lundin S, Ahmad SA. Topical 0.3% and 0.5% podophyllotoxin cream for self-treatment of condylomata acuminata in women. A placebo-controlled, double-blind study. Dermatol Basel Switz. 1994;189:142–5
Szeimies RM, Schleyer V, Moll I, et al. Adjuvant photodynamic therapy does not prevent recurrence of condylomata acuminata after carbon dioxide laser ablation-a phase III, prospective, randomized, bicentric, double-blind study. Dermatol Surg. 2009;35:757–64.
Tabari S, Javadian M, Barat S. The efficacy of podophylin 20% and tricholoroacetic acid %30 in the treatment of genital wart. Casp J Intern Med. 2010;1:16–9.
Tyring S, Edwards L, Cherry LK, et al. Safety and efficacy of 0.5% podofilox gel in the treatment of anogenital warts. Arch Dermatol. 1998;134:33–8
von Krogh G, Hellberg D. Self-treatment using a 0.5% podophyllotoxin cream of external genital condylomata acuminata in women. A placebo-controlled, double-blind study. Sex Transm Dis. 1992;19:170–4
Wallin J. 5-Fluorouracil in the treatment of penile and urethral condylomata acuminata. Br J Vener Dis. 1977;53:240–3.
Bertolotti A, Milpied B, Fouéré S, Cabié A, Dupin N, Derancourt C. Local management of anogenital warts in immunocompetent adults: systematic review and pooled analysis of randomized-controlled trial data. J Am Acad Dermatol. 2019;81:1203–4.
Ao C, Xie J, Wang L, et al. 5-aminolevulinic acid photodynamic therapy for anal canal condyloma acuminatum: a series of 19 cases and literature review. Photodiagnosis Photodyn Ther. 2018;23:230–4.
Yang Y, Zhang Y, Zou X, Guo X, Lin H. Perspective clinical study on effect of 5-aminolevulinic acid photodynamic therapy (ALA-PDT) in treating condylomata acuminata in pregnancy. Photodiagnosis Photodyn Ther 2018;pii:S1572–1000(18)30271–0
Winer RL, Kiviat NB, Hughes JP, et al. Development and duration of human papillomavirus lesions, after initial infection. J Infect Dis. 2005;191:731–8.
Arima Y, Winer RL, Feng Q, et al. Development of genital warts after incident detection of human papillomavirus infection in young men. J Infect Dis. 2010;202:1181–4.
Acknowledgements
We would like to thank Prof. Rodolphe Thiebaut for his continuous support, our research librarian Evelyne Mouillet, the dermatologists of the French Group of Dermato-Infectiology and Sexually Transmitted Diseases of the Société Française de Dermatologie and the Association des Dermatologues des Alpes du Sud, and our copy editor Arianne Dorval.
Funding
This study was supported by grants from the “Allocation jeunes chercheurs hospitaliers” 2015 and the “Programme Hospitalier de Recherche Clinique Interrégional” (No. 13 069). The journal’s Rapid Service Fee was funded by the Department of Research and Innovation of the Centre Hospitalier Universitaire de La Réunion.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
Christian Derancourt, Brigitte Milpied, and Nicolas Dupin conceptualized and designed the study. Antoine Bertolotti, Christian Derancourt, and Cyril Ferdynus participated in the acquisition, analysis, and interpretation of data. Antoine Bertolotti and Christian Derancourt drafted the initial manuscript. Laetitia Huiart, Nicolas Dupin, and Brigitte Milpied critically reviewed the manuscript. All authors read and approved the final manuscript.
Disclosures
Antoine Bertolotti, Cyril Ferdynus, Brigitte Milpied, Nicolas Dupin, Laetitia Huiart and Christian Derancourt have nothing to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Data Availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced Digital Features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.11604663.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Bertolotti, A., Ferdynus, C., Milpied, B. et al. Local Management of Anogenital Warts in Non-Immunocompromised Adults: A Network Meta-Analysis of Randomized Controlled Trials. Dermatol Ther (Heidelb) 10, 249–262 (2020). https://doi.org/10.1007/s13555-020-00357-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-020-00357-z