Abstract
Introduction
Cutaneous body image (CBI) is a construct encompassing how individuals perceive their hair, skin, and nails. Negative CBI has been related to negative psychological outcomes and body image concerns. The first aim of our study was to further validate CBI as a construct. Second, as individuals with dermatologic conditions are at an increased risk for anxiety and depression, the study examined CBI as a mediator of the relationships between having a skin condition and anxiety and depression.
Methods
A convenience sample of clinical participants with dermatologist-validated diagnoses of psoriasis, atopic dermatitis, or acne who were currently taking systemic medication (n = 128) were matched to a sample of comparison participants without skin conditions (n = 128) on self-reported gender, ethnicity, developmental stage, and weight status (body mass index). All participants reported on their CBI, self-esteem (global, appearance-related, and weight-related), body dissatisfaction, drive for thinness, dietary restraint, anxiety, depression, and demographic characteristics.
Results
Cutaneous body image was more negative in those respondents with skin conditions (regression analysis B = − 0.61, standard error 0.23, p = 0.008), demonstrating the criterion-related validity of the measure. CBI was significantly correlated with global (r = 0.39, p < 0.001) and appearance-related self-esteem (r = 0.50, p < 0.001), which establishes convergent validity. CBI was not significantly related to a drive for thinness (r = − 0.12, p = 0.06) or to dietary restraint (r = − 0.05, p = 0.39), supporting discriminant validity. CBI mediated the relationships between having a dermatologic condition and anxiety [point estimate of indirect effect 0.07, 95% confidence interval (CI) 0.02, 0.15] and depression (point estimate of indirect effect 0.04, 95% CI 0.01, 0.08).
Conclusions
The measure of CBI has been further validated. Dermatologists must be aware that various dermatoses may impact patient mental health via the mechanism of negative CBI.
Similar content being viewed by others
Why carry out this study? |
Cutaneous body image (CBI) encompasses how individuals perceive their hair, skin, and nails, and has been related to negative psychological outcomes and body image concerns. |
The first aim of our study was to further validate CBI as a construct. Second, as individuals with dermatologic conditions are at an increased risk for anxiety and depression, the study examined CBI as a mediator of the relationships between having a skin condition and anxiety and depression. |
What was learned from this study? |
The measure of CBI has been further validated. CBI mediates the relationships between having a skin condition and anxiety and depression. |
Dermatologists must be aware that various dermatoses may impact patient mental health via the mechanism of negative CBI. |
Introduction
Cutaneous body image (CBI) is defined as self-evaluative perceptions of the appearance of hair, skin, and nails [1]. Previous research using the only available measure of CBI revealed that patients suffering from skin conditions have a more negative CBI than those who are not [1], thus reinforcing the criterion-related validity of this CBI measure. In that study, the associations between CBI, body dissatisfaction, and drive for thinness were examined, with the results showing that body dissatisfaction predicted CBI [1]. Thus, convergent validity was supported. To date, the discriminant validity of the measure of CBI has not been examined.
People with skin conditions are at risk for internalizing problems [2, 3]. Negative CBI is related to negative psychological outcomes, including anxiety, depression, feelings of inadequacy or inferiority when compared to others, and suicidal ideation [2,3,4]. However, CBI as a mediator of the relationship between having a skin condition and mental health outcomes has not been explored in previous research. Doing so may better explain the link between skin conditions and poor mental health and provide physicians with an important understanding to intervene with patients.
The current study had two aims. The first was to further examine the construct validity of the only available measure of CBI. As a test of criterion-related validity, it was hypothesized that comparison participants would have more positive CBI than dermatology patients, as found in prior studies [1]. As a demonstration of convergent validity, it was hypothesized that CBI would relate to global self-esteem, appearance-related self-esteem, and body dissatisfaction. It is likely that CBI will be related to these self-related constructs because past research suggests that individuals at greater risk of negative CBI, including those suffering from dermatological conditions, also experience low self-esteem [2, 5, 6]. One reason for this low self-esteem may be that people with negative CBI are confronted with how their skin looks on a daily basis, which might impact overall self-assessments. This is particularly relevant when appearance-related self-esteem is considered. Continued exposure to their skin, a very noticeable feature, is likely to impact how people feel about their appearance. As a demonstration of discriminant validity, it was hypothesized that CBI would not be related to a drive for thinness, dietary restraint, or weight-related esteem. Although these three issues are related to body image [7, 8], they focus on weight and eating, which seem to be less relevant for perceptions about the skin’s appearance. Thus, CBI is likely to relate only weakly (if at all) to these constructs.
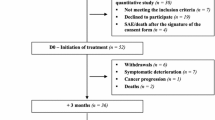
The second aim was to examine CBI as a mediator of the relationships between having a skin condition and associated psychological outcomes (anxiety and depression) and whether these mediations are moderated by gender (Fig. 1). It was hypothesized that CBI would mediate the relationship between having a skin condition and anxiety and depression. While gender was included as a moderator, no gender differences were anticipated.
Methods
Subjects
This study was approved by the institutional review board at the University of Texas at Dallas and was performed in accordance with the Helsinki Declaration of 1964 as revised in 2013. All participants gave written consent prior to participation in the study. All participants were given research exposure credit (university students) or entered into a drawing to win one of two iPad minis (one for each sample) as compensation for their participation. Numeric coding of participant data ensured confidentiality and anonymity.
Clinical participants were recruited from a dermatology teaching clinic at Baylor Scott & White Health in Dallas, Texas. Patients were approached and given the opportunity to participate after their appointment if they had been diagnosed by a dermatologist with acne, atopic dermatitis, or psoriasis and were being treated with systemic oral or injectable medications. In total, 225 patients were approached, of whom 11 declined to participate due to time restrictions. After consent was obtained, clinical participants were weighed. As self-reported height is highly correlated with measured height (r > 0.95), self-reported height was used [9, 10]. Lastly, participants were given the survey to complete at home and return by mail. It was made clear that the researcher was available by phone if they had any questions. If a participant had not returned the survey within 2 weeks, a follow-up phone call was made; if a phone number was unavailable, the participant was emailed by the lead researcher.
A comparison sample of 369 individuals without skin conditions was recruited to match the clinical sample. Participants were recruited using the research exposure credit system at the University of Texas at Dallas and other methods, including word of mouth, online posting on social media websites, and flyers in places where adults spend time (e.g., coffee shops, churches). Comparison participants completed the survey in a research laboratory on the University of Texas at Dallas campus or another location of their choosing after informed consent was obtained. After the participants completed the survey, they were weighed. The researcher or a member of her research staff was present during the survey to address any concerns. For both samples, the study survey was presented in one of five orders (no meaningful order effects were found) and took 20 min to complete.
Clinical and comparison participants were matched based on self-reported gender, ethnicity, developmental stage, and body mass index (BMI). Age was matched using developmental periods of adulthood, as done in prior studies of body image [11]. BMI was matched based on whether participants were classified as underweight (BMI < 18.5), average weight (BMI 18.5–24.9), overweight (BMI 25.0–29.9), or obese (BMI > 30) by the Centers for Disease Control and Prevention guidelines [12].
Measures
Cutaneous Body Image
CBI was assessed using the seven-item Cutaneous Body Image Scale [1]. A composite of all items was created, with lower scores indicating more negative CBI. The measure has shown convergent validity in adults and has been significantly related to the body dissatisfaction subscale of the Eating Disorder Inventory [1]. The measure had good internal consistency in the current study (Cronbach’s α = 0.85).
Global and Appearance-Related Self-Esteem
Global self-esteem (six items) and appearance-related self-esteem (four items) were measured using the respective scales of the previously validated Self-Perception Profile for Adults [13]. Composites were created, such that higher scores indicated higher self-esteem. The measures had good reliability (Cronbach’s α = 0.85, global self-esteem; Cronbach’s α = 0.72, appearance-related self-esteem) in the current study.
Body Dissatisfaction and Drive for Thinness
To measure body dissatisfaction (nine items) and drive for thinness (seven items), the respective subscales of the previously validated Eating Disorder Inventory were used [7]. Composites were created, such that higher scores indicated higher body dissatisfaction and drive for thinness. In the current study, the measures showed good reliability with Cronbach’s α of 0.86 and 0.89 for the body dissatisfaction and drive for thinness subscales, respectively.
Dietary Restraint
Dietary restraint was measured using the previously validated six-item cognitive restraint subscale of the Three Factor Eating Questionnare-R18 [14]. A composite was created, such that higher scores indicated more dietary restraint. The subscale had good reliability in the current study (Cronbach’s α = 0.82).
Weight-Related Esteem
Weight-related esteem was measured with the previously validated eight-item weight subscale of the Body Esteem Scale for Adolescents and Adults [15]. A composite was created, such that higher scores indicated higher weight-related esteem. The reliability of the measure in the current study was high (Cronbach’s α = 0.91).
Anxiety
Anxiety was assessed using the seven-item Generalized Anxiety Disorder Scale [16]. A composite was created, with higher scores indicating more anxiety. The measure had been previously validated [16] and showed strong reliability in the current study (Cronbach’s α = 0.90).
Depression
Depression was assessed using the previously validated Beck Depression Inventory-Short Form [17]. This measure contains an item relating to self-harm and suicide, which was not included in the current study due to ethical concerns. Thus, participants answered 12 questions. A composite was created, with higher scores indicating more severe depression. Reliability of the scale was appropriate in the current study (Cronbach’s α = 0.86).
Demographics
Demographics were collected by requesting participants to complete a questionnaire on their gender, age, height, ethnicity, income, marital status, and educational background, and if they were receiving treatment for acne, atopic dermatitis, psoriasis, or any other skin condition. If they were being treated for a skin condition, participants also were asked to report on the duration of their condition, the method of treatment, the duration of their current treatment, and how effective they thought their treatment was. Participants also indicated if their health was excellent, very good, good, fair, or poor [18]. This single-item measure for health has shown convergent validity with the Medical Outcomes survey Short-Form General Health Survey [18].
Statistical Analyses
The criterion-related validity of CBI was examined using regression analysis. The skin condition group was entered as the predictor of CBI. Convergent and discriminant validity were examined using correlations. To examine whether CBI mediated the relationships between having a skin condition and anxiety and depression, the bootstrapping procedure in the PROCESS macro outlined in Hayes [19] was used to test for moderated mediation. Separate analyses were conducted for anxiety and depression. In both models, CBI served as the mediator, and gender was entered as a moderator. In these analyses, gender (0 = male, 1 = female) and skin condition group (0 = comparison, 1 = clinical) were coded dichotomously. The bootstrapped estimates were found using 1000 random re-samples of the data in an effort to compensate for the possibility of non-normal sampling distributions. All data were analyzed using SPSS software (IBM Corp., Armonk, NY, USA).
Results
Of the initial patient sample, 60% (n = 136) completed their surveys. Comparison matches were only available for 128 of the patients in the clinical sample (67% female, 33% male); 85 patients were diagnosed with psoriasis, 31 with acne, and 12 with atopic dermatitis. A series of one-way analyses of variance did not indicate any statistically significant mean differences between patients with different skin condition diagnoses for any of the variables in the study. Therefore, clinical participants were combined into one group for further analyses. Patients ranged in age from 18 to 78 [mean 42.59, standard deviation (SD) 14.84] years and had a mean BMI of 28.41 (SD 6.91, range 18.14–68.44) kg/m2. All participants rated themselves as being in fair to excellent health aside from their skin.
The final matched comparison sample included 128 participants (67% female, 33% male) who were not undergoing treatment for a skin condition. These individuals ranged in age from 18 to 77 (mean 40.30, SD 14.7) years, and had a mean BMI of 28.58 (SD 7.03, range 17.95–55.78) kg/m2. All participants except for one rated themselves as being in fair to excellent health. The one exception indicated that she rated herself as in poor health due to her body size, but not to other ailments; thus, she was included in the study.
Construct Validity
The regression model examining the criterion-related validity of CBI was significant (Table 1). Having a skin condition significantly predicted more negative CBI, supporting the criterion-related validity of the measure.
The convergent validity of the CBI measure was supported (Table 2). CBI significantly, moderately correlated with global and appearance-related self-esteem (Table 2). The correlation between CBI and body dissatisfaction was close to moderate. CBI was not significantly related to dietary restraint or a drive for thinness, supporting its discriminant validity. CBI was moderately related to weight-related esteem.
The correlations between the items within the CBI scale and the other constructs are examined in Electronic Supplementary Material Table S1.
CBI as a Mediator
For anxiety and depression, CBI mediated the relationship between skin condition group and both of these mental health outcomes. Gender did not moderate these relationships in either instance (Table 3).
Discussion
The results of this study further support the validity of this measure of CBI as well as the utility of this construct. Patients with acne, atopic dermatitis, or psoriasis had a more negative CBI, thereby demonstrating criterion-related validity as patients with skin conditions feel more uncomfortable with their skin. These findings are similar to those reported by Gupta and Gupta [1] who also found that people with a skin condition have a more negative CBI than those who do not.
In the present study, the CBI was moderately related to global and appearance-related self-esteem, and the correlation between CBI and body dissatisfaction was close to moderate. These results demonstrate convergent validity. As the skin is a highly visible portion of the human body, it is not surprising that CBI relates to individuals’ feelings about themselves, and even more so to their feelings about their appearance. Future research should explore the salience of different physical characteristics in an effort to determine a hierarchy of characteristics people value (e.g., skin, hair, thinness, etc.) and how this hierarchy may change in people who have skin conditions (e.g., those with skin conditions may value skin’s appearance over thinness in a way that those without skin conditions do not).
We found that the CBI was not significantly related to dietary restraint or a drive for thinness which demonstrates discriminant validity. It stands to reason that constructs related to how people eat or diet are less likely to affect perceptions of their skin than other more relevant factors like global self-esteem. Weight-related esteem was more strongly related to CBI than expected. One explanation is that weight-related esteem also measures perceptions about a feature of the body and, therefore, weight-related esteem and CBI may be more strongly related than previously believed. Alternatively, this relationship may indicate that skin and weight are more connected than previously considered, as previous research in the psoriasis population has demonstrated [20]. Additionally, individuals who are undergoing treatment for a skin condition are at risk for weight gain or loss due to a host of issues, including gastrointestinal concomitant conditions, with side effects affecting some individuals [21]. Thus, participants in the clinical sample who were currently receiving these forms of therapies were potentially more at risk for weight-related concerns. However, because of the cross-sectional nature of the current study, this could not be examined. Future research should explore how individuals with skin conditions, such as psoriasis, feel about their weight throughout treatment and also explore any impacts weight fluctuations may have on their CBI.
CBI mediated the relationships between suffering from a skin condition and experiencing depression and anxiety. This finding gives credence to the notion that the poor psychological health many people with skin conditions experience may be due in part to their negative feelings about their skin rather than solely due to experiencing a specific skin condition. These relationships were not moderated by gender, indicating that CBI concerns relate to depression and anxiety in a similar fashion in males and females.
There are a number of limitations to this study. Participants were only examined at a single time-point. Future studies should collect longitudinal data over multiple points in time as this approach may yield information on how CBI changes or remains stable over time even when people experience other changes, such as the length of time individuals have had their conditions, environmental changes, or stress. If the conditions are longstanding, patients may have had more time to cope or get used to living with their conditions than those who are newly diagnosed. Alternatively, suffering with a skin condition for a long time could result in increasingly negative CBI because of frustration about a lack of improvement. Skin conditions also respond to the outside environment; for example, cold and dry weather have a negative effect on many individuals’ psoriasis or atopic dermatitis, while for some, the warmth and increased exposure to sunlight in the summer is helpful [22, 23]. In addition, stress is known to play a role in acne, atopic dermatitis, and psoriasis [24,25,26]. Therefore, transient stressors may also impact CBI. By examining CBI over multiple time-points, information can be gathered about whether CBI changes over time as well.
Finally, the number of patients studied was relatively low, and measures in this study were self-reported. Therefore, the relationships that emerged between variables may be a result of shared method variance. However, as CBI and the other measured variables are based on individuals’ perceptions, self-reporting is the most logical way to assess these constructs. Nevertheless, future research could potentially use other methods (i.e., clinical interviews, observations) to examine mental health constructs.
Conclusions
The study has several important strengths and implications. First, this study conducted a broader examination of the validity of CBI as a construct and further supported the measure’s usefulness for future research. Additionally, this study was the first to statistically examine whether CBI may explain some of the previously documented relationships between having a skin condition and poor mental health outcomes [3,4,5]. This research strongly supports the important role that dermatologists can play in improving patient mental health through effective treatments to increase CBI, thereby reducing depression and anxiety in a significant number of patients.
References
Gupta MA, Gupta AK, Johnson AM. Cutaneous body image: empirical validation of a dermatologic construct. J Invest Dermatol. 2004;123(2):405–6.
Fox FE, Rumsey N, Morris M. “Ur skin is the thing that everyone sees and you can’t change it!”: exploring the appearance-related concerns of young people with psoriasis. Dev Neurorehabil. 2007;10(2):133–41.
Picardi A, Lega I, Tarolla E. Suicide risk in skin disorders. Clin Dermatol. 2013;31(1):47–56.
Gupta MA, Gupta AK. Cutaneous body image dissatisfaction and suicidal ideation: mediation by interpersonal sensitivity. J Psychosom Res. 2013;75(1):55–9.
Koo J. The psychosocial impact of acne: patients’ perceptions. J Am Acad Dermatol. 1995;32(5 Pt 3):S26–30.
Schmid-Ott G, Jaeger B, Kuensebeck HW, Ott R, Lamprecht F. Dimensions of stigmatization in patients with psoriasis in a ‘Questionnaire on Experience with Skin Complaints’. Dermatology. 1996;193(4):304–10.
Garner DM, Olmstead MP, Polivy J. Development and validation of a multidimensional eating disorder inventory for anorexia nervosa and bulimia. Int J Eat Disord. 1983;2(2):15–34.
Ricciardelli LA, Tate D, Williams RJ. Body dissatisfaction as a mediator of the relationship between dietary restraint and bulimic eating patterns. Appetite. 1997;29(1):43–54.
Ng SP, Korda R, Clements M, et al. Validity of self-reported height and weight and derived body mass index in middle-aged and elderly individuals in Australia. Aust N Z J Public Health. 2011;35(6):557–63.
Roth LW, Allshouse AA, Lesh J, Polotsky AJ, Santoro N. The correlation between self-reported and measured height, weight, and BMI in reproductive age women. Maturitas. 2013;76(2):185–8.
Augustus-Horvath CL, Tylka TL. The acceptance model of intuitive eating: a comparison of women in emerging adulthood, early adulthood, and middle adulthood. J Couns Psychol. 2011;58(1):110–25.
Centers for Disease Control and Prevention. About BMI for Adults [Internet]. 2017. http://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html. Retrieved 31 Aug 2019.
Harter S, Messer B. Manual for the adult self perception profile. Denver: University of Denver; 1986.
de Lauzon B, Romon M, Deschamps V, et al. The Three-Factor Eating Questionnaire-R18 is able to distinguish among different eating patterns in a general population. J Nutr. 2004;134(9):2372–80.
Mendelson BK, Mendelson MJ, White DR. Body-esteem scale for adolescents and adults. J Pers Assess. 2001;76(1):90–106.
Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7.
Beck AT, Beck RW. Screening depressed patients in family practice. A rapid technic. Postgrad Med. 1972;52(6):81–5.
Cunny KA, Perri M 3rd. Single-item vs multiple-item measures of health-related quality of life. Psychol Rep. 1991;69(1):127–30.
Hayes A. Introduction to mediation, moderation, and conditional process analysis: a regression based approach. New York: The Guilford Press; 2013.
Jensen P, Skov L. Psoriasis and Obesity. Dermatology. 2016;232(6):633–9.
Megna M, Napolitano M, Patruno C, et al. Systemic treatment of adult atopic dermatitis: a review. Dermatol Ther (Heidelb). 2017;7(1):1–23.
Farber EM, Nall ML. The natural history of psoriasis in 5,600 patients. Dermatologica. 1974;148(1):1–18.
Vocks E, Busch R, Fröhlich C, Borelli S, Mayer H, Ring J. Influence of weather and climate on subjective symptom intensity in atopic eczema. Int J Biometeorol. 2001;45(1):27–33.
Ghodsi SZ, Orawa H, Zouboulis CC. Prevalence, severity, and severity risk factors of acne in high school pupils: a community-based study. J Invest Dermatol. 2009;129(9):2136–41.
Senra MS, Wollenberg A. Psychodermatological aspects of atopic dermatitis. Br J Dermatol. 2014;170[Suppl 1]:38–43.
Gupta MA, Gupta AK, Kirkby S, et al. A psychocutaneous profile of psoriasis patients who are stress reactors. A study of 127 patients. Gen Hosp Psychiatry. 1989;11(3):166–73.
Acknowledgements
Funding
This study was supported in part by a dissertation grant from the University of Texas at Dallas, Richardson, TX, USA. No Rapid Service Fee was received by the journal for the publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship of this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Alan Menter is an Editor-in-Chief of this journal. Sarah Hinkley and Shayla Holub have nothing to disclose.
Compliance with Ethics Guidelines
This study was approved by the institutional review board at the University of Texas at Dallas and was performed in accordance with the Helsinki Declaration of 1964 as revised in 2013. All participants gave written consent prior to participation in the study. All participants were given research exposure credit (university students) or entered into a drawing to win one of two iPad minis (one for each sample) as compensation for their participation. Numeric coding of participant data ensured confidentiality and anonymity.
Data Availability
The dataset generated during and/or analyzed during the current study is available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced Digital Features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.11498820.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Hinkley, S.B., Holub, S.C. & Menter, A. The Validity of Cutaneous Body Image as a Construct and as a Mediator of the Relationship Between Cutaneous Disease and Mental Health. Dermatol Ther (Heidelb) 10, 203–211 (2020). https://doi.org/10.1007/s13555-020-00351-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-020-00351-5