Abstract
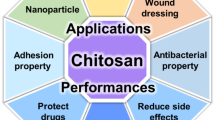
Neglected tropical diseases (NTDs) are a diverse group of infections which are difficult to prevent or control, affecting impoverished communities that are unique to tropical or subtropical regions. In spite of the low number of drugs that are currently used for the treatment of these diseases, progress on new drug discovery and development for NTDs is still very limited. Therefore, strategies on the development of new delivery systems for current drugs have been the main focus of formulators to provide improved efficacy and safety. In recent years, particulate delivery systems at micro- and nanosize, including polymeric micro- and nanoparticles, liposomes, solid lipid nanoparticles, metallic nanoparticles, and nanoemulsions, have been widely investigated in the treatment and control of NTDs. Among these polymers used for the preparation of such systems is chitosan, which is a marine biopolymer obtained from the shells of crustaceans. Chitosan has been investigated as a delivery system due to the versatility of its physicochemical properties as well as bioadhesive and penetration-enhancing properties. Furthermore, chitosan can be also used to improve treatment due to its bioactive properties such as antimicrobial, tissue regeneration, etc. In this review, after giving a brief introduction to neglected diseases and particulate systems developed for the treatment and control of NTDs, the chitosan-based systems will be described in more detail and the recent studies on these systems will be reviewed.

Graphical abstract


Similar content being viewed by others
References
WHO-Department of control of neglected tropical diseases. A road map for neglected tropical diseases 2021–2030, ending the neglect to attain the sustainable development goals 2020; WHO/UCN/NTD/2020.01; WHO: Geneva. https://www.who.int/neglected_diseases/diseases/en/; (accessed on 20 March 2020).
WHO-Department of control of neglected tropical diseases. A road map for neglected tropical diseases 2021–2030, ending the neglect to attain the sustainable development goals 2020; WHO/UCN/NTD/2020.01; WHO: Geneva; 15 May 2020.
WHO. Global update on implementation of preventive chemotherapy against neglected tropical diseases in 2018. Wkly Epidemiol Rec. 2019;38(94):425–40.
Date AA, Joshi MD, Patravale VB. Parasitic diseases: liposomes and polymeric nanoparticles versus lipid nanoparticles. Adv Drug Deliv Rev. 2007;59(6):505–21. https://doi.org/10.1016/j.addr.2007.04.009.
Islan GA, Durán M, Cacicedo ML, Nakazato G, Kobayashi RKT, Martinez DST, et al. Nanopharmaceuticals as a solution to neglected diseases: is it possible? Acta Trop. 2017;170:16–42. https://doi.org/10.1016/j.actatropica.2017.02.019.
Romero EL, Morilla MJ. Nanotechnological approaches against Chagas disease. Adv Drug Deliv Rev. 2010;62(4–5):576–88. https://doi.org/10.1016/j.addr.2009.11.025.
Akbari M, Oryan A, Hatam G. Application of nanotechnology in treatment of leishmaniasis: a review. Acta Trop. 2017;172:86–90. https://doi.org/10.1016/j.actatropica.2017.04.029.
De Souza A, Marins DSS, Mathias SL, Monteiro LM, Yukuyama MN, Scarim CB, et al. Promising nanotherapy in treating leishmaniasis. Int J Pharm. 2018;547(1–2):421–31. https://doi.org/10.1016/j.ijpharm.2018.06.018.
Walvekar P, Gannimani R, Govender T. Combination drug therapy via nanocarriers against infectious diseases. Eur J Pharm Sci. 2019;127:121–41. https://doi.org/10.1016/j.ejps.2018.10.017.
Pund S, Joshi A. Nanoarchitectures for neglected tropical protozoal diseases: challenges and state of the art. In: Grumezescu AM, editor. Nano- and microscale drug delivery systems: Elsevier; 2017;439–80. https://doi.org/10.1016/B978-0-323-52727-9.00023-6.
Rafati S, Gholami E, Zahedifard F. Delivery systems for Leishmania vaccine development. Expert Rev Vaccines. 2016;15(7):879–95. https://doi.org/10.1586/14760584.2016.1157478.
Volpedo G, Costa L, Ryan N, Halsey G, Satoskar A, Oghumu S. Nanoparticulate drug delivery systems for the treatment of neglected tropical protozoan diseases. J Venom Anim Toxins. 2019;25. https://doi.org/10.1590/1678-9199-jvatitd-1441-18.
CDC. Buruli ulcer. https://www.cdc.gov/buruli-ulcer/index.html; (accessed on 20 March 2020).
WHO. Buruli ulcer (Mycobacterium ulcerans infection). https://www.who.int/news-room/fact-sheets/detail/buruli-ulcer-(mycobacterium-ulcerans-infection); (accessed on 20 March 2020).
WHO. Prevent dengue & chikungunya. WHO Myanmar newsletter special. 2019.
FDA. Dengvaxia. https://www.fda.gov/vaccines-blood-biologics/dengvaxia; (accessed on 20 March 2020).
CDC. Chagas disease. https://www.cdc.gov/parasites/chagas/; (accessed on 20 March 2020).
WHO. Chagas disease (American trypanosomiasis). https://www.who.int/news-room/fact-sheets/detail/chagas-disease-(american-trypanosomiasis); (accessed on 20 March 2020).
WHO. Dracunculiasis (guinea-worm disease). https://www.who.int/news-room/fact-sheets/detail/dracunculiasis-(guinea-worm-disease); (accessed on 20 March 2020).
WHO. Echinococcosis. https://www.who.int/news-room/fact-sheets/detail/echinococcosis; (accessed on 20 March 2020).
CDC. Parasites-echinococcosis. https://www.cdc.gov/parasites/echinococcosis/; (accessed on 20 March 2020).
WHO. Foodborne trematodiases. https://www.who.int/news-room/fact-sheets/detail/foodborne-trematodiases; (accessed on 20 March 2020).
WHO. Trypanosomiasis, human African (sleeping sickness). https://www.who.int/news-room/fact-sheets/detail/trypanosomiasis-human-african-(sleeping-sickness); (accessed on 20 March 2020).
WHO. Leishmaniasis. https://www.who.int/news-room/fact-sheets/detail/leishmaniasis; (accessed on 20 March 2020).
CDC. Leishmaniasis. https://www.cdc.gov/parasites/leishmaniasis/; (accessed on 20 March 2020).
WHO. Leprosy. https://www.who.int/news-room/fact-sheets/detail/leprosy; (accessed on 20 March 2020).
WHO. Leprosy elimination. https://www.who.int/lep/disease/treatment/en/; (accessed on 20 March 2020).
WHO. Lymphatic filariasis. https://www.who.int/news-room/fact-sheets/detail/lymphatic-filariasis; (accessed on 20 March 2020).
WHO. Mycetoma, chromoblastomycosis and other deep mycoses. https://www.who.int/neglected_diseases/diseases/mycetoma-chromoblastomycosis-deep-mycoses/en/; (accessed on 20 March 2020).
WHO. Onchocerciasis. https://www.who.int/news-room/fact-sheets/detail/onchocerciasis; (accessed on 20 March 2020).
WHO. Rabies. https://www.who.int/ith/vaccines/rabies/en/; (accessed on 20 March 2020).
WHO. Scabies and other ectoparasites. https://www.who.int/neglected_diseases/diseases/scabies-and-other-ectoparasites/en/; (accessed 24 March 2020).
CDC. Scabies medication. https://www.cdc.gov/parasites/scabies/health_professionals/meds.html; (accessed on 20 March 2020).
WHO. Schistosomiasis. https://www.who.int/news-room/fact-sheets/detail/schistosomiasis; (accessed on 20 March 2020).
CDC. Parasites - soil-transmitted helminths. https://www.cdc.gov/parasites/sth/index.html; (accessed on 20 March 2020).
WHO. Soil-transmitted helminth infections. https://www.who.int/news-room/fact-sheets/detail/soil-transmitted-helminth-infections; (accessed on 20 March 2020).
WHO. Snakebite envenoming. https://www.who.int/snakebites/disease/en/; (accessed on 20 March 2020).
WHO. Taeniasis/cysticercosis. https://www.who.int/news-room/fact-sheets/detail/taeniasis-cysticercosis; (accessed on 20 March 2020).
WHO. Trachoma. https://www.who.int/news-room/fact-sheets/detail/trachoma; (accessed on 20 March 2020).
WHO. Yaws eradication. https://www.who.int/yaws/en/; (accessed on 20 March 2020).
Gregoriadis G, Florence AT. Liposomes in drug delivery. Drugs. 1993;45:15–28. https://doi.org/10.2165/00003495-199345010-00003.
Akbarzadeh A, Rezaei-Sadabady R, Davaran S, Joo SW, Zarghami N, Hanifehpour Y, et al. Liposome: classification, preparation, and applications. Nanoscale Res Lett. 2013;8:102. https://doi.org/10.1186/1556-276x-8-102.
Gregoriadis G, Perrie Y. Liposomes. In: Encyclopedia of Life Sciences (ELS). JohnWiley & Sons, Ltd: Chicheste; 2010r. https://doi.org/10.1002/9780470015902.a0002656.pub2.
Lovelyn C. Current state of nanoemulsions in drug delivery. JBNB. 2011;2:626–39. https://doi.org/10.4236/jbnb.2011.225075.
Jaiswal M, Dudhe R, Sharma PK. Nanoemulsion: an advanced mode of drug delivery system. 3 Biotech. 2015;5:123–7. https://doi.org/10.1007/s13205-014-0214-0.
Aliabadi HM, Lavasanifar A. Polymeric micelles for drug delivery. Expert Opin Drug Deliv. 2006;3(1):139–62. https://doi.org/10.1517/17425247.3.1.139.
Croy SR, Kwon GS. Polymeric micelles for drug delivery. Curr Pharm Des. 2006;12(36):4669–84. https://doi.org/10.2174/138161206779026245.
Kumari A, Yadav SK, Yadav SC. Biodegradable polymeric nanoparticles based drug delivery systems. Colloids Surf B. 2010;75(1):1–18. https://doi.org/10.1016/j.colsurfb.2009.09.001.
Elsabahy M, Wooley KL. Design of polymeric nanoparticles for biomedical delivery applications. Chem Soc Rev. 2012;41(7):2545. https://doi.org/10.1039/c2cs15327k.
Banik BL, Fattahi P, Brown JL. Polymeric nanoparticles: the future of nanomedicine. WIREs Nanomed Nanobiotechnol. 2015;8:n/a-n/a. https://doi.org/10.1002/wnan.1364.
Arvizo RR, Bhattacharyya S, Kudgus RA, Giri K, Bhattacharya R, Mukherjee P. Intrinsic therapeutic applications of noble metal nanoparticles: past, present and future. Chem Soc Rev. 2012;41(7):2943. https://doi.org/10.1039/c2cs15355f.
Kazi KM, Mandal AS, Biswas N, Guha A, Chatterjee S, Behera M, et al. Niosome: a future of targeted drug delivery systems. J Adv Pharm Technol Res. 2010;1(4):374–80. https://doi.org/10.4103/0110-5558.76435.
Yadav N, Khatak S, Sara UVS. Solid lipid nanoparticles - a review. Int J App Pharm. 2013;5(2):8–18.
Ghasemiyeh P, Mohammadi-Samani S. Solid lipid nanoparticles and nanostructured lipid carriers as novel drug delivery systems: applications, advantages and disadvantages. Res Pharm Sci. 2018;13(4):288–303. https://doi.org/10.4103/1735-5362.235156.
Emerich DF, Thanos CG. Nanotechnology and medicine. Expert Opin Biol Ther. 2003;3(4):655–63. https://doi.org/10.1517/14712598.3.4.655.
Duran N, Marcato PD, Teixeira Z, Duran M, Costa FTM, Brocchi M. State of the art of nanobiotechnology applications in neglected diseases. Curr Nanosci. 2009;5:396–408. https://doi.org/10.2174/157341309789378069.
Tomiotto-Pellissier F, Miranda-Sapla MM, Machado LF, Bortoleti BTDS, Sahd CS, Chagas AF, et al. Nanotechnology as a potential therapeutic alternative for schistosomiasis. Acta Trop. 2017;174:64–71. https://doi.org/10.1016/j.actatropica.2017.06.025.
Shah A, Gupta SS. Anti-leishmanial nanotherapeutics: a current perspective. Curr Drug Metab. 2019;20(6):473–82. https://doi.org/10.2174/1389200219666181022163424.
Sun Y, Chen D, Pan Y, Qu W, Hao H, Wang X, et al. Nanoparticles for antiparasitic drug delivery. Drug Deliv. 2019;26(1):1206–21. https://doi.org/10.1080/10717544.2019.1692968.
Singh M, Chakrapani A, O'Hagan D. Nanoparticles and microparticles as vaccine-delivery systems. Expert Rev Vaccines. 2007;6(5):797–808. https://doi.org/10.1586/14760584.6.5.797.
De Temmerman ML, Rejman J, Demeester J, Irvine DJ, Gander B, De Smedt SC. Particulate vaccines: on the quest for optimal delivery and immune response. Drug Discov Today. 2011;16(13–14):569–82. https://doi.org/10.1016/j.drudis.2011.04.006.
Lebre F, Hearnden CH, Lavelle EC. Modulation of immune responses by particulate materials. Adv Mater. 2016;28:5525–41 https://doi.org/10.1002/adma.201505395.
Roberts GAF. Chitin chemistry. New York: Macmillan Education; 1992.
Peniche C, Argüelles-Monal W, Goycoolea FM. Chapter 25 - chitin and chitosan: major sources, properties and applications. In: Belgacem MN, Gandini A, editors. Monomers, polymers and composites from renewable resources. Amsterdam: Elsevier; 2008. p. 517–42.
Younes I, Rinaudo M. Chitin and chitosan preparation from marine sources. Structure, properties and applications. Mar Drugs. 2015;13(3):1133–74. https://doi.org/10.3390/md13031133.
Roberts GAF. Thirty years of progress in chitin and chitosan. Prog Chem Appl Chitin. 2008;13:7–15 http://ptchit.lodz.pl/PTChit/13_01.pdf.
Basa S, Nampally M, Honorato T, Das SN, Podile AR, El Gueddari NE, et al. The pattern of acetylation defines the priming activity of chitosan tetramers. J Am Chem Soc. 2020;142(4):1975–86. https://doi.org/10.1021/jacs.9b11466.
Weinhold MX, Sauvageau JCM, Kumirska J, Thöming J. Studies on acetylation patterns of different chitosan preparations. Carbohydr Polym. 2009;78(4):678–84. https://doi.org/10.1016/j.carbpol.2009.06.001.
European Pharmacopoeia 9th edition: Monograph 1774; Council of European: Strasbourg, France; 2016.
The United States Pharmacopeia/The National Formulary 42/NF37; United States Pharmacopeial Convention: Rockville (MD); 2019: pp. 5663.
Şenel S. Current status and future of chitosan in drug and vaccine delivery. React Funct Polym. 2019;147:104452. https://doi.org/10.1016/j.reactfunctpolym.2019.104452.
Kean T, Roth S, Thanou M. Trimethylated chitosans as non-viral gene delivery vectors: cytotoxicity and transfection efficiency. J Control Release. 2005;103:643–53. https://doi.org/10.1016/j.jconrel.2005.01.001.
Kean T, Thanou M. Biodegradation, biodistribution and toxicity of chitosan. Adv Drug Deliv Rev. 2010;62(1):3–11. https://doi.org/10.1016/j.addr.2009.09.004.
Lim SM, Song DK, Oh SH, Lee-Yoon DS, Bae EH, Lee JH. In vitro and in vivo degradation behavior of acetylated chitosan porous beads. J Biomater Sci Polym Ed. 2008;19(4):453–66. https://doi.org/10.1163/156856208783719482.
Sashiwa H. Chemical aspects of chitin and chitosan derivatives. In: Kim SK, editor. Chitin and chitosan derivatives: advances in drug discovery and developments. Boca Raton: CRC, Taylor &Francis Group; 2014. p. 93–111.
Mourya VK, Inamdar NN, Choudhari YM. Chitooligosaccharides: synthesis, characterization and applications. Polym Sci. 2011;53(7):583–612. https://doi.org/10.1134/s0965545x11070066.
Lodhi G, Kim Y-S, Hwang J-W, Kim S-K, Jeon Y-J, Je J-Y, et al. Chitooligosaccharide and its derivatives: preparation and biological applications. Biomed Res Int. 2014;2014:654913. https://doi.org/10.1155/2014/654913.
Ruiz GAM, Corrales HFZ. Chitosan, chitosan derivatives and their biomedical applications. In: Shalaby EA (Ed)r: Biological Activities and Application of Marine Polysaccharides. Rijeka, Croatia: InTech; 2017. pp: 87-106. https://doi.org/10.5772/66527.
Zhao D, Yu S, Sun B, Gao S, Guo S, Zhao K. Biomedical applications of chitosan and its derivative nanoparticles. Polymers. 2018;10(4):462. https://doi.org/10.3390/polym10040462.
Sayın B, Şenel S. Chitosan and its derivatives for mucosal immunization. In: Jayakumar R, Prabaharan M, editors. Current research and developments on chitin and chitosan in biomaterials science; 2008. p. 145–65.
Sayın B, Somavarapu S, Li XW, Thanou M, Sesardic D, Alpar HO, et al. Mono-N-carboxymethyl chitosan (MCC) and N-trimethyl chitosan (TMC) nanoparticles for non-invasive vaccine delivery. Int J Pharm. 2008;363(1–2):139–48. https://doi.org/10.1016/j.ijpharm.2008.06.029.
Sayın B, Somavarapu S, Li XW, Sesardic D, Şenel S, Alpar OH. TMC-MCC (N-trimethyl chitosan-mono-N-carboxymethyl chitosan) nanocomplexes for mucosal delivery of vaccines. Eur J Pharm Sci. 2009;38(4):362–9. https://doi.org/10.1016/j.ejps.2009.08.010.
Wang W, Meng Q, Li Q, Liu J, Zhou M, Jin Z, et al. Chitosan derivatives and their application in biomedicine. Int J Mol Sci. 2020;21(2):487. https://doi.org/10.3390/ijms21020487.
Liu H, Wang C, Li C, Qin Y, Wang Z, Yang F, et al. A functional chitosan-based hydrogel as a wound dressing and drug delivery system in the treatment of wound healing. RSC Adv. 2018;8(14):7533–49. https://doi.org/10.1039/c7ra13510f.
Naseri M, Akbarzadeh A, Spotin A, Akbari NAR, Mahami-Oskouei M, Ahmadpour E. Scolicidal and apoptotic activities of albendazole sulfoxide and albendazole sulfoxide-loaded PLGA-PEG as a novel nanopolymeric particle against Echinococcus granulosus protoscoleces. Parasitol Res. 2016;115:4595–603. https://doi.org/10.1007/s00436-016-5250-8.
Dai T, Tanaka M, Huang Y-Y, Hamblin MR. Chitosan preparations for wounds and burns: antimicrobial and wound-healing effects. Expert Rev Anti-Infect Ther. 2011;9(7):857–79. https://doi.org/10.1586/eri.11.59.
Şenel S, McClure SJ. Potential applications of chitosan in veterinary medicine. Adv Drug Deliv Rev. 2004;56(10):1467–80. https://doi.org/10.1016/j.addr.2004.02.007.
Şenel S. Potential applications of chitosan in oral mucosal delivery. J Drug Del Sci Tech. 2010;20(1):23–32. https://doi.org/10.1016/S1773-2247(10)50003-0.
Kim J, Cai Z, Lee HS, Choi GS, Lee DH, Jo C. Preparation and characterization of a bacterial cellulose/chitosan composite for potential biomedical application. J Polym Res. 2011;18:739–44. https://doi.org/10.1007/s10965-010-9470-9.
Akca G, Özdemir A, Öner ZG, Şenel S. Comparison of different types and sources of chitosan for the treatment of infections in the oral cavity. Res Chem Intermed. 2018;44:4811–25. https://doi.org/10.1007/s11164-018-3338-8.
Akıncıbay H, Şenel S, Ay ZY. Application of chitosan gel in the treatment of chronic periodontitis. J Biomed Mater Res B Appl Biomater. 2007;80(2):290–6. https://doi.org/10.1002/jbm.b.30596.
Boynueğri D, Özcan G, Şenel S, Uç D, Uraz A, Ögüs E, et al. Clinical and radiographic evaluations of chitosan gel in periodontal intraosseous defects: a pilot study. J Biomed Mater Res B Appl Biomater. 2009;90B:461–6. https://doi.org/10.1002/jbm.b.31307.
Martin L, Wilson CG, Koosha F, Tetley L, Gray AI, Şenel S, et al. The release of model macromolecules may be controlled by the hydrophobicity of palmitoyl glycol chitosan hydrogels. J Control Release. 2002;80(1–3):87–100. https://doi.org/10.1016/s0168-3659(02)00005-6.
Özmeriç N, Özcan G, Haytaç CM, Alaaddinoğlu EE, Sargon MF, Şenel S. Chitosan film enriched with an antioxidant agent, taurine, in fenestration defects. J Biomed Mater Res. 2000;51(3):500–3. https://doi.org/10.1002/1097-4636(20000905)51:3<500::AID-JBM26>3.0.CO;2-P.
Zubareva A, Ily'Ina A, Prokhorov A, Kurek D, Efremov M, Varlamov V, et al. Characterization of protein and peptide binding to nanogels formed by differently charged chitosan derivatives. Molecules. 2013;18(7):7848–64. https://doi.org/10.3390/molecules18077848.
Azeran NSB, Zazali NDB, Timur SS, Özdogan AI, Ekizoglu M, Sheshala R, et al. Moxifloxacin loaded chitosan gel formulations for the treatment of periodontal diseases. J Polym Mater. 2017;34(1):157–69.
Şenel S, İkinci G, Kaş S, Yousefi-Rad A, Sargon MF, Hıncal AA. Chitosan films and hydrogels of chlorhexidine gluconate for oral mucosal delivery. Int J Pharm. 2000;193(2):197–203. https://doi.org/10.1016/s0378-5173(99)00334-8.
Sandri G, Rossi S, Ferrari F, Bonferoni MC, Muzzarelli C, Caramella C. Assessment of chitosan derivatives as buccal and vaginal penetration enhancers. Eur J Pharm Sci. 2004;21(2–3):351–9. https://doi.org/10.1016/j.ejps.2003.10.028.
Netsomboon K, Bernkop-Schnürch A. Mucoadhesive vs. mucopenetrating particulate drug delivery. Eur J Pharm Biopharm. 2016;98:76–89. https://doi.org/10.1016/j.ejpb.2015.11.003.
Şenel S, Kremer MJ, Kaş S, Wertz PW, Hıncal AA, Squier CA. Enhancing effect of chitosan on peptide drug delivery across buccal mucosa. Biomaterials. 2000;21(20):2067–71. https://doi.org/10.1016/s0142-9612(00)00134-4.
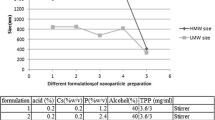
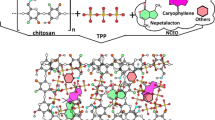
Tokumitsu H, Ichikawa H, Fukumori Y. Chitosan-gadopentetic acid complex nanoparticles for gadolinium neutron-capture therapy of cancer: preparation by novel emulsion-droplet coalescence technique and characterization. Pharm Res. 1999;16:1830–5. https://doi.org/10.1023/a:1018995124527.
Calvo P, Remunan-Lopez C, Vila-Jato JL, Alonso MJ. Novel hydrophilic chitosan-polyethylene oxide nanoparticles as protein carriers. J Appl Polym Sci. 1997;63(1):125–32. https://doi.org/10.1002/(SICI)1097-4628(19970103)63:1<125::AID-APP13>3.0.CO;2-4.
Sarmento B, Martins S, Ribeiro A, Veiga F, Neufeld R, Ferreira D. Development and comparison of different nanoparticulate polyelectrolyte complexes as insulin carriers. Int J Pept Res Ther. 2006;12(2):131–8. https://doi.org/10.1007/s10989-005-9010-3.
El-Shabouri MH. Positively charged nanoparticles for improving the oral bioavailability of cyclosporin-A. Int J Pharm. 2002;249(1–2):101–8. https://doi.org/10.1016/s0378-5173(02)00461-1.
Mitra S, Gaur U, Ghosh PC, Maitra AN. Tumour targeted delivery of encapsulated dextran-doxorubicin conjugate using chitosan nanoparticles as carrier. J Control Release. 2001;74(1–3):317–23. https://doi.org/10.1016/s0168-3659(01)00342-x.
Tian XX, Groves MJ. Formulation and biological activity of antineoplastic proteoglycans derived from Mycobacterium vaccae in chitosan nanoparticles. J Pharm Pharmacol. 1999;51(2):151–7. https://doi.org/10.1211/0022357991772268.
Ohya Y, Shiratani M, Kobayashi H, Ouchi T. Release behavior of 5-fluorouracil from chitosan-gel nanospheres immobilizing 5-fluorouracil coated with polysaccharides and their cell specific cytotoxicity. J Macromol Sci A. 1994;31(5):629–42. https://doi.org/10.1080/10601329409349743.
Grenha A. Chitosan nanoparticles: a survey of preparation methods. J Drug Target. 2012;20(4):291–300. https://doi.org/10.3109/1061186x.2011.654121.
Liu C, Tan Y, Liu C, Chen X, Yu L. Preparations, characterizations and applications of chitosan-based nanoparticles. J Ocean U China. 2007;6(3):237–43. https://doi.org/10.1007/s11802-007-0237-9.
Lee JW, Park JH, Robinson JR. Bioadhesive-based dosage forms: the next generation. J Pharm Sci. 2000;89(7):850–66. https://doi.org/10.1002/1520-6017(200007)89:7.
Peppas N, Huang Y. Nanoscale technology of mucoadhesive interaction. Adv Drug Deliv Rev. 2004;56:1675–87. https://doi.org/10.1016/j.addr.2004.03.001.
Luessen HL, de Leeuw BJ, Langemeyer MW, de Boer AB, Verhoef JC, Junginger HE. Mucoadhesive polymers in peroral peptide drug delivery. VI. Carbomer and chitosan improve the intestinal absorption of the peptide drug buserelin in vivo. Pharm Res. 1996;13(11):1668–72. https://doi.org/10.1023/a:1016488623022.
Furda I. Reduction of absorption of dietary lipids and cholesterol by chitosan and its derivatives and special formulations. In: Muzzareilli RAA, editor. Chitosan per os: from dietary supplement to drug carrier. Grottammare: Atec; 2000. p. 41–63.
Thanou M, Verhoef JC, Junginger HE. Oral drug absorption enhancement by chitosan and its derivatives. Adv Drug Deliv Rev. 2001;52(2):117–26. https://doi.org/10.1016/s0169-409x(01)00231-9.
Sonia TA, Sharma CP. Chitosan and its derivatives for drug delivery perspective. In: Jayakumar R, Prabaharan M, Muzzarelli RAA, editors. Chitosan for biomaterials I. Berlin: Springer; 2011. p. 23–53.
Bernkop-Schnürch A, Dünnhaupt S. Chitosan-based drug delivery systems. Eur J Pharm Sci. 2012;81(3):463–9. https://doi.org/10.1016/j.ejpb.2012.04.007.
Singh PK, Pawar VK, Jaiswal AK, Singh Y, Srikanth CH, Chaurasia M, et al. Chitosan coated PluronicF127 micelles for effective delivery of amphotericin B in experimental visceral leishmaniasis. Int J Biol Macromol. 2017;105(1):1220–31. https://doi.org/10.1016/j.ijbiomac.2017.07.161.
Jain V, Gupta A, Pawar VK, Asthana S, Jaiswal AK, Dube A, et al. Chitosan-assisted immunotherapy for intervention of experimental leishmaniasis via amphotericin B-loaded solid lipid nanoparticles. Appl Biochem Biotechnol. 2014;174:1309–30. https://doi.org/10.1007/s12010-014-1084-y.
Gupta PK, Asthana S, Jaiswal AK, Kumar V, Verma AK, Shukla P, et al. Exploitation of lectinized lipo-polymerosome encapsulated amphotericin B to target macrophages for effective chemotherapy of visceral leishmaniasis. Bioconjug Chem. 2014;25(6):1091–102. https://doi.org/10.1021/bc500087h.
Vemireddy S, Preethi Pallavi MC, Sampath Kumar Halmuthur M. Chitosan stabilized nasal emulsion delivery system for effective humoral and cellular response against recombinant tetravalent dengue antigen. Carbohydr Polym. 2018;190:129–38. https://doi.org/10.1016/j.carbpol.2018.02.073.
Neimert-Andersson T, Binnmyr J, Enoksson M, Langeback J, Zettergren L, Hallgren AC, et al. Evaluation of safety and efficacy as an adjuvant for the chitosan-based vaccine delivery vehicle ViscoGel in a single-blind randomised phase I/IIa clinical trial. Vaccine. 2014;32(45):5967–74. https://doi.org/10.1016/j.vaccine.2014.08.057.
Arca HC, Günbeyaz M, Şenel S. Chitosan-based systems for the delivery of vaccine antigens. Expert Rev Vaccines. 2009;8(7):937–53. https://doi.org/10.1586/erv.09.47.
Şenel S. Chitosan-based particulate systems for non-invasive vaccine delivery. In: Jayakumar R, Prabaharan M, RAA M, editors. Advances in polymer sciences. Berlin: Springer; 2011. p. 111–37.
Çokçalışkan C, Özyörük F, Gürsoy RN, Alkan M, Günbeyaz M, Arca HÇ, et al. Chitosan-based systems for intranasal immunization against foot-and-mouth disease. Pharm Dev Technol. 2014;19(2):181–8. https://doi.org/10.3109/10837450.2013.763263.
Huo Z, Sinha R, McNeela EA, Borrow R, Giemza R, Cosgrove C, et al. Induction of protective serum meningococcal bactericidal and diphtheria-neutralizing antibodies and mucosal immunoglobulin a in volunteers by nasal insufflations of the Neisseria meningitidis serogroup C polysaccharide-CRM197 conjugate vaccine mixed with chitosan. Infect Immun. 2005;73(12):8256–65. https://doi.org/10.1128/IAI.73.12.8256-8265.2005.
Zaharoff DA, Rogers CJ, Hance KW, Schlom J, Greiner JW. Chitosan solution enhances both humoral and cell-mediated immune responses to subcutaneous vaccination. Vaccine. 2007;25(11):2085–94. https://doi.org/10.1016/j.vaccine.2006.11.034.
McNeela EA, Jabbal-Gill I, Illum L, Pizza M, Rappuoli R, Podda A, et al. Intranasal immunization with genetically detoxified diphtheria toxin induces T cell responses in humans: enhancement of Th2 responses and toxin-neutralizing antibodies by formulation with chitosan. Vaccine. 2004;22(8):909–14. https://doi.org/10.1016/j.vaccine.2003.09.012.
Read RC, Naylor SC, Potter CW, Bond J, Jabbal-Gill I, Fisher A, et al. Effective nasal influenza vaccine delivery using chitosan. Vaccine. 2005;23(35):4367–74. https://doi.org/10.1016/j.vaccine.2005.04.021.
Atmar RL, Bernstein DI, Harro CD, Al-Ibrahim MS, Chen WH, Ferreira J, et al. Norovirus vaccine against experimental human Norwalk virus illness. N Engl J Med. 2011;365(23):2178–87. https://doi.org/10.1056/nejmoa1101245.
Yüksel S, Pekcan M, Puralı N, Esendağlı G, Tavukçuoğlu E, Rivero-Arredondo V, et al. Development and in vitro evaluation of a new adjuvant system containing Salmonella Typhi porins and chitosan. Int J Pharm. 2020;578:119129. https://doi.org/10.1016/j.ijpharm.2020.119129.
Peluso G, Petillo O, Ranieri M, Santin M, Ambrosio L, Calabro D, et al. Chitosan-mediated stimulation of macrophage function. Biomaterials. 1994;15(15):1215–20. https://doi.org/10.1016/0142-9612(94)90272-0.
Nishimura K, Nishimura S, Nishi N, Saiki I, Tokura S, Azuma I. Immunological activity of chitin and its derivatives. Vaccine. 1984;2(1):93–9. https://doi.org/10.1016/s0264-410x(98)90039-1.
Carroll EC, Jin L, Mori A, Munoz-Wolf N, Oleszycka E, Moran HBT, et al. The vaccine adjuvant chitosan promotes cellular immunity via DNA sensor cGAS-STING-dependent induction of type I interferons. Immunity. 2016;44(3):597–608. https://doi.org/10.1016/j.immuni.2016.02.004.
Scherließ R, Buske S, Young K, Weber B, Rades T, Hook S. In vivo evaluation of chitosan as an adjuvant in subcutaneous vaccine formulations. Vaccine. 2013;31(42):4812–9. https://doi.org/10.1016/j.vaccine.2013.07.081.
Moran HBT, Turley JL, Andersson M, Lavelle EC. Immunomodulatory properties of chitosan polymers. Biomaterials. 2018;184:1–9. https://doi.org/10.1016/j.biomaterials.2018.08.054.
Ravindranathan S, Koppolu B, Smith S, Zaharoff D. Effect of chitosan properties on immunoreactivity. Mar Drugs. 2016;14(5):91. https://doi.org/10.3390/md14050091.
Ragelle H, Vandermeulen G, Préat V. Chitosan-based siRNA delivery systems. J Control Release. 2013;172(1):207–18. https://doi.org/10.1016/j.jconrel.2013.08.005.
Şenel S, Aksoy EA, Akca G. Application of chitosan based scaffolds for drug delivery and tissue engineering in dentistry. In: Choi A, Ben-Nissan B, editors. Marine-derived biomaterials for tissue engineering applications. Springer Series in biomaterials science and engineering, vol. 14. Singapore: Springer; 2019. p. 157–78. https://doi.org/10.1007/978-981-13-8855-2_8.
Li P, Poon YF, Li W, Zhu H-Y, Yeap SH, Cao Y, et al. A polycationic antimicrobial and biocompatible hydrogel with microbe membrane suctioning ability. Nat Mater. 2011;10:149–56. https://doi.org/10.1038/nmat2915.
Andres Y, Giraud L, Gerente C, Le Cloirec P. Antibacterial effects of chitosan powder: mechanisms of action. Environ Technol. 2007;28(12):1357–63. https://doi.org/10.1080/09593332808618893.
Raafat D, Von Bargen K, Haas A, Sahl HG. Insights into the mode of action of chitosan as an antibacterial compound. Appl Environ Microbiol. 2008;74(12):3764–73. https://doi.org/10.1128/aem.00453-08.
Rabea EI, Badawy ME, Stevens CV, Smagghe G, Steurbaut W. Chitosan as antimicrobial agent: applications and mode of action. Biomacromolecules. 2003;4(6):1457–65. https://doi.org/10.1021/bm034130m.
Kong M, Chen XG, Xing K, Park HJ. Antimicrobial properties of chitosan and mode of action: a state of the art review. Int J Food Microbiol. 2010;144(1):51–63. https://doi.org/10.1016/j.ijfoodmicro.2010.09.012.
Prudden JF, Migel P, Hanson P, Friedrich L, Balassa L. The discovery of a potent pure chemical wound-healing accelerator. Am J Surg. 1970;119(5):560–4. https://doi.org/10.1016/0002-9610(70)90175-3.
Muzzarelli RA, Mattioli-Belmonte M, Pugnaloni A, Biagini G. Biochemistry, histology and clinical uses of chitins and chitosans in wound healing. In: Jolles P, Muzzarelli RA, editors. Chitin and chitinases. 1st ed. Basel: Birkhäuser; 1999. p. 251–64.
Ueno H, Nakamura F, Murakami M, Okumura M, Kadosawa T, Fujinaga T. Evaluation effects of chitosan for the extracellular matrix production by fibroblasts and the growth factors production by macrophages. Biomaterials. 2001;22(15):2125–30. https://doi.org/10.1016/s0142-9612(00)00401-4.
Suzuki Y. Influence of physico-chemical properties of chitin and chitosan on complement activation. Carbohydr Polym. 2000;42(3):307–10. https://doi.org/10.1016/s0144-8617(99)00161-7.
Ueno H, Mori T, Fujinaga T. Topical formulations and wound healing applications of chitosan. Adv Drug Deliv Rev. 2001;52(2):105–15. https://doi.org/10.1016/s0169-409x(01)00189-2.
Hu Z, Zhang D-Y, Lu S-T, Li P-W, Li S-D. Chitosan-based composite materials for prospective hemostatic applications. Mar Drugs. 2018;16(8). https://doi.org/10.3390/md16080273.
WHO. Dengue and severe dengue. https://www.who.int/news-room/fact-sheets/detail/dengue-and-severe-dengue; (accessed 24 March 2020).
Sanofi. Dengue. https://www.sanofi.com/en/your-health/vaccines/dengue; (accessed 24 March 2020).
Hunsawong T, Sunintaboon P, Warit S, Thaisomboonsuk B, Jarman RG, Yoon I-K, et al. Immunogenic properties of a BCG adjuvanted chitosan nanoparticle-based dengue vaccine in human dendritic cells. PLoS Negl Trop Dis. 2015;9(9):e0003958. https://doi.org/10.1371/journal.pntd.0003958.
Hunsawong T, Sunintaboon P, Warit S, Thaisomboonsuk B, Jarman RG, Yoon I-K, et al. A novel dengue virus serotype-2 nanovaccine induces robust humoral and cell-mediated immunity in mice. Vaccine. 2015;33(14):1702–10. https://doi.org/10.1016/j.vaccine.2015.02.016.
Nantachit N, Sunintaboon P, Ubol S. EDIII-DENV3 nanospheres drive immature dendritic cells into a mature phenotype in an in vitro model. Microbiol Immunol. 2017;61:305–17. https://doi.org/10.1111/1348-0421.12497.
Nantachit N, Sunintaboon P, Ubol S. Responses of primary human nasal epithelial cells to EDIII-DENV stimulation: the first step to intranasal dengue vaccination. Virol J. 2016;13:142. https://doi.org/10.1186/s12985-016-0598-z.
Izaguirre-Hernandez IY, Mellado-Sanchez G, Mondragon-Vasquez K, Thomas-Dupont P, Sanchez-Vargas LA, Hernandez-Flores KG, et al. Non-conjugated chitosan-based nanoparticles to proteic antigens elicit similar humoral immune responses to those obtained with alum. J Nanosci Nanotechnol. 2017;17(1):846–52. https://doi.org/10.1166/jnn.2017.13067.
Cavalcanti IT, Silva BVM, Peres NG, Moura P, Sotomayor MDPT, Guedes MIF, et al. A disposable chitosan-modified carbon fiber electrode for dengue virus envelope protein detection. Talanta. 2012;91:41–6. https://doi.org/10.1016/j.talanta.2012.01.002.
Leonardi D, Salomón CJ, Lamas MC, Olivieri AC. Development of novel formulations for Chagas’ disease: optimization of benznidazole chitosan microparticles based on artificial neural networks. Int J Pharm. 2009;367(1–2):140–7. https://doi.org/10.1016/j.ijpharm.2008.09.036.
Nhavene EPF, Da Silva WM, Trivelato Junior RR, Gastelois PL, Venâncio T, Nascimento R, et al. Chitosan grafted into mesoporous silica nanoparticles as benznidazol carrier for Chagas diseases treatment. Microporous Mesoporous Mater. 2018;272:265–75. https://doi.org/10.1016/j.micromeso.2018.06.035.
Vespa GN, Cunha FQ, Silva JS. Nitric oxide is involved in control of Trypanosoma cruzi-induced parasitemia and directly kills the parasite in vitro. Infect Immun. 1994;62(11):5177–82.
Seabra AB, Durán N. Chapter 2 - nitric oxide donors for treating neglected diseases. In: Seabra AB, editor. Nitric oxide donors. London: Academic; 2017. p. 25–53.
Gutierrez FR, Mineo TW, Pavanelli WR, Guedes PM, Silva JS. The effects of nitric oxide on the immune system during Trypanosoma cruzi infection. Mem Inst Oswaldo Cruz. 2009;104:236–45. https://doi.org/10.1590/s0074-02762009000900030.
Seabra AB, Kitice NA, Pelegrino MT, Lancheros CAC, Yamauchi LM, Pinge-Filho P, et al. Nitric oxide-releasing polymeric nanoparticles against Trypanosoma cruzi. J Phys Conf Ser. 2015;617:012020. https://doi.org/10.1088/1742-6596/617/1/012020.
Contreras Lancheros CA, Pelegrino MT, Kian D, Tavares ER, Hiraiwa PM, Goldenberg S, et al. Selective antiprotozoal activity of nitric oxide-releasing chitosan nanoparticles against Trypanosoma cruzi: toxicity and mechanisms of action. Curr Pharm Des. 2018;24(7):830–9. https://doi.org/10.2174/1381612824666180209105625.
WHO. Echinococcosis. https://www.who.int/news-room/fact-sheets/detail/echinococcosis; (accessed 02 December 2019).
Torabi N, Dobakhti F, Faghihzadeh S, Haniloo A. In vitro and in vivo effects of chitosan-praziquantel and chitosan-albendazole nanoparticles on Echinococcus granulosus Metacestodes. Parasitol Res. 2018;117:2015–23. https://doi.org/10.1007/s00436-018-5849-z.
Liu Y, Wang X-Q, Ren W-X, Chen Y-L, Yu Y, Zhang J-K, et al. Novel albendazole-chitosan nanoparticles for intestinal absorption enhancement and hepatic targeting improvement in rats. J Biomed Mater Res B Appl Biomater. 2013;101B(6):998–1005. https://doi.org/10.1002/jbm.b.32908.
Abulaihaiti M, Wu X-W, Qiao L, Lv H-L, Zhang H-W, Aduwayi N, et al. Efficacy of albendazole-chitosan microsphere-based treatment for alveolar echinococcosis in mice. PLoS Negl Trop Dis. 2015;9(9):e0003950. https://doi.org/10.1371/journal.pntd.0003950.
Araújo C, Leon L. Biological activities of Curcuma longa L. Mem Inst Oswaldo Cruz. 2001;96(5):723–8. https://doi.org/10.1590/s0074-02762001000500026.
Napooni S, Delavari M, Arbabi M, Barkheh H, Rasti S, Hooshyar H, et al. Scolicidal effects of chitosan-curcumin nanoparticles on the hydatid cyst protoscolices. Acta Parasitol. 2019;64:367–75. https://doi.org/10.2478/s11686-019-00054-8.
WHO. Leishmaniasis. https://www.who.int/news-room/fact-sheets/detail/leishmaniasis; (accessed 10 March 2020).
Bahrami S, Esmaeilzadeh S, Zarei M, Ahmadi F. Potential application of nanochitosan film as a therapeutic agent against cutaneous leishmaniasis caused by L. major. Parasitol Res. 2015;114(12):4617–24. https://doi.org/10.1007/s00436-015-4707-5.
Riezk A, Raynes JG, Yardley V, Murdan S, Croft SL. Activity of chitosan and its derivatives against Leishmania major and L. mexicana in vitro. Antimicrob Agents Chemother. 2019;64:e01772–19. https://doi.org/10.1128/aac.01772-19.
Esboei B, Mohebali M, Mousavi P, Fakhar M, Akhoundi B. Potent antileishmanial activity of chitosan against Iranian strain of Leishmania major (MRHO/IR/75/ER): in vitro and in vivo assay. J Vector Borne Dis. 2018;55:111–5. https://doi.org/10.4103/0972-9062.242557.
Abdollahimajd FMH, Dadkhahfar S, Mahdavi H, Mohebali M, Mirzadeh H. Chitosan-based biocompatible dressing for treatment of recalcitrant lesions of cutaneous leishmaniasis: a pilot clinical study. Indian J Dermatol Venereol Leprol. 2019;85:609–14. https://doi.org/10.4103/ijdvl.IJDVL_189_18.
Danesh-Bahreini MASJ, Samiei A, Kamali-Sarvestani E, Barzegar-Jalali M, Mohammadi-Samani S. Nanovaccine for leishmaniasis: preparation of chitosan nanoparticles containing Leishmania superoxide dismutase and evaluation of its immunogenicity in BALB/c mice. Int J Nanomedicine. 2011;6:835–42. https://doi.org/10.2147/ijn.s16805.
Yeganeh F, Barkhordari F, Omidi M, Samiei A, Adeli A, Mahboudi F, et al. Cloning and expression of Leishmania major superoxide dismutase B1: a potential target antigen for serodiagnosis of Leishmaniasis. Iran J Immunol. 2009;6(3):130–40.
Hojatizade M, Soleymani M, Tafaghodi M, Badiee A, Chavoshian O, Jaafari MR. Chitosan nanoparticles loaded with whole and soluble Leishmania antigens, and evaluation of their immunogenecity in a mouse model of leishmaniasis. Iran J Immunol. 2018;15(4):281–93. https://doi.org/10.22034/IJI.2018.39397.
Esfandiari F, Motazedian MH, Asgari Q, Morowvat MH, Molaei M, Heli H. Paromomycin-loaded mannosylated chitosan nanoparticles: synthesis, characterization and targeted drug delivery against leishmaniasis. Acta Trop. 2019;197:105045. https://doi.org/10.1016/j.actatropica.2019.105045.
Chaubey P, Mishra B. Mannose-conjugated chitosan nanoparticles loaded with rifampicin for the treatment of visceral leishmaniasis. Carbohydr Polym. 2014;101:1101–8. https://doi.org/10.1016/j.carbpol.2013.10.044.
Monteiro LM, Lobenberg R, Fotaki N, de Araujo GLB, Cotrim PC, Bou-Chacra N. Co-delivery of buparvaquone and polymyxin B in a nanostructured lipid carrier for leishmaniasis treatment. J Glob Antimicrob Resist. 2019;18:279–83. https://doi.org/10.1016/j.jgar.2019.06.006.
Yamamoto ES, Campos BLS, Jesus JA, Laurenti MD, Ribeiro SP, Kallás EG, et al. The effect of ursolic acid on Leishmania (Leishmania) amazonensis is related to programed cell death and presents therapeutic potential in experimental cutaneous leishmaniasis. PLoS One. 2015;10(12):e0144946. https://doi.org/10.1371/journal.pone.0144946.
Santos-Valle ABC, Souza GRR, Paes CQ, Miyazaki T, Silva AH, Altube MJ, et al. Nanomedicine strategies for addressing major needs in neglected tropical diseases. Annu Rev Control. 2019;48:423–41. https://doi.org/10.1016/j.arcontrol.2019.08.001.
Frézard F, Demicheli C, Da Silva SM, Azevedo EG, Ribeiro RR. ,Nanostructures for improved antimonial therapy of leishmaniasis. In: Grumezescu AM (Ed.) Nano- and Microscale Drug Delivery Systems. Philadelphia, US: Elsevier; 2017. pp. 419–37. https://doi.org/10.1016/B978-0-323-52727-9.00022-4.
Tripathi P, Dwivedi P, Khatik R, Jaiswal AK, Dube A, Shukla P, et al. Development of 4-sulfated N-acetyl galactosamine anchored chitosan nanoparticles: a dual strategy for effective management of leishmaniasis. Colloids Surf B. 2015;136:150–9. https://doi.org/10.1016/j.colsurfb.2015.08.037.
Tan JSL, Roberts C, Billa N. Pharmacokinetics and tissue distribution of an orally administered mucoadhesive chitosan-coated amphotericin B-loaded nanostructured lipid carrier (NLC) in rats. J Biomater Sci Polym Ed. 2020;31(2):141–54. https://doi.org/10.1080/09205063.2019.1680926.
Gupta PK, Jaiswal AK, Kumar V, Verma A, Dwivedi P, Dube A, et al. Covalent functionalized self-assembled lipo-polymerosome bearing amphotericin B for better management of leishmaniasis and its toxicity evaluation. Mol Pharm. 2014;11(3):951–63. https://doi.org/10.1021/mp400603t.
Gupta PK, Jaiswal AK, Asthana S, Verma A, Kumar V, Shukla P, et al. Self assembled ionically sodium alginate cross-linked amphotericin B encapsulated glycol chitosan stearate nanoparticles: applicability in better chemotherapy and non-toxic delivery in visceral leishmaniasis. Pharm Res. 2015;32:1727–40. https://doi.org/10.1007/s11095-014-1571-4.
Shahnaz G, Edagwa BJ, McMillan J, Akhtar S, Raza A, Qureshi NA, et al. Development of mannose-anchored thiolated amphotericin B nanocarriers for treatment of visceral leishmaniasis. Nanomedicine. 2017;12(2):99–115. https://doi.org/10.2217/nnm-2016-0325.
Asthana S, Jaiswal AK, Gupta PK, Pawar VK, Dube A, Chourasia MK. Immunoadjuvant chemotherapy of visceral leishmaniasis in hamsters using amphotericin B-encapsulated nanoemulsion template-based chitosan nanocapsules. Antimicrob Agents Chemother. 2013;57(4):1714–22. https://doi.org/10.1128/aac.01984-12.
Asthana S, Gupta PK, Jaiswal AK, Dube A, Chourasia MK. Overexpressed macrophage mannose receptor targeted nanocapsules-mediated cargo delivery approach for eradication of resident parasite: in vitro and in vivo studies. Pharm Res. 2015;32(8):2663–77. https://doi.org/10.1007/s11095-015-1651-0.
Ribeiro TG, Chávez-Fumagalli MA, Valadares DG, França JR, Rodrigues LB, Duarte MC, et al. Novel targeting using nanoparticles: an approach to the development of an effective anti-leishmanial drug-delivery system. Int J Nanomedicine. 2014;9:877–90. https://doi.org/10.2147/IJN.S55678.
Ribeiro T, Franca J, Fuscaldi L, Santos M, Duarte M, Lage P, et al. An optimized nanoparticle delivery system based on chitosan and chondroitin sulfate molecules reduces the toxicity of amphotericin B and is effective in treating tegumentary leishmaniasis. Int J Nanomedicine. 2014;9:5341–53. https://doi.org/10.2147/ijn.s68966.
Bose PP, Kumar P, Dwivedi MK. Hemoglobin guided nanocarrier for specific delivery of amphotericin B to Leishmania infected macrophage. Acta Trop. 2016;158:148–59. https://doi.org/10.1016/j.actatropica.2016.02.026.
Serrano DR, Lalatsa A, Dea-Ayuela MA, Bilbao-Ramos PE, Garrett NL, Moger J, et al. Oral particle uptake and organ targeting drives the activity of amphotericin B nanoparticles. Mol Pharm. 2015;12(2):420–31. https://doi.org/10.1021/mp500527x.
Cabral FV, Pelegrino MT, Sauter IP, Seabra AB, Cortez M, Ribeiro MS. Nitric oxide-loaded chitosan nanoparticles as an innovative antileishmanial platform. Nitric Oxide. 2019;93:25–33. https://doi.org/10.1016/j.niox.2019.09.007.
Rabia S, Khaleeq N, Batool S, Dar MJ, Kim DW, Din FU, et al. Rifampicin-loaded nanotransferosomal gel for treatment of cutaneous leishmaniasis: passive targeting via topical route. Nanomedicine. 2020;15(2):183–203. https://doi.org/10.2217/nnm-2019-0320.
Moreno E, Schwartz J, Larrea E, Conde I, Font M, Sanmartín C, et al. Assessment of β-lapachone loaded in lecithin-chitosan nanoparticles for the topical treatment of cutaneous leishmaniasis in L. major infected BALB/c mice. Nanomed-Nanotechnol. 2015;11(8):2003–12. https://doi.org/10.1016/j.nano.2015.07.011.
Malli S, Pomel S, Dennemont I, Loiseau PM, Bouchemal K. Combination of amphotericin B and chitosan platelets for the treatment of experimental cutaneous leishmaniasis: histological and immunohistochemical examinations. J Drug Deliv Sci Tec. 2019;50:34–41. https://doi.org/10.1016/j.jddst.2018.12.031.
Malli S, Pomel S, Ayadi Y, Deloménie C, Da Costa A, Loiseau PM, et al. Topically applied chitosan-coated poly (isobutylcyanoacrylate) nanoparticles are active against cutaneous leishmaniasis by accelerating lesion healing and reducing the parasitic load. ACS Appl Bio Mater. 2019;2(6):2573–86. https://doi.org/10.1021/acsabm.9b00263.
Varshosaz J, Arbabi B, Pestehchian N, Saberi S, Delavari M. Chitosan-titanium dioxide-glucantime nanoassemblies effects on promastigote and amastigote of Leishmania major. Int J Biol Macromol. 2018;107:212–21. https://doi.org/10.1016/j.ijbiomac.2017.08.177.
Rafiee A, Riazi-Rad F, Darabi H, Khaze V, Javadian S, Ajdary S, et al. Ferroportin-encapsulated nanoparticles reduce infection and improve immunity in mice infected with Leishmania major. Int J Pharm. 2014;466(1–2):375–81. https://doi.org/10.1016/j.ijpharm.2014.03.039.
WHO. Lymphatic filariasis. https://www.who.int/lymphatic_filariasis/disease/en/; (accessed 24 March 2020).
Ali M, Afzal M, Verma M, Misra-Bhattacharya S, Ahmad FJ, Dinda AK. Improved antifilarial activity of ivermectin in chitosan–alginate nanoparticles against human lymphatic filarial parasite, Brugia malayi. Parasitol Res. 2013;112(8):2933–43. https://doi.org/10.1007/s00436-013-3466-4.
Shukla R, Gupta J, Shukla P, Dwivedi P, Tripathi P, Bhattacharya SM, et al. Chitosan coated alginate micro particles for the oral delivery of antifilarial drugs and combinations for intervention in Brugia malayi induced lymphatic filariasis. RSC Adv. 2015;5:69047–56. https://doi.org/10.1039/C5RA06982C.
Madhumathi J, Prince PR, Anugraha G, Kiran P, Rao DN, Reddy MVR, et al. Identification and characterization of nematode specific protective epitopes of Brugia malayi TRX towards development of synthetic vaccine construct for lymphatic filariasis. Vaccine. 2010;28(31):5038–48. https://doi.org/10.1016/j.vaccine.2010.05.012.
Gregory WF, Atmadja AK, Allen JE, Maizels RM. The abundant larval transcript-1 and -2 genes of Brugia malayi encode stage-specific candidate vaccine antigens for filariasis. Infect Immun. 2000;68(7):4174–9. https://doi.org/10.1128/iai.68.7.4174-4179.2000.
Malathi B, Mona S, Thiyagarajan D, Kaliraj P. Immunopotentiating nano-chitosan as potent vaccine carter for efficacious prophylaxis of filarial antigens. Int J Biol Macromol. 2015;73:131–7. https://doi.org/10.1016/j.ijbiomac.2014.11.014.
Oliveira CR, Rezende CMF, Silva MR, Borges OM, Pêgo AP, Goes AM. Oral vaccination based on DNA-chitosan nanoparticles against Schistosoma mansoni infection. ScientificWorldJournal. 2012;2012:938457. https://doi.org/10.1100/2012/938457.
Oliveira CR, Rezende CMF, Silva MR, Pêgo AP, Borges O, Goes AM. A new strategy based on Smrho protein loaded chitosan nanoparticles as a candidate oral vaccine against schistosomiasis. PLoS Negl Trop Dis. 2012;6(11):e1894. https://doi.org/10.1371/journal.pntd.0001894.
Cambridge CD, Singh SR, Waffo AB, Fairley SJ, Dennis VA. Formulation, characterization, and expression of a recombinant MOMP chlamydia trachomatis DNA vaccine encapsulated in chitosan nanoparticles. Int J Nanomedicine. 2013;8(1):1759–71. https://doi.org/10.2147/ijn.s42723.
Sarwar HS, Sohail MF, Saljoughian N, Rehman AU, Akhtar S, Nadhman A, et al. Design of mannosylated oral amphotericin B nanoformulation: efficacy and safety in visceral leishmaniasis. Artif Cells Nanomed Biotechnol. 2018;46(sup1):521–31. https://doi.org/10.1080/21691401.2018.1430699.
Das S, Ghosh S, De AK, Bera T. Oral delivery of ursolic acid-loaded nanostructured lipid carrier coated with chitosan oligosaccharides: development, characterization, in vitro and in vivo assessment for the therapy of leishmaniasis. Int J Biol Macromol. 2017;102:996–1008. https://doi.org/10.1016/j.ijbiomac.2017.04.098.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Şenel, S., Yüksel, S. Chitosan-based particulate systems for drug and vaccine delivery in the treatment and prevention of neglected tropical diseases. Drug Deliv. and Transl. Res. 10, 1644–1674 (2020). https://doi.org/10.1007/s13346-020-00806-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-020-00806-4