Abstract
Implant-based local drug delivery is a unique surgical therapy with many clinical advantages. Atmospheric pressure plasma is a novel non-thermal surface biotechnology that has only recently been applied in enhancing a surgical implant. We are the first to use this technology to successfully create a dexamethasone-delivery metallic implant. Irrespective of the loaded medication, the surface of this novel implant possesses advantageous material features including homogeneity, hydrophilicity, and optimal roughness. UV-vis spectroscopy revealed much more sustainable drug release compared to the implants produced using simple drug attachment. In addition, our drug-releasing implant was found to have multiple biological benefits. As proven by the ELISA data, this multi-layer drug complex provides differential regulation on the cell apoptosis, as well as pro-osteogenic and anti-inflammatory effects on the peri-implant tissue. Furthermore, using the pathway-specific PCR array, our study discovered 28 and 26 upregulated and downregulated genes during osteogenesis and inflammation on our newly fabricated drug-delivery implant, respectively. The medication-induced change in molecular profile serves as a promising clue for designing future implant-based therapy. Collectively, we present atmospheric pressure plasma as a potent tool for creating a surgical implant-based drug-delivery system, which renders multiple therapeutic potentials.

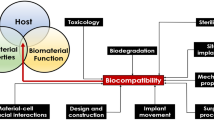
Schematic of the APP-facilitated Dex-delivery implant. This layer-by-layer drug-releasing complex consisted of bottom plasma activation layer, middle medication layer, and top absorbable polymer layer.









Similar content being viewed by others
References
Dimitriadis PA, Farr MR, Allam A, Ray J. Three year experience with the cochlear BAHA attract implant: a systematic review of the literature. BMC Ear Nose Throat Disord. 2016;16:12.
Parithimarkalaignan S, Padmanabhan TV. Osseointegration: an update. J Indian Prosthodont Soc. 2013;13(1):2–6.
Shapiro S, Ramadan J, Cassis A. BAHA skin complications in the pediatric population: systematic review with meta-analysis, otology & neurotology : official publication of the American Otological Society. Otol Neurotol. 2018;39(7):865–73.
Greenhalgh DG. The role of apoptosis in wound healing. Int J Biochem Cell Biol. 1998;30(9):1019–30.
Campos PP, Andrade SP, Moro L, Ferreira MA, Vasconcelos AC. Cellular proliferation, differentiation and apoptosis in polyether-polyurethane sponge implant model in mice. Histol Histopathol. 2006;21(12):1263–70.
Jia H, Wang J, Francois F, Uziel A, Puel JL, Venail F. Molecular and cellular mechanisms of loss of residual hearing after cochlear implantation. Ann Otol Rhinol Laryngol. 2013;122(1):33–9.
Stea S, Visentin M, Granchi D, Cenni E, Ciapetti G, Sudanese A, et al. Apoptosis in peri-implant tissue. Biomaterials. 2000;21(13):1393–8.
Tan F, Walshe P, Viani L, Al-Rubeai M. Surface biotechnology for refining cochlear implants. Trends Biotechnol. 2013;31(12):678–87.
Coutinho AE, Chapman KE. The anti-inflammatory and immunosuppressive effects of glucocorticoids, recent developments and mechanistic insights. Mol Cell Endocrinol. 2011;335(1):2–13.
Park JB. The effects of dexamethasone, ascorbic acid, and beta-glycerophosphate on osteoblastic differentiation by regulating estrogen receptor and osteopontin expression. J Surg Res. 2012;173(1):99–104.
Song IH, Caplan AI, Dennis JE. In vitro dexamethasone pretreatment enhances bone formation of human mesenchymal stem cells in vivo. J Orthop Res. 2009;27(7):916–21.
Wang Q, Wang J, Lu Q, Detamore MS, Berkland C. Injectable PLGA based colloidal gels for zero-order dexamethasone release in cranial defects. Biomaterials. 2010;31(18):4980–6.
Zhong Y, McConnell GC, Ross JD, DeWeerth SP, Bellamkonda RV, A novel dexamethasone-releasing, anti-inflammatory coating for neural implants, Conference Proceedings. 2nd International IEEE EMBS Conference on Neural Engineering, 2005., 2005, pp. 522–525.
Santos A, Sinn Aw M, Bariana M, Kumeria T, Wang Y, Losic D. Drug-releasing implants: current progress, challenges and perspectives. J Mater Chem B. 2014;2(37):6157–82.
Trajkovski B, Petersen A, Strube P, Mehta M, Duda GN. Intra-operatively customized implant coating strategies for local and controlled drug delivery to bone. Adv Drug Deliv Rev. 2012;64(12):1142–51.
Xuereb M, Camilleri J, Attard NJ. Systematic review of current dental implant coating materials and novel coating techniques. Int J Prosthodont. 2015;28(1):51–9.
Heinlin J, Isbary G, Stolz W, Morfill G, Landthaler M, Shimizu T, et al. Plasma applications in medicine with a special focus on dermatology. J Eur Acad Dermatol Venereol. 2011;25(1):1–11.
Metcalfe C, Muzaffar J, Daultrey C, Coulson C. Coblation tonsillectomy: a systematic review and descriptive analysis. Eur Arch Otorhinolaryngol. 2017;274(6):2637–47.
Tan F, O’Neill F, Naciri M, Dowling D, Al-Rubeai M. Cellular and transcriptomic analysis of human mesenchymal stem cell response to plasma-activated hydroxyapatite coating. Acta Biomater. 2012;8(4):1627–38.
Prasad BR, Brook MA, Smith T, Zhao S, Chen Y, Sheardown H, et al. Controlling cellular activity by manipulating silicone surface roughness, colloids and surfaces. Colloids Surf B Biointerfaces. 2010;78(2):237–42.
Dowling DP, Ramamoorthy A, Rahman M, Mooney DA, MacElroy JMD. Influence of atmospheric plasma source and gas composition on the properties of deposited siloxane coatings. Plasma Process Polym. 2009;6(S1):S483–9.
Tynan J, Ward P, Byrne G, Dowling DP. Deposition of biodegradable polycaprolactone coatings using an in-line atmospheric pressure plasma system. Plasma Process Polym. 2009;6(S1):S51–6.
Dowling DP, Maher S, Law VJ, Ardhaoui M, Stallard C, Keenan A. Modified drug release using atmospheric pressure plasma deposited siloxane coatings. J Phys D Appl Phys. 2016;49(36):364005.
Spriano S, Yamaguchi S, Baino F, Ferraris S. A critical review of multifunctional titanium surfaces: new frontiers for improving osseointegration and host response, avoiding bacteria contamination. Acta Biomater. 2018;79:1–22.
Tan F, Naciri M, Dowling D, Al-Rubeai M. In vitro and in vivo bioactivity of CoBlast hydroxyapatite coating and the effect of impaction on its osteoconductivity. Biotechnol Adv. 2012;30(1):352–62.
Dowling DP, Donegan M, Cullen PJ, Law VJ, Milosavljevic V. Importance of plasma thermal energy transfer for plasma jet systems. IEEE Transactions on Plasma Science. 2014;42(10):2426–7.
Stallard CP, Iqbal MM, Turner MM, Dowling DP Investigation of the formation mechanism of aligned nano-structured siloxane coatings deposited using an atmospheric plasma jet Plasma Process Polym 10(10) 2013 n/a-n/a
Breathnach R, McDonnell KA, Chebbi A, Callanan JJ, Dowling DP. Evaluation of the effectiveness of kINPen Med plasma jet and bioactive agent therapy in a rat model of wound healing. Biointerphases. 2018;13(5):051002.
Kokubo T. Bioactive glass ceramics: properties and applications. Biomaterials. 1991;12(2):155–63.
Forouzandeh A, Hesaraki S, Zamanian A. The releasing behavior and in vitro osteoinductive evaluations of dexamethasone-loaded porous calcium phosphate cements. Ceram Int. 2014;40(1):1081–91.
Zhang C, Soori M, Miles FL, Sikes RA, Carson DD, Chung LW, et al. Paracrine factors produced by bone marrow stromal cells induce apoptosis and neuroendocrine differentiation in prostate cancer cells. Prostate. 2011;71(2):157–67.
Chrysis D, Zaman F, Chagin AS, Takigawa M, Savendahl L. Dexamethasone induces apoptosis in proliferative chondrocytes through activation of caspases and suppression of the Akt-phosphatidylinositol 3′-kinase signaling pathway. Endocrinology. 2005;146(3):1391–7.
Tan F, Naciri M, Al-Rubeai M. Osteoconductivity and growth factor production by MG63 osteoblastic cells on bioglass-coated orthopedic implants. Biotechnol Bioeng. 2011;108(2):454–64.
Spano A, Barni S, Sciola L. PMA withdrawal in PMA-treated monocytic THP-1 cells and subsequent retinoic acid stimulation, modulate induction of apoptosis and appearance of dendritic cells. Cell Prolif. 2013;46(3):328–47.
Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(−Delta Delta C(T)) Method. Methods. 2001;25(4):402–8.
Strnad G, Chirila N, Petrovan C, Russu O. Contact angle measurement on medical implant titanium based biomaterials. Procedia Technology. 2016;22:946–53.
Duske K, Koban I, Kindel E, Schroder K, Nebe B, Holtfreter B, et al. Atmospheric plasma enhances wettability and cell spreading on dental implant metals. J Clin Periodontol. 2012;39(4):400–7.
Yang DH, Yoon SJ, Lee DW. Preparation and evaluation of dexamethasone (DEX)/growth and differentiation factor-5 (GDF-5) surface-modified titanium using beta-cyclodextrin-conjugated heparin (CD-Hep) for enhanced osteogenic activity in vitro and in vivo. Int J Mol Sci. 2017;18(8).
Gittens RA, Scheideler L, Rupp F, Hyzy SL, Geis-Gerstorfer J, Schwartz Z, et al. A review on the wettability of dental implant surfaces II: biological and clinical aspects. Acta Biomater. 2014;10(7):2907–18.
Ponsonnet L, Reybier K, Jaffrezic N, Comte V, Lagneau C, Lissac M, et al. Relationship between surface properties (roughness, wettability) of titanium and titanium alloys and cell behaviour. Mater Sci Eng C. 2003;23(4):551–60.
Barry JN, Cowley A, McNally PJ, Dowling DP. Influence of substrate metal alloy type on the properties of hydroxyapatite coatings deposited using a novel ambient temperature deposition technique. J Biomed Mater Res A. 2014;102(3):871–9.
Benzon HT, Chew TL, McCarthy RJ, Benzon HA, Walega DR. Comparison of the particle sizes of different steroids and the effect of dilution: a review of the relative neurotoxicities of the steroids. Anesthesiology. 2007;106(2):331–8.
Faia-Torres AB, Charnley M, Goren T, Guimond-Lischer S, Rottmar M, Maniura-Weber K, et al. Osteogenic differentiation of human mesenchymal stem cells in the absence of osteogenic supplements: a surface-roughness gradient study. Acta Biomater. 2015;28:64–75.
Yang JH, Kim KH, You CK, Rautray TR, Kwon TY. Synthesis of spherical hydroxyapatite granules with interconnected pore channels using camphene emulsion. J Biomed Mater Res B Appl Biomater. 2011;99(1):150–7.
Albrektsson T, Johansson C. Osteoinduction, osteoconduction and osseointegration. Eur Spine J. 2001;10(Suppl 2):S96–101.
Araujo JV, Martins A, Leonor IB, Pinho ED, Reis RL, Neves NM. Surface controlled biomimetic coating of polycaprolactone nanofiber meshes to be used as bone extracellular matrix analogues. J Biomater Sci Polym Ed. 2008;19(10):1261–78.
Chen J, Luo Y, Hong L, Ling Y, Pang J, Fang Y, et al. Synthesis, characterization and osteoconductivity properties of bone fillers based on alendronate-loaded poly(epsilon-caprolactone)/hydroxyapatite microspheres. J Mater Sci Mater Med. 2011;22(3):547–55.
von Woedtke T, Reuter S, Masur K, Weltmann KD. Plasmas for medicine. Phys Rep. 2013;530(4):291–320.
Sarrette J-P, Rouffet B, Ricard A. Determination of nitrogen atoms loss probabilities on copper, aluminium, alumina, brass and nylon surfaces. Plasma Process Polym. 2006;3(2):120–6.
Kesavan K, Pandit JK, Kant S, Muthu MS. Positively charged microemulsions of dexamethasone: comparative effects of two cosurfactants on ocular drug delivery and bioavailability. Ther Deliv. 2013;4(11):1385–95.
Petlin DG, Tverdokhlebov SI, Anissimov YG. Plasma treatment as an efficient tool for controlled drug release from polymeric materials: a review. J Control Release. 2017;266:57–74.
Bhatt S, Pulpytel J, Mirshahi M, Arefi-Khonsari F. Plasma co-polymerized nano coatings—as a biodegradable solid carrier for tunable drug delivery applications. Polymer. 2013;54(18):4820–9.
Yoshida S, Hagiwara K, Hasebe T, Hotta A. Surface modification of polymers by plasma treatments for the enhancement of biocompatibility and controlled drug release. Surf Coat Technol. 2013;233(0):99–107.
Gruver-Yates AL, Cidlowski JA. Tissue-specific actions of glucocorticoids on apoptosis: a double-edged sword. Cells. 2013;2(2):202–23.
Moutsatsou P, Kassi E, Papavassiliou AG. Glucocorticoid receptor signaling in bone cells. Trends Mol Med. 2012;18(6):348–59.
Li H, Qian W, Weng X, Wu Z, Li H, Zhuang Q, et al. Glucocorticoid receptor and sequential P53 activation by dexamethasone mediates apoptosis and cell cycle arrest of osteoblastic MC3T3-E1 cells. PLoS One. 2012;7(6):e37030.
Achuthan A, Aslam ASM, Nguyen Q, Lam PY, Fleetwood AJ, Frye AT, et al. Glucocorticoids promote apoptosis of proinflammatory monocytes by inhibiting ERK activity. Cell Death Dis. 2018;9(3):267.
Zeng S, Qiao H, Lv XW, Fan D, Liu T, Xie D. High-dose dexamethasone induced LPS-stimulated rat alveolar macrophages apoptosis. Drug Des Devel Ther. 2017;11:3097–104.
Ren R, Oakley RH, Cruz-Topete D, Cidlowski JA. Dual role for glucocorticoids in cardiomyocyte hypertrophy and apoptosis. Endocrinology. 2012;153(11):5346–60.
Wen LP, Madani K, Fahrni JA, Duncan SR, Rosen GD. Dexamethasone inhibits lung epithelial cell apoptosis induced by IFN-gamma and Fas. Am J Phys. 1997;273(5):L921–9.
Smith LK, Cidlowski JA. Glucocorticoid-induced apoptosis of healthy and malignant lymphocytes. Prog Brain Res. 2010;182:1–30.
Gross KL, Oakley RH, Scoltock AB, Jewell CM, Cidlowski JA. Glucocorticoid receptor alpha isoform-selective regulation of antiapoptotic genes in osteosarcoma cells: a new mechanism for glucocorticoid resistance. Mol Endocrinol. 2011;25(7):1087–99.
Werner SB, Tessler J, Guglielmotti MB, Cabrini RL. Effect of dexamethasone on osseointegration: a preliminary experimental study. J Oral Implantol. 1996;22(3–4):216–9.
Schinke T, Karsenty G. Transcriptional control of osteoblast differentiation and function. In: Bilezikian JP, Raisz LG, Martin TJ, editors. Principles of bone biology. San Diego: Academic Press; 2008. p. 109–19.
Setzer B, Bachle M, Metzger MC, Kohal RJ. The gene-expression and phenotypic response of hFOB 1.19 osteoblasts to surface-modified titanium and zirconia. Biomaterials. 2009;30(6):979–90.
Duarte PM, Serrao CR, Miranda TS, Zanatta LC, Bastos MF, Faveri M, et al. Could cytokine levels in the peri-implant crevicular fluid be used to distinguish between healthy implants and implants with peri-implantitis? A systematic review. J Periodontal Res. 2016;51(6):689–98.
Gabay C. Interleukin-6 and chronic inflammation. Arthritis Res Ther. 2006;8(Suppl 2):S3.
Tanaka T, Narazaki M, Kishimoto T. IL-6 in inflammation, immunity, and disease. Cold Spring Harb Perspect Biol. 2014;6(10):a016295.
Kzhyshkowska J, Gudima A, Riabov V, Dollinger C, Lavalle P, Vrana NE. Macrophage responses to implants: prospects for personalized medicine. J Leukoc Biol. 2015;98(6):953–62.
Barbosa Saliba J, Vieira L, Fernandes-Cunha GM, Rodrigues Da Silva G, Ligorio Fialho S, Silva-Cunha A, et al. Anti-inflammatory effect of dexamethasone controlled released from anterior suprachoroidal polyurethane implants on endotoxin-induced uveitis in rats. Invest Ophthalmol Vis Sci. 2016;57(4):1671–9.
Bruderer M, Richards RG, Alini M, Stoddart MJ. Role and regulation of RUNX2 in osteogenesis. Eur Cell Mater. 2014;28:269–86.
Na Y, Heo SJ, Kim SK, Koak JY. Implant surface treatments affect gene expression of Runx2, osteogenic key marker. J Adv Prosthodont. 2009;1(2):91–6.
Schneider GB, Zaharias R, Seabold D, Keller J, Stanford C. Differentiation of preosteoblasts is affected by implant surface microtopographies. J Biomed Mater Res A. 2004;69(3):462–8.
Hata K, Ikebe K, Wada M, Nokubi T. Osteoblast response to titanium regulates transcriptional activity of Runx2 through MAPK pathway. J Biomed Mater Res A. 2007;81(2):446–52.
Phillips JE, Gersbach CA, Wojtowicz AM, Garcia AJ. Glucocorticoid-induced osteogenesis is negatively regulated by Runx2/Cbfa1 serine phosphorylation. J Cell Sci. 2006;119(Pt 3):581–91.
Sinha KM, Zhou X. Genetic and molecular control of osterix in skeletal formation. J Cell Biochem. 2013;114(5):975–84.
Tu Q, Valverde P, Li S, Zhang J, Yang P, Chen J. Osterix overexpression in mesenchymal stem cells stimulates healing of critical-sized defects in murine calvarial bone. Tissue Eng. 2007;13(10):2431–40.
Tu Q, Valverde P, Chen J. Osterix enhances proliferation and osteogenic potential of bone marrow stromal cells. Biochem Biophys Res Commun. 2006;341(4):1257–65.
Rashid H, Ma C, Chen H, Wang H, Hassan MQ, Sinha K, et al. Sp7 and Runx2 molecular complex synergistically regulate expression of target genes. Connect Tissue Res. 2014;55(Suppl 1):83–7.
Schneider H, Sedaghati B, Naumann A, Hacker MC, Schulz-Siegmund M. Gene silencing of chordin improves BMP-2 effects on osteogenic differentiation of human adipose tissue-derived stromal cells. Tissue Eng A. 2014;20(1–2):335–45.
Dinarello CA. Overview of the IL-1 family in innate inflammation and acquired immunity. Immunol Rev. 2018;281(1):8–27.
Hallab NJ, Jacobs JJ. Chemokines associated with pathologic responses to orthopedic implant debris. Front Endocrinol. 2017;8:5.
McHugh J. Long-term safety of canakinumab in systemic JIA. Nat Rev Rheumatol. 2018;14(11):622.
Menten P, Wuyts A, Van Damme J. Macrophage inflammatory protein-1. Cytokine Growth Factor Rev. 2002;13(6):455–81.
Dapunt U, Maurer S, Giese T, Gaida MM, Hansch GM. The macrophage inflammatory proteins MIP1alpha (CCL3) and MIP2alpha (CXCL2) in implant-associated osteomyelitis: linking inflammation to bone degradation. Mediat Inflamm. 2014;2014:728619.
Varma TK, Toliver-Kinsky TE, Lin CY, Koutrouvelis AP, Nichols JE, Sherwood ER. Cellular mechanisms that cause suppressed gamma interferon secretion in endotoxin-tolerant mice. Infect Immun. 2001;69(9):5249–63.
Schierano G, Bellone G, Cassarino E, Pagano M, Preti G, Emanuelli G. Transforming growth factor-beta and interleukin 10 in oral implant sites in humans. J Dent Res. 2003;82(6):428–32.
Asadullah K, Sterry W, Volk HD. Interleukin-10 therapy—review of a new approach. Pharmacol Rev. 2003;55(2):241–69.
Acknowledgments
The authors wish to thank Professor Denis Dowling in UCD Centre for Biomedical Engineering and experts in the National Centre for Plasma Science & Technology.
Funding
This work was sponsored by the Shanghai Pujiang Program (project no. 19PJ1408800). It was initiated by Science Foundation Ireland and Shanghai East Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
No informed consent or animal studies were used in this study.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tan, F., Al-Rubeai, M. A multifunctional dexamethasone-delivery implant fabricated using atmospheric plasma and its effects on apoptosis, osteogenesis and inflammation. Drug Deliv. and Transl. Res. 11, 86–102 (2021). https://doi.org/10.1007/s13346-019-00700-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-019-00700-8