Abstract
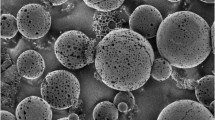
This work was aimed to tune solid matrices for bevacizumab (BVZ) subconjunctival or intravitreal administration in order to prolong drug release, to reduce the number of applications and consequently the side effects. Matrices, with sizes suitable for intravitreal or subconjunctival administration, based on hydroxypropylmethyl cellulose (HPMC), polyvinylpyrrolidone (PVP), polyvinyl alcohol (PVA) and polyacrylic acid (PAA) were obtained by freeze-drying of polymeric dispersions either in phosphate buffer solution or water and were sterilized by gamma rays. The matrices were characterized from the technological point of view and evaluated for in vitro release of dextran and BVZ. In vivo evaluation of BVZ release in ocular humours was finally carried out on rabbits. The obtained matrices showed solvent sorption time ranging from a few seconds for PAA to 46 min for HPMC, with shorter times when prepared in buffer solution. The hydration times were up to 5.5-fold higher after sterilization. HPMC and PVA matrices showed a slowdown of the release rate of both dextran and BVZ, but HPMC was selected for following in vivo studies also in consideration of its higher viscosity after rehydration of the matrix. HPMC matrix was well tolerated by the rabbit eye when intravitreally and subconjunctivally administered. The different treatment produced the same effect in terms of drug concentration in aqueous and vitreous humour up to 12 weeks after administration. The results of this study support the possible use of lyophilized matrices as a BVZ delivery system to the posterior segment of the eye.







Similar content being viewed by others
References
Agarwal A, Rhoades WR, Hanout M, Soliman MK, Sarwar S, Sadiq MA, et al. Management of neovascular age-related macular degeneration: current state-of-the-art care for optimizing visual outcomes and therapies in development. Clin Ophthalmol. 2015; https://doi.org/10.2147/OPTH.S74959.
World Health Organization. Action plan for the prevention of avoidable blindness and visual impairment 2009-2013, vol. 2010. Geneva: WHO Document Production Services.
Thrimawithana TR, Young S, Bunt CR, Green C, Alany RG. Drug delivery to the posterior segment of the eye. Drug Discov Today. 2011;16:270–7. https://doi.org/10.1016/j.drudis.2010.12.004.
Joseph M, Trinh HM, Cholkar K, Pal D, Mitra AK. Recent perspectives on the delivery of biologics to back of the eye. Expert Opin Drug Deliv. 2016;14:631–45. https://doi.org/10.1080/17425247.2016.1227783.
Bakri SJ, Snyder MR, Reid JM, Pulido JS, Singh RJ. Pharmacokinetics of intravitreal bevacizumab (Avastin). Ophthalmology. 2007;114:855–9. https://doi.org/10.1016/j.ophtha.2007.01.017.
Ahn J, Kim H, Woo SJ, Park JH, Park S, Hwang DJ, et al. Pharmacokinetics of intravitreally injected bevacizumab in vitrectomized eyes. J Ocular Pharmacol Ther. 2013;29:612–8. https://doi.org/10.1089/jop.2013.0009.
Rauck BM, Friberg TR, Mendez CAM, Park D, Shah V, Bilonick RA, et al. Biocompatible reverse thermal gel sustains the release of intravitreal bevacizumab in vivo. Invest Ophthalmol Vis Sci. 2014;55:469–76. https://doi.org/10.1167/iovs.13-13120.
Burgalassi S, Monti D, Tampucci S, Chetoni P. In vitro evaluation of some parameters involved in mucoadhesion of aqueous polymeric dispersions. Pharm Dev Technol. 2015;20:927–34. https://doi.org/10.3109/10837450.2014.943406.
Gummer CL, Hinz RS, Maibach HI. The skin penetration cell: a design update. Int J Pharm. 1987;40:101–4. https://doi.org/10.1016/0378-5173(87)90053-6.
Dow Brochure, ID 1051. Dow Chemical Company; 2015. https://dowac.custhelp.com/app/answers/detail/a_id/1051/related/1.
Briscoe B, Luckham S, Zhu S. The effects of hydrogen bonding upon the viscosity of aqueous poly(vinyl alcohol) solutions. Polymer. 2000;41:3851–60. https://doi.org/10.1016/S0032-3861(99)00550-9.
Güner A. Properties of aqueous salt solutions of polyvinylpyrrolidone. I. Viscosity characteristics. J Appl Polym Sci. 1996;62:785–8.
Teng C, Gao Y, Wang X, Jiang W, Zhang C, Wang R, et al. Reentanglement kinetics of freeze-dried polymers above the glass transition temperature. Macromolecules. 2012;45:6648–51. https://doi.org/10.1021/ma300885w.
Sebert P, Andrianoff N, Rollet M. Effect of gamma irradiation on hydroxypropylmethylcellulose powders: consequences on physical, rheological and pharmacotechnical properties. Int J Pharm. 1993;99:37–42. https://doi.org/10.1016/0378-5173(93)90320-F.
Su X, Tan MJ, Li Z, Wong M, Rajamani L, Lingam G, et al. Recent progress in using biomaterials as vitreous substitutes. Biomacromolecules. 2015; doi; https://doi.org/10.1021/acs.biomac.5b01091.
Li H, Zhang W, Xu W, Zhang X. Hydrogen bonding governs the elastic properties of poly(vinyl alcohol) in water: single-molecule force spectroscopic studies of PVA by AFM. Macromolecules. 2000;33:465–9. https://doi.org/10.1021/ma990878e.
Sahoo CK, Rao SRM, Sudhaka M. HPMC a biomedical polymer in pharmaceutical dosage forms. J Chem Pharm Sci. 2015;8:875–81.
Paul M, Vieillard V, Roumi E, Cauvin A, Despiau MC, Laurent M, et al. Long-term stability of bevacizumab repackaged in 1 mL polypropylene syringes for intravitreal administration. Ann Pharm Fr. 2012;70:139–54. https://doi.org/10.1016/j.pharma.2012.03.006.
Sharma G, Khalili A, Awwad S, Malik K, Matejtschuk P, Gaisford S, et al. Freeze drying to develop a bevacizumab-based tablet for ocular implantation. Invest Ophthalmol Vis Sci. 2013;54:Abstract 1082.
Sousa F, Cruz A, Fonte P, Mendes Pinto I, Neves-Petersen MT, Sarmento B. A new paradigm for antiangiogenic therapy through controlled release of bevacizumab from PLGA nanoparticles. Sci Rep. 2017:2017. https://doi.org/10.1038/s41598-017-03959-4.
Taniwaki L, Mendonça R, Cunha-Júnior AS, Faraco AAG, Ribeiro JAS, Scott IU, et al. Effect of lyophilization on the in vitro biological activity of bevacizumab. Eye. 2010;24:1628–9. https://doi.org/10.1038/eye.2010.96.
Yandrapu SK, Upadhyay AK, Petrash JM, Kompella UB. Nanoparticles in porous microparticles prepared by supercritical infusion and pressure quench technology for sustained delivery of bevacizumab. Mol Pharm. 2013;10:4676–86. https://doi.org/10.1021/mp400487f.
Cleland JL, Lam X, Kendrick B, Yang J, Yang TH, Overcashier D, et al. A specific molar ratio of stabilizer to protein is required for storage stability of a lyophilized monoclonal antibody. J Pharm Sci. 2001;90:310–21. https://doi.org/10.1002/1520-6017(200103)90:3<310::AID-JPS6>3.0.CO;2-R.
Grieb T, Forng RY, Brown R, Owolabi T, Maddox E, McBain A, et al. Effective use of gamma Irradiation for pathogen inactivation of monoclonal antibody preparations. Biologicals. 2002;30:207–16. https://doi.org/10.1006/biol.2002.0330.
Silindir M, Ozer AY. Sterilization methods and the comparison of E-beam sterilization with gamma radiation sterilization. FABAD J Pharm Sci. 2009;34:43–53.
Abrishami M, Ganavati SZ, Soroush D, Rouhbakhsh M, Jaafari MR, Malaekeh-Nikouei B. Preparation, characterization, and in vivo evaluation of nanoliposomes-encapsulated bevacizumab (Avastin) for intravitreal administration. Retina. 2009;29:699–703. https://doi.org/10.1097/IAE.0b013e3181a2f42a.
Andrew JS, Anglin EJ, Wu EC, Chen MY, Cheng L, Freeman WR, et al. Sustained release of a monoclonal antibody from electrochemically prepared mesoporous silicon oxide. Adv Funct Mater. 2010;20:4168–74. https://doi.org/10.1002/adfm.201000907.
Lovett ML, Wang X, Yucel T, York L, Keirstead M, Haggerty L, et al. Silk hydrogel for sustained ocular delivery of anti-vascular endothelial growth factor (anti-VEGF) therapeutics. Eur J Pharm Biopharm. 2015;95:271–8. https://doi.org/10.1016/j.ejpb.2014.12.029.
Nomoto H, Shiraga F, Kuno N, Kimura E, Fujii S, Shinomiya K, et al. Pharmacokinetics of bevacizumab after topical, subconjunctival, and intravitreal administration in rabbits. Invest Ophthalmol Vis Sci. 2009;50:4807. https://doi.org/10.1167/iovs.08-3148.
Sinapis CI, Routsias JG, Sinapis AI, Sinapis DI, Agrogiannis GD, Pantopoulou A, et al. Pharmacokinetics of intravitreal bevacizumab (Avastin®) in rabbits. Clinical Ophthalmol. 2011; https://doi.org/10.2147/OPTH.S19555.
Ye Z, Ji YL, Ma X, Wen JG, Wei W, Huang SM. Pharmacokinetics and distributions of bevacizumab by intravitreal injection of bevacizumab-PLGA microspheres in rabbits. Int J Ophthalmol. 2015; https://doi.org/10.3980/j.issn.2222-3959.2015.04.02.
Kim MJ, Han ES, Kim JW, Kim TW. Aqueous humor concentration of bevacizumab after subconjunctival injection in rabbit. J Ocular Pharmacol Ther. 2010;26:49–54. https://doi.org/10.1089/jop.2009.0022.
Davis B, Normando EM, Guo L, Turner LA, Nizari S, O’Shea P, et al. Topical delivery of Avastin to the posterior segment of the eye in vivo using annexin A5-associated liposomes. Small. 2014;10:1575–84. https://doi.org/10.1002/smll.201303433.
Li F, Hurley B, Liu Y, Leonard B, Griffith M. Controlled release of bevacizumab through nanospheres for extended treatment of age-related macular degeneration. Open Ophthalmol J. 2012;6:54–8. https://doi.org/10.2174/1874364101206010054.
Pandit J, Sultana Y, Aqil M. Chitosan-coated PLGA nanoparticles of bevacizumab as novel drug delivery to target retina: optimization, characterization, and in vitro toxicity evaluation. Art Cells Nanomed Biothechnol. 2017;45:1397–407. https://doi.org/10.1080/21691401.2016.1243545.
Battaglia L, Gallarate M, Peira E, Chirio D, Solazzi I, Giordano SMA, et al. Bevacizumab loaded solid lipid nanoparticles prepared by the coacervation technique: preliminary in vitro studies. Nanotechnology. 2015;26:255102. https://doi.org/10.1088/0957-4484/26/25/255102.
Xie B, Jin L, Luo Z, Yu J, Shi S, Zhang Z, et al. An injectable thermosensitive polymeric hydrogel for sustained release of Avastin® to treat posterior segment disease. Int J Pharm. 2015;490:375–83. https://doi.org/10.1016/j.ijpharm.2015.05.071.
De Cogan F, Hill LJ, Lynch A, Morgan-Warren PJ, Lechner J, Berwick MR, et al. Topical delivery of anti-VEGF drugs to the ocular posterior segment using cell-penetrating peptides. Invest Ophthalmol Vis Sci. 2017;58:2578. https://doi.org/10.1167/iovs.16-20072.
Ambati J, Canakis CS, Miller JW, Gragoudas ES, Edwards A, Weissgold DJ, et al. Diffusion of high molecular weight compounds through sclera. Invest Ophthalmol Vis Sci. 2000;41:1181–5.
Ambati J, Gragoudas ES, Miller JW, You TT, Miyamoto K, Delori FC, et al. Transscleral delivery of bioactive protein to the choroid and retina. Invest Ophthalmol Vis Sci. 2000;41:1186–91.
Maurice DM, Mishima S. Ocular pharmacokinetics. In: Sears ML, editor. Pharmacology of the eye. Berlin: Springer-Verlag; 1984. p. 19–116.
Del Amo EM, Urtti A. Rabbit as an animal model for intravitreal pharmacokinetics: clinical predictability and quality of the published data. Exp Eye Res. 2015;137:111–24. https://doi.org/10.1016/j.exer.2015.05.003.
Acknowledgements
This work was funded by University of Pisa (grant PRA 2016_27). The authors would like to thank Dr. Carla Lenzi and Prof. Giancarlo De Montis for technical support to histological analysis and the relevant interpretation of the results.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All institutional and national guidelines for the care and use of laboratory animals were followed.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Burgalassi, S., Monti, D., Nicosia, N. et al. Freeze-dried matrices for ocular administration of bevacizumab: a comparison between subconjunctival and intravitreal administration in rabbits. Drug Deliv. and Transl. Res. 8, 461–472 (2018). https://doi.org/10.1007/s13346-018-0520-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-018-0520-x