Abstract
Objective
Resting energy expenditure (REE) is an important tool in nutrition management, especially in type 2 diabetes mellitus (T2DM). The predicted REE (pREE) was reported to be inaccurate, compared with measured REE (mREE) in Japanese T2DM patients. Despite the accuracy of REE, measured via indirect calorimetry (mREE), the technique is demanding. This study evaluated the associated clinical factors of the difference between pREE and mREE in Japanese patients with T2DM.
Methods
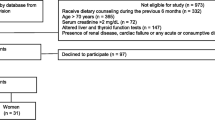
Forty-nine Japanese patients with T2DM but no severe complications (32 men and 17 women) were enrolled. mREE was determined via indirect calorimetry.
Results
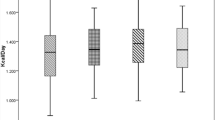
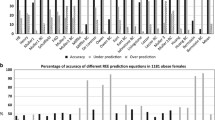
Participants average age was 56.3 ± 11.0 years, body mass index was 25.2 ± 3.6 kg/m2, and HbA1c was 9.6 ± 1.6%. The mean mREE was 1099 ± 212 kcal/day. Age, body mass index, hemoglobin, and uric acid levels were all associated with mREE by simple regression; of these, body weight was the significant factor in the multiple regression analysis. When the patients were divided into tertiles, the average mREE values were lower than the pREE values for each group. The difference between mREE and pREE was largest in the lowest value group, whose subjects were mostly women aged over 50 years. This group of women showed significantly lower mREE (904 ± 121 kcal) in comparison with men in the same age group, with 26% overestimation of pREE, even when the equation that yielded the closest mREE value was used.
Conclusion
The previously reported pREE overestimates mREE in Japanese patients with T2DM, especially in postmenopausal women.



Similar content being viewed by others
References
Ravussin E, Lillioja S, Anderson TE, Christin L, Bogardus C. Determinants of 24-hour energy expenditure in man. Methods and results using a respiratory chamber. J Clin Invest. 1986;78:1568–78.
Harris JA, Benedict FG. A Biometric Study of Human Basal Metabolism. Proc Natl Acad Sci U S A. 1918;4:370–3.
Case KO, Brahler CJ, Heiss C. Resting energy expenditures in Asian women measured by indirect calorimetry are lower than expenditures calculated from prediction equations. J Am Diet Assoc. 1997;97:1288–92.
Ganpule AA, Tanaka S, Ishikawa-Takata K, Tabata I. Interindividual variability in sleeping metabolic rate in Japanese subjects. Eur J Clin Nutr. 2007;61:1256–61.
Miyake R, Tanaka S, Ohkawara K, Ishikawa-Takata K, Hikihara Y, Taguri E, Kayashita J, Tabata I. Validity of predictive equations for basal metabolic rate in Japanese adults. J Nutr Sci Vitaminol. (Tokyo). 2011;57:224–32.
Ikeda K, Fujimoto S, Goto M, Yamada C, Hamasaki A, Ida M, Nagashima K, Shide K, Kawamura T, Inagaki N. A new equation to estimate basal energy expenditure of patients with diabetes. Clin Nutr. 2013;32:777–82.
Buscemi S, Verga S, Caimi G, Cerasola G. A low resting metabolic rate is associated with metabolic syndrome. Clin Nutr. 2007;26:806–9.
Miyake R, Ohkawara K, Ishikawa-Takata K, Morita A, Watanabe S, Tanaka S. Obese Japanese adults with type 2 diabetes have higher basal metabolic rates than non-diabetic adults. J Nutr Sci Vitaminol. (Tokyo). 2011;57:348–54.
Tabata S, Kinoshita N, Yamada S, Matsumoto H. Accuracy of basal metabolic rate estimated by predictive equations in Japanese with type 2 diabetes. Asia Pac J Clin Nutr. 2018;27:763–9.
Cooper JA, Watras AC, O’Brien MJ, Luke A, Dobratz JR, Earthman CP, Schoeller DA. Assessing validity and reliability of resting metabolic rate in six gas analysis systems. J Am Diet Assoc. 2009;109:128–32.
Alam DS, Hulshof PJ, Roordink D, Meltzer M, Yunus M, Salam MA, van Raaij JM. Validity and reproducibility of resting metabolic rate measurements in rural Bangladeshi women: comparison of measurements obtained by Medgem and by Deltatrac device. Eur J Clin Nutr. 2005;59:651–7.
Weir JB. New methods for calculating metabolic rate with special reference to protein metabolism. J Physiol. 1949;109:1–9.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, Yamagata K, Tomino Y, Yokoyama H, Hishida A. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
Kashiwagi A, Kasuga M, Araki E, Oka Y, Hanafusa T, Ito H, et al. Society CotSoDMRLToJD. International clinical harmonization of glycated hemoglobin in Japan: from Japan Diabetes Society to National Glycohemoglobin Standardization Program values. J Diabetes Investig. 2012;3:39–40.
Huang KC, Kormas N, Steinbeck K, Loughnan G, Caterson ID. Resting metabolic rate in severely obese diabetic and nondiabetic subjects. Obes Res. 2004;12:840–5.
Martin K, Wallace P, Rust PF, Garvey WT. Estimation of resting energy expenditure considering effects of race and diabetes status. Diabetes Care. 2004;27:1405–11.
Gougeon R, Lamarche M, Yale JF, Venuta T. The prediction of resting energy expenditure in type 2 diabetes mellitus is improved by factoring for glycemia. Int J Obes Relat Metab Disord. 2002;26:1547–52.
Ryan M, Sallé A, Guilloteau G, Genaitay M, Livingstone MB, Ritz P. Resting energy expenditure is not increased in mildly hyperglycaemic obese diabetic patients. Br J Nutr. 2006;96:945–8.
Ikeda K, Fujimoto S, Goto M, Yamada C, Hamasaki A, Shide K, Kawamura T, Inagaki N. Impact of endogenous and exogenous insulin on basal energy expenditure in patients with type 2 diabetes under standard treatment. Am J Clin Nutr. 2011;94:1513–8.
Weyer C, Bogardus C, Pratley RE. Metabolic factors contributing to increased resting metabolic rate and decreased insulin-induced thermogenesis during the development of type 2 diabetes. Diabetes. 1999;48:1607–14.
Hashimoto R, Yoshida N, Miyazaki H, Adachi H, Tashiro H, Toshima H. Relationship among energy expenditure, Nutrient intake and risk factors in a farming village, Kyushu. Kyoei-Seimei kenkyu josei ronbun-shu. 1990;6:19–28 [in Japanese].
Levine W, Dyer AR, Shekelle RB, Schoenberger JA, Stamler J. Serum uric acid and 11.5-years morality of middle-aged women: findings of the Chicago Heart Association Detection project in industry. J Clin Epidemiol. 1989;42:257–67.
Christensen B. Whole body metabolic effects of prolonged endurance training in combination with erythropoietin treatment in humans: a randomized placebo controlled trial. Am J Physiol Endocrinol Metab. 2013;305:E879–89.
Krings A, Rahman S, Huang S, Lu Y, Czernik PJ, Lecka-Czernik B. Bone marrow fat has brown adipose tissue characteristics, which are attenuated with aging and diabetes. Bone. 2012;50:546–52.
Arciero PJ, Goran MI, Gardner AM. A practical equation to predict resting metabolic rate in older females. J Am Geriatr Soc. 1993;41:389–95.
Geer EB, Shen W. Gender differences in insulin resistance, body composition, and energy balance. Gend Med. 2009;6(Suppl 1):60–75.
Liu P, Ji Y, Yuen T, Rendina-Ruedy E, DeMambro VE, Dhawan S, et al. Blocking FSH induces thermogenic adipose tissue and reduces body fat. Nature. 2017;546:107–12.
Hodson L, Harnden K, Banerjee R, Real B, Marinou K, Karpe F, Fielding BA. Lower resting and total energy expenditure in postmenopausal compared with premenopausal women matched for abdominal obesity. J Nutr Sci. 2014;3:e3.
Kovanen V, Aukee P, Kokko K, Finni T, Tarkka IM, Tammelin T, Kujala UM, Sipilä S, Laakkonen EK. Design and protocol of Estrogenic Regulation of Muscle Apoptosis (ERMA) study with 47 to 55-year-old women’s cohort: novel results show menopause-related differences in blood count. Menopause. 2018;25:1020–32.
Kanis JA, McCloskey EV, Johansson H, Cooper C, Rizzoli R, Reginster JY, et al. on behalf of the Scientific Advisory Board of the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) and the Committee of Scientific Advisors of the International Osteoporosis Foundation (IOF). European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 2013;24:23–57.
Ogata M, Ide R, Takizawa M, Tanaka M, Tetsuo T, Sato A, Iwasaki N, Uchigata Y. Association between basal metabolic function and bone metabolism in postmenopausal women. Nutrition. 2015;31:1394–401.
Acknowledgements
We thank Ms. M Tomioka for her technical assistance. This study was partially supported by a research Grants from the Shukutoku University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest to declare.
Human and animals rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and/or with the Helsinki Declaration of 1964 and later versions. Informed consent or substitute for it was obtained from all patients for being included in the study.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration, and the study protocol complied with the Ethical Guidelines for Medical and Health Research Involving Human Subjects. The study design was approved by the Ethics Committee of the Tokyo Women’s Medical University School of Medicine (9 May, 2017 No. 3829R).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Ide, R., Ogata, M., Iwasaki, N. et al. Low resting energy expenditure in postmenopausal Japanese women with type 2 diabetes mellitus. Diabetol Int 10, 268–278 (2019). https://doi.org/10.1007/s13340-019-00391-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13340-019-00391-z