Abstract
Background
The purpose of our analysis was to compare the results of treatment in patients who underwent resection for colorectal carcinoma.
Methods
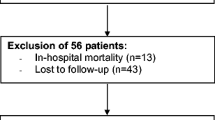
In the period from 1/1/1991 to 31/12/2000 1478 patients with colorectal carcinoma underwent potentially curative resection. We divided them into two 5-year period groups according to different treatment regimes. The 5-year net survival rate was estimated, where the net survival is the probability of survival derived solely from the cancer-specific hazard.
Results
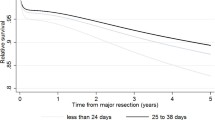
In a 10-year period, we resected 1478 patients. The 5-year net survival rate for R0-resected patients with colon cancer increased from 76.3 to 85.2% between the periods 1991–1995 and 1995–2000. The 5-year net survival rate for R0-resected patients with rectal cancer also increased from 67.5 to 73% in the same period.
Conclusion
A comparison of the 5-year net survival rate for R0-resected patients with colorectal cancer increased in the last period from 1995 to 2000 compared with the period from 1991 to 1995. In multivariate analysis, early stage at diagnosis and adjuvant chemotherapy was both associated with better net survival after surgery with curative intent. The improvement of net survival is potentially the result of combination of better surgical and adjuvant therapy.





Similar content being viewed by others
References
Zadnik V, Primic Zakelj M, Lokar K et al (2017) Cancer burden in slovenia with the time trends analysis. Radiol Oncol 51:47–55. https://doi.org/10.1515/raon-2017-0008
Vrdoljak E, Bodoky G, Jassem J et al (2016) Cancer Control in Central and Eastern Europe: current situation and recommendations for improvement. Oncologist 21:1183–1190. https://doi.org/10.1634/theoncologist.2016-0137
Vitale SG, Valenti G, Rapisarda AMC et al (2016) P16INK4a as a progression/regression tumour marker in LSIL cervix lesions: our clinical experience. Eur J Gynaecol Oncol 37:685–688. https://doi.org/10.12892/ejgo3240.2016
Valenti G, Vitale SG, Tropea A et al (2017) Tumor markers of uterine cervical cancer: a new scenario to guide surgical practice? Updates Surg 69:441–449. https://doi.org/10.1007/s13304-017-0491-3
Ibragimova MK, Tsyganov MM, Litviakov NV (2018) Human papillomavirus and colorectal cancer. Med Oncol 35:140. https://doi.org/10.1007/s12032-018-1201-9
Sant M, Capocaccia R, Coleman MP et al (2001) Cancer survival increases in Europe, but international differences remain wide. Eur J Cancer 37:1659–1667
Blomqvist P, Ekbom A, Nyrén O et al (1997) Survival after colon cancer 1973–1990 in Sweden. Convergence between catchment areas. Ann Surg 225:208–216
Martijn H, Voogd AC, van de Poll-Franse LV et al (2003) Improved survival of patients with rectal cancer since 1980: a population-based study. Eur J Cancer 39:2073–2079
Finn-Faivre C, Maurel J, Benhamiche AM et al (1999) Evidence of improving survival of patients with rectal cancer in France: a population based study. Gut 44:377–381
Biondi A, Tropea A, Tropea DA, Basile F (2010) Clinical rescue evaluation in laparoscopic surgery for hepatic metastases by colorectal cancer. Surg Laparosc Endosc Percutan Tech 20:69–72. https://doi.org/10.1097/SLE.0b013e3181d83f02
Siegel R, Desantis C, Jemal A (2014) Colorectal cancer statistics, 2014. CA Cancer J Clin 64:104–117. https://doi.org/10.3322/caac.21220
Wingo PA, Ries LA, Rosenberg HM et al (1998) Cancer incidence and mortality, 1973–1995: a report card for the US. Cancer 82:1197–1207
Marventano S, Grosso G, Mistretta A et al (2014) Evaluation of four comorbidity indices and Charlson comorbidity index adjustment for colorectal cancer patients. Int J Colorectal Dis 29:1159–1169. https://doi.org/10.1007/s00384-014-1972-1
Wu JS, Fazio VW (2000) Colon cancer. Dis Colon Rectum 43:1473–1486
Laganà AS, Vitale SG, Trovato MA et al (2016) Full-thickness excision versus shaving by laparoscopy for intestinal deep infiltrating endometriosis: rationale and potential treatment options. Biomed Res Int 2016:3617179. https://doi.org/10.1155/2016/3617179
Raffaelli R, Garzon S, Baggio S et al (2018) Mesenteric vascular and nerve sparing surgery in laparoscopic segmental intestinal resection for deep infiltrating endometriosis. Eur J Obstet Gynecol Reprod Biol 231:214–219. https://doi.org/10.1016/j.ejogrb.2018.10.057
de Buck van Overstraeten A, Eshuis EJ, Vermeire S et al (2017) Short- and medium-term outcomes following primary ileocaecal resection for Crohn’s disease in two specialist centres. Br J Surg 104:1713–1722. https://doi.org/10.1002/bjs.10595
Labianca R, Milesi L, Mosconi S et al (2007) The role of adjuvant chemotherapy in colon cancer. Surg Oncol 16(Suppl 1):S93–S96
Fischer J, Walker LC, Robinson BA et al (2019) Clinical implications of the genetics of sporadic colorectal cancer. ANZ J Surg. https://doi.org/10.1111/ans.15074
Vitale SG, Laganà AS, Capriglione S et al (2017) Target therapies for uterine carcinosarcomas: current evidence and future perspectives. Int J Mol Sci. https://doi.org/10.3390/ijms18051100
Vitale SG, Capriglione S, Zito G et al (2019) Management of endometrial, ovarian and cervical cancer in the elderly: current approach to a challenging condition. Arch Gynecol Obstet 299:299–315. https://doi.org/10.1007/s00404-018-5006-z
Brenner H, Kloor M, Pox CP (2014) Colorectal cancer. Lancet (London, England) 383:1490–1502. https://doi.org/10.1016/S0140-6736(13)61649-9
Mitry E, Bouvier A-M, Esteve J, Faivre J (2005) Improvement in colorectal cancer survival: a population-based study. Eur J Cancer 41:2297–2303. https://doi.org/10.1016/j.ejca.2005.01.028
Pohar Perme M, Estève J, Rachet B (2016) Analysing population-based cancer survival—settling the controversies. BMC Cancer 16:933. https://doi.org/10.1186/s12885-016-2967-9
Perme MP, Henderson R, Stare J (2009) An approach to estimation in relative survival regression. Biostatistics 10:136–146. https://doi.org/10.1093/biostatistics/kxn021
Stare J, Pohar M, Henderson R (2005) Goodness of fit of relative survival models. Stat Med 24:3911–3925. https://doi.org/10.1002/sim.2414
R Core Team (2018) A language and environment for statistical computing. In: R Found. Stat. Comput. https://www.r-project.org/. Accessed 1 Jan 2019
Perme MP, Pavlic K (2018) Nonparametric relative survival analysis with the R Package relsurv. J Stat Softw. https://doi.org/10.18637/jss.v087.i08
Omejc M, Stor Z, Juvan R et al (2004) Colorectal cancer in Slovenia at the turn of the century. Eur Surg 36:356–359. https://doi.org/10.1007/s10353-004-0108-1
Wibe A, Møller B, Norstein J et al (2002) A national strategic change in treatment policy for rectal cancer–implementation of total mesorectal excision as routine treatment in Norway. A national audit. Dis Colon Rectum 45:857–866
Angell-Andersen E, Tretli S, Coleman MP et al (2004) Colorectal cancer survival trends in Norway 1958–1997. Eur J Cancer 40:734–742. https://doi.org/10.1016/j.ejca.2003.09.034
Bellia A, Vitale SG, Laganà AS et al (2016) Feasibility and surgical outcomes of conventional and robot-assisted laparoscopy for early-stage ovarian cancer: a retrospective, multicenter analysis. Arch Gynecol Obstet 294:615–622. https://doi.org/10.1007/s00404-016-4087-9
Enker WE, Thaler HT, Cranor ML, Polyak T (1995) Total mesorectal excision in the operative treatment of carcinoma of the rectum. J Am Coll Surg 181:335–346
Steele RJ (1999) Anterior resection with total mesorectal excision. J R Coll Surg Edinb 44:40–45
Bisset IP, Chau KY, Hill GL (2000) Extrafascial excision of the rectum: surgical anatomy of the fascia propria. Dis Colon Rectum 43:903–910
MacFarlane JK, Ryall RD, Heald RJ (1993) Mesorectal excision for rectal cancer. Lancet (London, England) 341:457–460
Chapuis P, Bokey L, Fahrer M et al (2002) Mobilization of the rectum: anatomic concepts and the bookshelf revisited. Dis Colon Rectum 45:1–8 (discussion 8–9)
Herbst F, Widder J, Maier A (2006) Diagnosis and therapy of rectal cancer. Eur Surg 38:129–134. https://doi.org/10.1007/s10353-006-0237-9
Church JM, Gibbs P, Chao MW, Tjandra JJ (2003) Optimizing the outcome for patients with rectal cancer. Dis Colon Rectum 46:389–402. https://doi.org/10.1097/01.DCR.0000054884.45152.15
de Haas-Kock DF, Baeten CG, Jager JJ et al (1996) Prognostic significance of radial margins of clearance in rectal cancer. Br J Surg 83:781–785
Kapiteijn E, Marijnen CA, Nagtegaal ID et al (2001) Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N Engl J Med 345:638–646. https://doi.org/10.1056/NEJMoa010580
Beets-Tan RGH, Beets GL (2003) Rectal cancer: how accurate can imaging predict the T stage and the circumferential resection margin? Int J Colorectal Dis 18:385–391. https://doi.org/10.1007/s00384-003-0480-5
Fuchsjäger MH, Maier AG, Schima W et al (2003) Comparison of transrectal sonography and double-contrast MR imaging when staging rectal cancer. AJR Am J Roentgenol 181:421–427. https://doi.org/10.2214/ajr.181.2.1810421
Brown G, Kirkham A, Williams GT et al (2004) High-resolution MRI of the anatomy important in total mesorectal excision of the rectum. AJR Am J Roentgenol 182:431–439. https://doi.org/10.2214/ajr.182.2.1820431
Blomqvist L, Brown G (2004) Colorectal cancer imaging. AJR Am J Roentgenol 182:1600–1601. https://doi.org/10.2214/ajr.182.6.1821600a
Akasu T, Iinuma G, Fujita T et al (2005) Thin-section MRI with a phased-array coil for preoperative evaluation of pelvic anatomy and tumor extent in patients with rectal cancer. AJR Am J Roentgenol 184:531–538. https://doi.org/10.2214/ajr.184.2.01840531
Pijl MEJ, Chaoui AS, Wahl RL, van Oostayen JA (2002) Radiology of colorectal cancer. Eur J Cancer 38:887–898
Colorectal Cancer Collaborative Group (2001) Adjuvant radiotherapy for rectal cancer: a systematic overview of 8507 patients from 22 randomised trials. Lancet (London, England) 358:1291–1304. https://doi.org/10.1016/S0140-6736(01)06409-1
Sauer R, Becker H, Hohenberger W et al (2004) Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med 351:1731–1740. https://doi.org/10.1056/NEJMoa040694
Wagman R, Minsky BD, Cohen AM et al (1998) Sphincter preservation in rectal cancer with preoperative radiation therapy and coloanal anastomosis: long term follow-up. Int J Radiat Oncol Biol Phys 42:51–57
Minsky BD (1999) Adjuvant therapy of rectal cancer. Semin Oncol 26:540–544
Vitale SG, La Rosa VL, Rapisarda AMC, Laganà AS (2017) The importance of fertility preservation counseling in patients with gynecologic cancer. J Reprod Infertil 18:261–263
Martinez F (2017) Update on fertility preservation from the Barcelona International Society for Fertility Preservation-ESHRE-ASRM 2015 expert meeting: indications, results and future perspectives. Hum Reprod 32:1802–1811. https://doi.org/10.1093/humrep/dex218
Donnez J, Dolmans M-M (2017) Fertility preservation in women. N Engl J Med 377:1657–1665. https://doi.org/10.1056/NEJMra1614676
Shandley LM, McKenzie LJ (2019) Recent advances in fertility preservation and counseling for reproductive-aged women with colorectal cancer: a systematic review. Dis Colon Rectum 62:762–771. https://doi.org/10.1097/DCR.0000000000001351
Vitale SG, La Rosa VL, Rapisarda AMC, Laganà AS (2018) Fertility preservation in women with gynaecologic cancer: the impact on quality of life and psychological well-being. Hum Fertil (Camb) 21:35–38. https://doi.org/10.1080/14647273.2017.1339365
Haggar F, Pereira G, Preen D et al (2013) Maternal and neonatal outcomes in pregnancies following colorectal cancer. Surg Endosc 27:2327–2336. https://doi.org/10.1007/s00464-012-2774-6
Baggio S, Pomini P, Zecchin A et al (2015) Delivery and pregnancy outcome in women with bowel resection for deep endometriosis: a retrospective cohort study. Gynecol Surg 12:279–285. https://doi.org/10.1007/s10397-015-0901-9
Valle L, Vilar E, Tavtigian SV, Stoffel EM (2019) Genetic predisposition to colorectal cancer: syndromes, genes, classification of genetic variants and implications for precision medicine. J Pathol 247:574–588. https://doi.org/10.1002/path.5229
Funding
The work was not supported by any fund/grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
All procedures performed in studies involving animals were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all subjects.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Štor, Z., Blagus, R., Tropea, A. et al. Net survival of patients with colorectal cancer: a comparison of two periods. Updates Surg 71, 687–694 (2019). https://doi.org/10.1007/s13304-019-00662-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-019-00662-z