Abstract
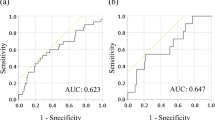
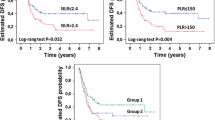
Interaction between tumour and host triggers a systemic inflammatory response. This situation has been associated to cancer progression. Several peripheral blood inflammatory scores have been recently developed, as PLR. Data about the relationship between these scores and cancer prognosis are contradictory. Therefore, the aim of our work is to evaluate the capability of PLR to predict long-term outcomes (OS and RFS) in patients who underwent curative surgery for colon cancer. A retrospective study was designed with patients who underwent curative surgery for colon cancer between September 2008 and January 2012 at Rio Hortega University Hospital, Valladolid (Spain). We analysed the influence of PLR and other clinical variables on OS and RFS. Finally, 201 patients were analysed. Optimal cut-off value for PLR, established with ROC curves, was 153. 1-, 3- and 5-year OS were: 99.0, 90.4 and 82.3% for low PLR, and 93.8, 74.9 and 61.9% for high PLR, p < 0.001. 1-, 3- and 5-year RFS were: 92.4, 84.7 and 77.6% for low PLR, and 83.3, 64.5 and 52.6% for high PLR, p < 0.001. In MVA, high PLR was an independent negative prognostic factor for OS (HR = 2.11; 95% CI 1.22–3.66; p = 0.008) and RFS (HR = 1.99; 95% CI 1.19–3.34; p = 0.009). PLR represents an independent negative prognostic factor for OS and RFS in our sample of patients who underwent curative surgery for colon cancer. However, further studies with a larger sample size from different populations are necessary to confirm this conclusion.


Similar content being viewed by others
References
Aran V, Victorino AP, Thuler LC, Ferreira CG, Levine JS, Ahnen DJ et al (2016) Colorectal cancer: epidemiology, disease mechanisms and interventions to reduce onset and mortality. Clin Colorectal Cancer 15(3):195–203
Coussens LM, Werb Z (2002) Inflammation and cancer. Nature 420(6917):860–867
Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144(5):646–674
Ishizuka M, Nagata H, Takagi K, Iwasaki Y, Kubota K (2012) Inflammation-based prognostic system predicts postoperative survival of colorectal cancer patients with a normal preoperative serum level of carcinoembryonic antigen. Ann Surg Oncol 19(11):3422–3431
Pine JK, Morris E, Hutchins GG, West NP, Jayne DG, Quirke P et al (2015) Systemic neutrophil-to-lymphocyte ratio in colorectal cancer: the relationship to patient survival, tumour biology and local lymphocytic response to tumour. Br J Cancer 113(2):204–211
Park BK, Park JW, Han EC, Ryoo SB, Han SW, Kim TY et al (2016) Systemic inflammatory markers as prognostic factors in stage IIA colorectal cancer. J Surg Oncol 114(2):216–221
Peng HX, Lin K, He BS, Pan YQ, Ying HQ, Hu XX et al (2016) Platelet-to-lymphocyte ratio could be a promising prognostic biomarker for survival of colorectal cancer: a systematic review and meta-analysis. FEBS Open Bio 6(7):742–750
Emir S, Aydin M, Can G, Bali I, Yildirim O, Öznur M et al (2015) Comparison of colorectal neoplastic polyps and adenocarcinoma with regard to NLR and PLR. Eur Rev Med Pharmacol Sci 19(19):3613–3618
Zhou X, Du Y, Huang Z, Xu J, Qiu T, Wang J et al (2014) Prognostic value of PLR in various cancers: a meta-analysis. PLoS One 9(6):e101119
Pedrazzani C, Mantovani G, Fernandes E, Bagante F, Luca Salvagno G, Surci N et al (2017) Assessment of neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio and platelet count as predictors of long-term outcome after R0 resection for colorectal cancer. Sci Rep 7(1):1494
Akgül Ö, Çetinkaya E, Yalaza M, Özden S, Tez M (2017) Prognostic efficacy of inflammation-based markers in patients with curative colorectal cancer resection. World J Gastrointest Oncol 9(7):300–307
Fearon K, Strasser F, Anker SD, Bosaeus I, Bruera E, Fainsinger RL et al (2011) Definition and classification of cancer cachexia: an international consensus. Lancet Oncol 12(5):489–495
Blum D, Stene GB, Solheim TS, Fayers P, Hjermstad MJ, Baracos VE et al (2014) Validation of the consensus-definition for cancer cachexia and evaluation of a classification model—a study based on data from an international multicentre project (EPCRC-CSA). Ann Oncol 25(8):1635–1642
Nieswandt B, Hafner M, Echtenacher B, Männel DN (1999) Lysis of tumor cells by natural killer cells in mice is impeded by platelets. Cancer Res 59(6):1295–1300
Mantovani A, Allavena P, Sica A, Balkwill F (2008) Cancer-related inflammation. Nature 454(7203):436–444
Gu X, Gao XS, Qin S, Li X, Qi X, Ma M et al (2016) Elevated platelet to lymphocyte ratio is associated with poor survival outcomes in patients with colorectal cancer. PLoS One 11(9):e0163523
Min GT, Wang YH, Yao N, Zhao JM, Wang J, Wang HP et al (2017) The prognostic role of pretreatment platelet-to-lymphocyte ratio as predictors in patients with colorectal cancer: a meta-analysis. Biomark Med 11(1):87–97
Huang XZ, Chen WJ, Zhang X, Wu CC, Zhang CY, Sun SS et al (2017) An elevated platelet-to-lymphocyte ratio predicts poor prognosis and clinicopathological characteristics in patients with colorectal cancer: a meta-analysis. Dis Markers 2017:1053125
Guo YH, Sun HF, Zhang YB, Liao ZJ, Zhao L, Cui J et al (2017) The clinical use of the platelet/lymphocyte ratio and lymphocyte/monocyte ratio as prognostic predictors in colorectal cancer: a meta-analysis. Oncotarget 8(12):20011–20024
Son HJ, Park JW, Chang HJ, Kim DY, Kim BC, Kim SY et al (2013) Preoperative plasma hyperfibrinogenemia is predictive of poor prognosis in patients with nonmetastatic colon cancer. Ann Surg Oncol 20(9):2908–2913
Baranyai Z, Krzystanek M, Jósa V, Dede K, Agoston E, Szász AM et al (2014) The comparison of thrombocytosis and platelet-lymphocyte ratio as potential prognostic markers in colorectal cancer. Thromb Haemost 111(3):483–490
Mori K, Toiyama Y, Saigusa S, Fujikawa H, Hiro J, Kobayashi M et al (2015) Systemic analysis of predictive biomarkers for recurrence in colorectal cancer patients treated with curative surgery. Dig Dis Sci 60(8):2477–2487
Szkandera J, Pichler M, Absenger G, Stotz M, Arminger F, Weissmueller M et al (2014) The elevated preoperative platelet to lymphocyte ratio predicts decreased time to recurrence in colon cancer patients. Am J Surg 208(2):210–214
Ying HQ, Deng QW, He BS, Pan YQ, Wang F, Sun HL et al (2014) The prognostic value of preoperative NLR, d-NLR, PLR and LMR for predicting clinical outcome in surgical colorectal cancer patients. Med Oncol 31(12):305
Neofytou K, Smyth EC, Giakoustidis A, Khan AZ, Cunningham D, Mudan S (2014) Elevated platelet to lymphocyte ratio predicts poor prognosis after hepatectomy for liver-only colorectal metastases, and it is superior to neutrophil to lymphocyte ratio as an adverse prognostic factor. Med Oncol 31(10):239
Zou ZY, Liu HL, Ning N, Li SY, Du XH, Li R (2016) Clinical significance of pre-operative neutrophil lymphocyte ratio and platelet lymphocyte ratio as prognostic factors for patients with colorectal cancer. Oncol Lett 11(3):2241–2248
Josse JM, Cleghorn MC, Ramji KM, Jiang H, Elnahas A, Jackson TD et al (2016) The neutrophil-to-lymphocyte ratio predicts major perioperative complications in patients undergoing colorectal surgery. Colorectal Dis 18(7):O236–O242
Cao X, Zhao G, Yu T, An Q, Yang H, Xiao G (2017) Preoperative prognostic nutritional index correlates with severe complications and poor survival in patients with colorectal cancer undergoing curative laparoscopic surgery: a retrospective study in a single Chinese institution. Nutr Cancer 69(3):454–463
Kwon HC, Kim SH, Oh SY, Lee S, Lee JH, Choi HJ et al (2012) Clinical significance of preoperative neutrophil-lymphocyte versus platelet-lymphocyte ratio in patients with operable colorectal cancer. Biomarkers 17(3):216–222
Ozawa T, Ishihara S, Nishikawa T, Tanaka T, Tanaka J, Kiyomatsu T et al (2015) The preoperative platelet to lymphocyte ratio is a prognostic marker in patients with stage II colorectal cancer. Int J Colorectal Dis 30(9):1165–1171
Author information
Authors and Affiliations
Contributions
We declare every author has actively participated in the drafting and design of this manuscript. We declare every author is pleased with the final version of this manuscript.
Corresponding author
Ethics declarations
Funding information
No funds or Grants have been provided.
Consent for publication
Every patient has given permission for publication of information from the medical history as long as it is used for medical research purposes.
Conflict of interest
The authors declare that they have no conflict of interest. No funds or grants have been provided.
Research involving human participants and/or animals
We have performed an observational retrospective study in which we have not modified the usual treatment of this disease, so disclosures about human research (in the sense of a clinical trial) are not applicable. No animal has been involved in this study.
Informed consent
Every patient has signed the informed consent for surgery. In addition, every patient has given permission for publication of information from the medical history as long as it is used for medical research purposes.
Rights and permissions
About this article
Cite this article
Bailon-Cuadrado, M., Choolani-Bhojwani, E., Tejero-Pintor, F.J. et al. Preoperative platelet–lymphocyte ratio is an independent factor of poor prognosis after curative surgery for colon cancer. Updates Surg 70, 33–39 (2018). https://doi.org/10.1007/s13304-017-0503-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-017-0503-3