Abstract
Introduction
Despite growing evidence that type 2 diabetes is associated with dementia, the question of whether intensive glucose control can prevent or arrest cognitive decline remains unanswered. In the analysis reported here, we explored the effect of intensive glucose control versus standard care on brain health, including structural abnormalities of the brain (atrophy, white matter hyperintensities, lacunar infarction, and cerebral microbleeds), cognitive dysfunction, and risk of dementia.
Methods
We searched the PubMed and Embase databases, the Web of Science website, and the Clinicaltrial.gov registry for studies published in English prior to July 2020. Only studies with a randomized controlled trial (RCT) design were considered. We analyzed structural abnormalities of the brain (atrophy, white matter hyperintensities, lacunar infarction, and cerebral microbleeds), cognitive function (cognitive impairment, executive function, memory, attention, and information-processing speed), and dementia (Alzheimer’s disease, vascular dementia, and mixed dementia).
Results
Six studies (5 different RCTs) with 16,584 participants were included in this meta-analysis. One study that compared structural changes between groups receiving intensive versus conventional glucose control measures reported non-significant results. The results of the five studies, comprising four cohorts, indicated a significantly poorer decline in cognitive function in the intensive glucose control group (β − 0.03, 95% confidence interval [CI] − 0.05 to − 0.02) than in the conventional glucose control group. Further subgroup analysis showed a significant difference in the change in cognitive performance in composite cognitive function (β − 0.03, 95% CI − 0.05 to − 0.01) and memory (β − 0.13, 95% CI − 0.25 to − 0.02). One trial evaluated the prevalence of cognitive impairment and dementia between groups receiving intensive and conventional glucose control, respectively, and the differences were insignificant.
Conclusion
This meta-analysis suggests that intensive glucose control in patients with type 2 diabetes can slow down cognitive decline, especially the decline in composite cognition and memory function. However, further studies are necessary to confirm the impact of strict glucose control on structural abnormalities in the brain and the risk of dementia.
Similar content being viewed by others
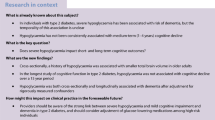
Why carry out this study? | |
Despite growing evidence that type 2 diabetes is associated with dementia, whether intensive glucose control can prevent or arrest the cognitive decline remains unknown. | |
This analysis was carried out with the aim to further explore the impact of intensive versus conventional glucose control on brain health. | |
What was learned from the study? | |
The results suggest that intensive glucose control in patients with type 2 diabetes can slow down cognitive decline, especially the decline in composite cognition and memory function. | |
However, further studies are necessary to confirm the impact of strict glucose control on structural abnormalities in the brain and the risk of dementia. |
Digital Features
This article is published with digital features, including a summary slide, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.13614653.
Introduction
Type 2 diabetes is a significant health challenge worldwide, and the prevalence of diabetes in adults is predicted to increase to 10.4% by 2040 [1]. Dementia and diabetes frequently coexist [2], with the prevalence of dementia being approximately 14% among people with diabetes aged more than 80 years [3]. Moreover, diabetes is a risk factor for cognitive dysfunction that can range from subtle diabetes-associated cognitive decline to pre-dementia and dementia [4]. The potential mechanisms of type 2 diabetes impacting brain health might be related to dysfunction of the inflammatory system [5], oxidative stress [6], and endothelial dysfunction [7], all of which are induced by both insulin resistance and elevated blood glucose levels. Previously published results show that fluctuations in blood glucose level have an effect on vascular complications [8, 9], which also impacts brain health. Thus, appropriate blood glucose control is vital for preserving brain health in patients with diabetes.
A number of cohort studies have focused on the differential impact of intensive and conventional blood glucose control on brain health, including structural abnormalities in the brain [10], cognitive dysfunction, and dementia [11]. Authors have suggested that cognitive functioning in patients with type 2 diabetes might benefit from several months of improved glycemic control [12, 13]. A recent meta-analysis indicated that people with type 2 diabetes performed better in processing speed and executive function but more poorly in memory and attention when on intensive glucose control regimes [14]. However, this analysis assessed the performance of the participants only at the end of the study.
The aim of the meta-analysis reported here was to further explore the impact of intensive versus conventional glucose control on brain health. Based on the previous studies, we focused not only on cognitive performance at the end of the study but also on cognitive change during the follow-up years, structural abnormalities of the brain, and the risk of dementia, as reported in randomized controlled studies.
Methods
Study Inclusion
The PubMed and Embase databases, the Web of Science website, and the Clinicaltrial.gov registry were searched for relevant studies published up to July 2020. Search terms used were “diabetes mellitus,” “hypoglycemic therapy” (including antidiabetic drugs, physical activity, and diet therapy), “brain structural abnormalities” (including brain atrophy, white matter hyperintensities, lacunar infarction, and cerebral microbleeds), “cognitive function” (including cognitive impairment, executive function, memory, attention, and information-processing speed), and “dementia” (including Alzheimer’s disease, vascular dementia, and mixed dementia), used alone and in combination. Further pertinent articles were supplemented by inspecting the references of the selected articles.
This report was conducted according to the Meta-analysis Of Observational Studies in Epidemiology [15] and the Preferred Reporting Items for Systematic Reviews and Meta-Analysis [16]. This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Inclusion and Exclusion Criteria
We included studies that met the following criteria: (1) original articles based on randomized controlled trials (RCTs) published in English; (2) study population comprised patients with type 2 diabetes; (3) at least one group of patients received intensive therapy and the other received conventional therapy to control blood glucose levels; (4) clear and consistent definitions of glucose level, brain structure abnormalities, and/or cognitive function or any type of dementia; and (5) data available on comparisons of brain health between the study groups receiving intensive and conventional glucose control therapy with more than a 1-year follow-up. Exclusion criteria were: (1) reviews, case reports, animal studies, or letter to the editor; (2) articles that did not clearly define clinical outcomes; (3) the author could not provide valid data when contacted; and (4) duplicated data.
The definition of “intensive therapy” was achieving glycated hemoglobin (HbA1c) of < 7% or a fasting glucose level of < 130 mg/dL. The format and content of the interventions could vary. For the current analysis, if articles provided data from the same cohort, we selected the cohort with the longest follow-up, largest sample size, and most comprehensive results. We analyzed the differences in brain structural abnormalities, cognitive dysfunction, and prevalence of dementia between the group receiving conventional glucose control and the one receiving intensive glucose control.
Data Extraction and Quality Assessment
The literature search was performed in July 2020. Two investigators (XYT, JBZ) independently extracted the data from the included studies, following identical standards on the study cohort, follow-up years, population characteristics, and outcomes. The risk of bias in selecting the included studies was assessed using the Newcastle–Ottawa Quality Assessment Scale (NOS) criteria [17]. Following the NOS guidelines, we rated the quality of the studies on the basis of selection, comparability, and outcome. In case of disagreement, the two investigators discussed the study with the other authors to arrive at a consensus.
Composite cognitive function was defined using the scores of the Mini-Mental State Examination (MMSE) [18] or the Comprehensive Assessment and Referral Evaluation-Diagnostic Scale [19]; memory was assessed using digit span scores [20] or Rey Auditory Verbal Learning Test scores [21]; attention and executive function were assessed using the scores of the Trail Making Test [22] or Stroop Test [23]; and information-processing speed was assessed using the Digit symbol substitution test scores [24]. Cognitive impairment was defined as a decline in cognitive function (decrease in the MMSE score by at least 3 points, compared to the baseline score) [11].
Statistical Analysis
Heterogeneity between the studies was evaluated using the I2 metric, and the variance between studies was evaluated using the Tau-squared (Tau2) metric. Random-effects models were selected if I2 > 50%, and fixed-effects models were chosen if I2 ≤ 0%. Data were obtained directly from the studies. Pooled differences in cognitive change during follow-up between the groups receiving intensive glucose control and those receiving conventional glucose control were performed using the β metric and the 95% confidence interval (CI). For the Stroop Test, a positive change in the value represents a worsening score; hence, we used the opposite number of the results. To identify additional potential factors impacting the bias, we also conducted a subgroup and sensitivity analysis. Sensitivity analyses were conducted to assess the influence of a single result on the pooled estimate. Egger’s asymmetry test was used to evaluate potential publication bias [25]. p values were two-tailed, and p < 0.05 was considered to be statistically significant. The statistical analyses were performed using STATA version 12.0 (Stata Corp., College Station, TX, USA).
Results
Literature Search Outcomes and Validity Assessment
The search strategy identified 8852 potentially relevant reports, of which 3220 were excluded due to duplication. The remaining 5632 articles were subjected to title and abstract screening, resulting in a further 5185 publications being excluded as they were reviews, letters or conference abstracts, and case reports. The remaining 447 articles were eligible for full-text review and data assessment. Of these, 441 articles were excluded for lack of relevant information or because they were based on animal studies. Ultimately, a total of six studies [10, 11, 26,27,28,29] with 16,584 participants met the inclusion criteria. The mean follow-up duration ranged from 3.5 to 10 years. The mean age of participants in the studies included in the current meta-analysis was 65.6 years at the initiation of the studies, and the proportion of women was 40.8% (Fig. 1). Table 1 shows the characteristics of the six included studies.
Quality Assessment
The NOS evaluation tool was used to assess the quality of the included studies. All quality assessment scores fell in the range of 8 or 9, indicating high quality (Table 2).
Structural Changes in the Brain Between Groups Receiving Intensive and Conventional Glucose Control
Only one cohort [10] study compared structural changes in the brain between groups receiving intensive and conventional glucose control, respectively. The Action to Control Cardiovascular Risk in Diabetes Memory in Diabetes (ACCORD MIND) trial, a sub-cohort of the ACCORD trial, comprised 614 patients with brain outcomes assessed by magnetic resonance imaging during 80 months of follow-up. The results showed that both the intensive and conventional glucose control groups had a decrease in total brain volume and an increase in abnormal white matter volume. Compared to the conventional glucose control group, the intensive glucose control group had a significantly slower decrease in total brain volume (4.6 cm3; 95% CI 2.0–7.3, p = 0.0006) at 40 months; however, there was no significant difference in the decrease in total brain volume between the groups at 80 months (0.2 cm3; 95% CI − 3.4–3.8, p = 0.91). The increase in log-transformed abnormal white matter volume at 40 months was significantly quicker in the intensive glucose control groups than that in the conventional glucose control groups (0.10; 95% CI 0.02–0.18, p = 0.014). However, at 80 months, there was no significant difference between the groups (0.05; 95% CI − 0.07 to 0.17, p = 0.41).
Change in Cognitive Function in the Intensive and Conventional Glucose Control Groups
Five studies [10, 26,27,28,29] comprising four cohorts, including the Informatics in Diabetes Education and Telemedicine Study, the Anglo-Danish–Dutch Study of Intensive Treatment in People with Screen-Detected Diabetes in Primary Care, the Veterans Affairs Diabetes Trial (VADT), and the ACCORD MIND trial, described the difference in the change in cognitive function between the groups receiving intensive glucose control and those receiving conventional glucose control. Since the cohorts in two studies were identical (ACCORDION MIND; [10, 26]), we selected the study with the longer follow-up period [10]. A total of 2751 patients who received intensive glucose control treatment and 2693 patients who received conventional glucose control treatment were included in this analysis. With the conventional glucose control group as a reference, the pooled results indicated a statistically significant slower decline in cognitive function in the intensive glucose control group (β − 0.03, 95% CI − 0.05 to − 0.02). Further subgroup analysis showed a significantly slower decline in the cognitive performance composite (β − 0.03, 95% CI − 0.05 to − 0.01) and memory (β − 0.13, 95% CI − 0.25 to − 0.02) in the intensive glucose control group; however, no difference in information-processing speed (β 0.09, 95% CI − 0.06 to 0.25) or attention and executive function (β − 0.14, 95% CI − 0.30–0.03) was seen between the groups (Fig. 2).
Difference in cognitive function change between groups receiving intensive glucose control and those receiving conventional glucose control. CI Confidence interval. I-squared is the variation in effect estimates attributable to heterogeneity, Overall refers to the pooled fixed effect estimate of all studies, and Subtotal is the fixed random effects estimate of the subgroup analysis studies. Weights are from the fixed-effects analysis, and %Weight is the weight assigned to each study, based on the inverse of the within- and between-study variance. The size of the gray boxes around the point estimates reflects the weight assigned to each study
The results of the meta-regression analyses suggested that differences in cognitive change between the two groups were not associated with sample size, number of follow-up years, mean age, and NOS scores (p > 0.05). After excluding studies one by one, the outcomes of the sensitivity analysis indicated that the results were stable. In the analysis of publication bias, the p value of the Egger test was > 0.05 (p = 0.74) for the difference in cognitive change between the intensive and conventional glucose control groups. The funnel figure of these studies showed no publication bias, having an asymmetrical inverted distribution, which is consistent with the results of the Egger test. (Fig. 3).
Difference in the Risk of Dementia Between the Intensive and Conventional Glucose Control Groups
Only one cohort [11], the Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation (ADVANCE) trial, measured the cognitive decline and risk of dementia between intensive and conventional glucose control groups. The trial included 5571 patients in the intensive control group and 5569 in the conventional control group with 8 years of follow-up. However, there was no significant difference in the cognitive impairment (risk ratio [RR] 0.98, 95% CI 0.90–1.07) and risk of dementia (RR 1.27, 95% CI 0.87–1.85) between the two groups. Further analysis of relative risk reduction also showed non-significant outcomes between the two groups in terms of cognitive impairment (2%; 95% CI − 7–11%) and risk of dementia (− 27%; 95% CI − 86–13%).
Discussion
A total of six studies involving five cohorts were included in our meta-analysis. We compared the impact of intensive and conventional glucose control on brain health, including brain structural abnormalities, cognitive change, and the risk of dementia. According to the pooled results, intensive glucose control can slow down the cognitive function—which declines with age—in terms of composite performance and memory, but not in terms of information-processing speed or attention and executive function. Although the impact of intensive glucose control on composite performance showed statistical significance, the rate of decline was minimal; hence, the results should be interpreted with caution. Therefore, more rigorous randomized controlled studies on the impact of intensive versus conventional glucose control on brain structural abnormalities and risk of dementia are needed.
A recent meta-analysis that included only three studies on type 2 diabetes compared the difference in the impact of intensive and conventional glucose control on cognitive performance among patients with diabetes [14]. The pooled analysis of these three studies, including 3200 individuals with type 2 diabetes, showed the benefits of intensive glucose control therapy on information-processing speed and executive functions, but no difference was observed on attention and memory. However, the sample size was small, and the analysis focused only on cognitive performance at the end of the follow-up period. The current meta-analysis had a larger sample size and analyzed the difference in impact between intensive and conventional glucose control on cognitive change during the follow-up period, brain structural abnormalities, and risk of dementia. We found that only one RCT reported a difference in total brain volume decline and an increase in abnormal white matter volume between the two groups; another study mentioned the risk of dementia.
There is evidence that in comparison to conventional glucose control, intensive glucose treatment measures increase the risk of severe hypoglycemia [30]. Overall mortality in the ACCORD and VADT studies was higher in the intensive glucose control group than in the conventional glucose control group, while in the ADVANCE study, the overall mortality was lower in the intensive than in the conventional treatment group [30]. Severe hypoglycemia is considered a risk factor for cognitive impairment [31] and mortality [32]. Nevertheless, the current analysis showed that intensive glucose control slowed the cognitive decline and might have more obvious benefits on cognitive performance.
Potential Mechanisms
Various mechanisms may have the potential to contribute to the association between elevated blood glucose levels, glucose variability, and brain health. Diabetes causes insulin resistance, imbalance in brain energy metabolism, changes in the regional cerebral blood flow, and osmotic effects on neurons, all of which damage brain health [33]. Insulin is one of the molecules that provides neuroprotection by regulating tau protein phosphorylation in the neurons and is crucial for the health of neuronal networks [34]. Insulin resistance may cause tau binding to microtubules, thus triggering the pathogenesis of cognitive decline and eventually leading to dementia [35]. Intensive glucose control can preserve insulin secretion and functional roles, which, in turn, improve neuronal functions. Another possible mechanism is that poor blood glucose control might lead to neuronal mitochondrial dysfunction and stress, DNA damage, and oxidative stress in endothelial cells [36, 37]. Thus, stricter management of blood glucose levels might decrease these risk factors, especially in those diagnosed with type 2 diabetes. However, a higher mortality and frequency of hypoglycemic events, both of which are threats to brain health, have been reported in patients treated with intensive glucose control measures [38]. Evidence has shown that insulin resistance might damage the brain structure, even in those without clinical diabetes [39], indicating that abnormal functioning of insulin signaling rather than blood glucose levels affect the cognitive impairment in patients with type 2 diabetes. Furthermore, the Diabetes Heart Study Mind provided neuroimaging data and revealed that the presence or absence of type 2 diabetes—but not HbA1c level—was independently associated with reduced white matter volume and reduced gray and white matter fractional anisotropy [40]. Thus, the influence of tighter glucose control on brain health (brain structural abnormalities, cognitive decline, and dementia prevalence) should be considered more cautiously.
Public Health Impact
With the rapid increase in aging populations worldwide, diabetes [41] and dementia [42] have become an increasing burden for society. Prevention and management of cognitive dysfunction and dementia are essential, especially in those diagnosed with diabetes. The benefits of intensive glucose control in preventing microvascular complications, such as diabetic retinopathy and diabetic kidney diseases, have been proven during a long-term follow-up study [43]. The results of the current meta-analysis indicate that intensive glucose control among patients with type 2 diabetes patients might slow down cognitive decline in composite and memory function. Better glucose control effectively prevents deterioration in brain health, which can help to avoid tremendous economic costs. However, hypoglycemia unawareness, significant comorbidities (risk factors of brain health), and mortality [44] caused by intensive glucose control treatment [45] suggest that more caution is necessary for prioritizing intensive glucose control as a general rule, particularly in elderly subjects. Therefore, an individualized approach seems the most reasonable strategy.
Strengths and Limitations of the Study
Although our meta-analysis considered the entire spectrum from pre-dementia to dementia and extracted valuable information regarding associations between intensive and conventional glucose control with brain health among patients with diabetes, its essential strengths and limitations merit mention. The strengths include choosing the strictest study design (RCT), developing a comprehensive search strategy, and conducting a comprehensive search. Some limitations warrant mention. The first is that only a few studies focused on the relationship between intensive and conventional glucose control with brain structural abnormalities and the risk of dementia. Second, the lack of information on the adverse effects of intensive glucose control, such as severe hypoglycemia, limited further analysis [46]. Third, some antidiabetic drugs had a different impact on cognitive impairment and dementia [47]; for example, glucagon-like peptide 1 analogs and sodium-dependent glucose transporter 2 inhibitors showed a protective effect [48, 49], while thiazolidinediones might have a negative impact [50]. However, the current analysis on this aspect was limited due to the lack of data. Fourth, the heterogeneity of the results; these might be due to differences in race, methods, and goals of intensive glucose control.
Conclusions
The current study suggests that intensive glucose control in persons with type 2 diabetes can slow down cognitive decline, especially the decline in composite and memory function. The impact of intensive glucose control on the brain structural abnormalities and risk of dementia needs further rigorously designed studies to validate our findings. Also, replicating and validating these findings is warranted.
References
Ogurtsova K, Da Rocha FJD, Huang Y, et al. IDF diabetes atlas: global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract. 2017;128:40–50.
Bunn F, Burn AM, Goodman C, et al. Comorbidity and dementia: a scoping review of the literature. BMC Med. 2014;12:192.
Wild S, Roglic G, Green A, et al. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27(5):1047–53.
Biessels GJ, Despa F. Cognitive decline and dementia in diabetes mellitus: mechanisms and clinical implications. Nat Rev Endocrinol. 2018;14(10):591–604.
Exalto LG, Whitmer RA, Kappele LJ, et al. An update on type 2 diabetes, vascular dementia and Alzheimer’s disease. Exp Gerontol. 2012;47(11):858–64.
Chang CM, Hsieh CJ, Huang JC, et al. Acute and chronic fluctuations in blood glucose levels can increase oxidative stress in type 2 diabetes mellitus. Acta Diabetol. 2012;49(Suppl 1):S171–7.
Wardlaw JM, Smith C, Dichgans M. Mechanisms of sporadic cerebral small vessel disease: insights from neuroimaging. Lancet Neurol. 2013;12(5):483–97.
Cavalot F, Petrelli A, Traversa M, et al. Postprandial blood glucose is a stronger predictor of cardiovascular events than fasting blood glucose in type 2 diabetes mellitus, particularly in women: lessons from the San Luigi Gonzaga Diabetes Study. J Clin Endocrinol Metab. 2006;91(3):813–9.
Zoppini G, Verlato G, Targher G, et al. Variability of body weight, pulse pressure and glycaemia strongly predict total mortality in elderly type 2 diabetic patients. The Verona Diabetes Study. Diabetes Metab Res Rev. 2008;24(8):624–8.
Murray AM, Hsu FC, Williamson JD, et al. ACCORDION MIND: results of the observational extension of the ACCORD MIND randomised trial. Diabetologia. 2017;60(1):69–80.
Kirkman MS, Mahmud H, Korytkowski MT. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes mellitus. Endocrinol Metab Clin N Am. 2018;47(1):81-+.
Naor M, Steingrüber HJ, Westhoff K, et al. Cognitive function in elderly non-insulin-dependent diabetic patients before and after inpatient treatment for metabolic control. J Diabetes Complicat. 1997;11(1):40–6.
Ryan CM, Freed MI, Rood JA, et al. Improving metabolic control leads to better working memory in adults with type 2 diabetes. Diabetes Care. 2006;29(2):345–51.
Peñaherrera-Oviedo C, Moreno-Zambrano D, Palacios M, et al. Does intensive glucose control prevent cognitive decline in diabetes? A meta-analysis. Int J Chronic Dis. 2015;2015:680104.
Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–12.
Knobloch K, Yoon U, Vogt PM. Preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement and publication bias. J Craniomaxillofac Surg. 2011;39(2):91–2.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5.
Folstein MF, Folstein SE, Mchugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98.
Gurland B, Kuriansky J, Sharpe L, et al. The Comprehensive assessment and Referral Evaluation (CARE)—rationale, development and reliability. Int J Aging Hum Dev. 1977;8(1):9–42.
Da W. Wechsler adult intelligence scale—revised UK. New York: Psychological Corporation; 1997.
Schmidt M. Rey auditory verbal learning test: a handbook. Los Angeles: Western Psychological Services; 1996.
Corrigan JD, Hinkeldey NS. Relationships between parts A and B of the Trail Making Test. J Clin Psychol. 1987;43(4):402–9.
Houx PJ, Jolles J, Vreeling FW. Stroop interference: aging effects assessed with the Stroop Color-Word Test. Exp Aging Res. 1993;19(3):209–24.
Silverstein AB. Two- and four-subtest short forms of the Wechsler Adult Intelligence Scale-Revised. J Consult Clin Psychol. 1982;50(3):415–8.
Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Launer LJ, Miller ME, Williamson JD, et al. Effects of intensive glucose lowering on brain structure and function in people with type 2 diabetes (ACCORD MIND): a randomised open-label substudy. Lancet Neurol. 2011;10(11):969–77.
Luchsinger JA, Palmas W, Teresi JA, et al. Improved diabetes control in the elderly delays global cognitive decline. J Nutr Health Aging. 2011;15(6):445–9.
Koekkoek PS, Ruis C, Van Den Donk M, et al. Intensive multifactorial treatment and cognitive functioning in screen-detected type 2 diabetes—the ADDITION-Netherlands study: a cluster-randomized trial. J Neurol Sci. 2012;314(1–2):71–7.
Zimering M B, Knight J, Ge L, et al. Predictors of cognitive decline in older adult type 2 diabetes from the veterans affairs diabetes trial. Front Endocrinol (Lausanne). 2016;7:123. https://doi.org/10.3389/fendo.2016.00123
Schernthaner G. Diabetes and cardiovascular disease: Is intensive glucose control beneficial or deadly? Lessons from ACCORD, ADVANCE, VADT, UKPDS, PROactive, and NICE-SUGAR. Wien Med Wochenschr. 1946;2010(160):8–19.
Mattishent K, Loke Y. Bi-directional interaction between hypoglycaemia and cognitive impairment in elderly patients treated with glucose-lowering agents: a systematic review and meta-analysis. Diabetes Obes Metab. 2016;18(2):135–41.
International Hypoglycaemia Study Group. Hypoglycaemia, cardiovascular disease, and mortality in diabetes: epidemiology, pathogenesis, and management. Lancet Diabet Endocrinol. 2019, 7(5):385–396.
Biessels GJ, Strachan MW, Visseren FL, et al. Dementia and cognitive decline in type 2 diabetes and prediabetic stages: towards targeted interventions. Lancet Diabetes Endocrinol. 2014;2(3):246–55.
Hölscher C. Novel dual GLP-1/GIP receptor agonists show neuroprotective effects in Alzheimer’s and Parkinson’s disease models. Neuropharmacology. 2018;136(Pt B):251–9.
Hong M, Lee VM. Insulin and insulin-like growth factor-1 regulate tau phosphorylation in cultured human neurons. J Biol Chem. 1997;272(31):19547–53.
Russo VC, Higgins S, Werther GA, et al. Effects of fluctuating glucose levels on neuronal cells in vitro. Neurochem Res. 2012;37(8):1768–82.
Schisano B, Tripathi G, Mcgee K, et al. Glucose oscillations, more than constant high glucose, induce p53 activation and a metabolic memory in human endothelial cells. Diabetologia. 2011;54(5):1219–26.
Jacobson AM, Musen G, Ryan CM, et al. Long-term effect of diabetes and its treatment on cognitive function. N Engl J Med. 2007;356(18):1842–52.
Willette A, Xu G, Johnson S, et al. Insulin resistance, brain atrophy, and cognitive performance in late middle-aged adults. Diabetes Care. 2013;36(2):443–9.
Raffield L, Cox A, Freedman B, et al. Analysis of the relationships between type 2 diabetes status, glycemic control, and neuroimaging measures in the Diabetes Heart Study Mind. Acta Diabetol. 2016;53(3):439–47.
Nanayakkara G, Kariharan T, Wang L, et al. The cardio-protective signaling and mechanisms of adiponectin. Am J Cardiovasc Dis. 2012;2(4):253–66.
Rizzi L, Rosset I, Roriz-Cruz M. Global epidemiology of dementia: Alzheimer’s and vascular types. Biomed Res Int. 2014;2014:908915.
Holman RR, Paul SK, Bethel MA, et al. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359(15):1577–89.
Rawlings AM, Sharrett AR, Mosley TH, et al. Glucose peaks and the risk of dementia and 20-year cognitive decline. Diabetes Care. 2017;40(7):879–86.
Terry T, Raravikar K, Chokrungvaranon N, et al. Does aggressive glycemic control benefit macrovascular and microvascular disease in type 2 diabetes? Insights from ACCORD, ADVANCE, and VADT. Curr Cardiol Rep. 2012;14(1):79–88.
Whitmer RA, Karter AJ, Yaffe K, et al. Hypoglycemic episodes and risk of dementia in older patients with type 2 diabetes mellitus. JAMA. 2009;301(15):1565–72.
Zhou J, Tang X, Han M, et al. Impact of antidiabetic agents on dementia risk: a Bayesian network meta-analysis. Metabolism. 2020;109:154265.
Bohlken J, Jacob L, Kostev K. Association between the use of antihyperglycemic drugs and dementia risk: a case-control study. J Alzheimer’s Dis. 2018;66(2):725–32.
Wium-Andersen I, Osler M, Jørgensen M, et al. Antidiabetic medication and risk of dementia in patients with type 2 diabetes: a nested case-control study. Eur J Endocrinol. 2019;181(5):499–507.
Cheng C, Lin C, Tsai Y, et al. Type 2 diabetes and antidiabetic medications in relation to dementia diagnosis. J Gerontol. 2014;69(10):1299–305.
Acknowledgements
Funding
This work was supported by the National Natural Science Foundation of China (No. 82070851, 81870556, 81930019), Beijing Municipal Administration of Hospital's Youth Program (QML20170204), Excellent Talents in Dongcheng District of Beijing. Capital's Funds for Health Improvement and Research (2020-1-1181). The Rapid Service Fee was funded by the authors.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
The authors are solely responsible for the design and conduct of this study, all study analyses, the drafting and editing of the manuscript, and its final contents. Xingyao Tang, Marly A. Cardoso, Jinkui Yang, Jian-Bo Zhou, and Rafael Simó have no disclosures to declare.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Data Availability
All data generated or analyzed during this study are included in this published article/as supplementary information files.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Tang, X., Cardoso, M.A., Yang, J. et al. Impact of Intensive Glucose Control on Brain Health: Meta-Analysis of Cumulative Data from 16,584 Patients with Type 2 Diabetes Mellitus. Diabetes Ther 12, 765–779 (2021). https://doi.org/10.1007/s13300-021-01009-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-021-01009-x